Abstract
Introduction
An algorithm to convert from any other opioid to oral levo-methadone was developed in Germany, the German model of levo-methadone conversion (GMLC). According to this GMLC, the pre-existing opioid is stopped, then titration of oral levo-methadone is initiated with a starting dose of 5 mg orally q 4 h (plus prn q 1 h). If necessary, levo-methadone dose is increased (pain) or decreased (side effects) by 30% q 4 h (plus prn q 1 h). After 72 h, the achieved single dose is maintained, but the dosing interval increases twofold to q 8 h (plus prn q 3 h). The aim of this study was to obtain information about the practicability, safety, and efficacy of the GMLC in clinical routine.
Methods
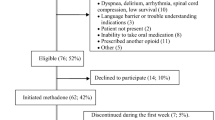
A retrospective, systematic chart review of levo-methadone conversions for the treatment of pain in inpatient palliative care was performed.
Results
Fifty-two patients were analyzed. The dosing interval was increased correctly after 72 h as demanded by the GMLC in 60% of patients. In 85% of the patients, opioid medication with levo-methadone could be maintained until the end of the inpatient stay. In three patients (6%), levo-methadone administration had to be stopped due to side effects. No serious adverse events could be detected during opioid rotation. Pain intensity was reduced significantly (p < 0.001) after conversion concerning mean (NRS 0.9; range 0–4) and maximum pain over the day (NRS 3.9; range 0–10).
Conclusion
The presented study indicates that the GMLC provides a practical and reasonably safe approach to perform opioid rotation to levo-methadone in a palliative care setting.


Similar content being viewed by others
References
Ansermot N, Albayrak O, Schlapfer J, Crettol S, Croquette-Krokar M, Bourquin M, Deglon JJ, Faouzi M, Scherbaum N, Eap CB (2010) Substitution of (R, S)-methadone by (R)-methadone: impact on QTc interval. Arch Intern Med 170:529–536
Bausewein C, Remi C, Twycross R, Wilcock A (2005) Arzneimitteltherapie in der Palliativmedizin. Urban & Fischer Verlag, München
Benitez-Rosario MA, Salinas-Martin A, Aguirre-Jaime A, Perez-Mendez L, Feria M (2009) Morphine-methadone opioid rotation in cancer patients: analysis of dose ratio predicting factors. J Pain Symptom Manage 37:1061–1068
Bruera E, Pereira J, Watanabe S (1996) Opioid rotation in patients with cancer pain: a retrospective comparison of dose ratios between methadone, hydromorphone, and morphine. Cancer 78:852–857
Bruera E, Sweeney C (2002) Methadone use in cancer patients with pain: a review. J Palliat Med 5:127–138
Davis MP, Walsh D (2001) Methadone for relief of cancer pain: a review of pharmacokinetics, pharmacodynamics, drug interactions and protocols of administration. Support Care Cancer 9:73–83
Foley KM (2003) Opioids and chronic neuropathic pain. N Engl J Med 348:1279–1281
Gaertner J, Voltz R, Ostgathe C (2008) Methadone: a closer look at the controversy. J Pain Symptom Manage 36:e4–e7
Klepstad P, Kaasa S, Cherny N, Hanks G, de Conno F (2005) Pain and pain treatments in European palliative care units. A cross sectional survey from the European Association for Palliative Care Research Network. Palliat Med 19:477–484
Krantz MJ, Mehler PS (2006) QTc prolongation: methadone's efficacy-safety paradox. Lancet 368:556–557
Lin C, Somberg T, Molnar J, Somberg J (2009) The effects of chiral isolates of methadone on the cardiac potassium channel IKr. Cardiol 113:59–65
Mancini I, Lossignol DA, Body JJ (2000) Opioid switch to oral methadone in cancer pain. Curr Opin Oncol 12:308–313
Morley JS, Makin MK (1998) The use of methadone in cancer pain poorly responsive to other opioids. Pain Reviews 5:51–58
Nauck F, Ostgathe C, Dickerson ED (2001) A German model for methadone conversion. Am J Hosp Palliat Care 18:200–202
Nauck F, Ostgathe C, Klaschik E, Bausewein C, Fuchs M, Lindena G, Neuwohner K, Schulenberg D, Radbruch L (2004) Drugs in palliative care: results from a representative survey in Germany. Palliat Med 18:100–107
Ostgathe C, Gaertner J, Nauck F, Voltz R (2008) High dose levo-methadone treatment for cancer pain in a patient with a history of drug addiction. J Pain Symptom Manage 35:229–231
Ostgathe C, Radbruch L, Nauck F, Elsner F (2007) Cancer pain management. Zeitschrift für Palliativmedizin 8:13–30
Pollock AB, Tegeler ML, Morgan V, Baumrucker SJ (2011) Morphine to methadone conversion: an interpretation of published data. Am J Hosp Palliat Care 28:135–140
Ripamonti C, Dickerson ED (2001) Strategies for the treatment of cancer pain in the new millennium. Drugs 61:955–977
Ripamonti C, Groff L, Brunelli C, Polastri D, Stavrakis A, De Conno F (1998) Switching from morphine to oral methadone in treating cancer pain: what is the equianalgesic dose ratio? J Clin Oncol 16:3216–3221
Ripamonti C, Groff L, Brunelli C, Polastri D, Stravakis A, De Conno F (1998) Switching from morphine to oral methadone in treating cancer pain. What is the equianalgesic dose ratio? J Clin Oncol 16(10):3216–3221
Tse DM, Sham MM, Ng DK, Ma HM (2003) An ad libitum schedule for conversion of morphine to methadone in advanced cancer patients: an open uncontrolled prospective study in a Chinese population. Palliat Med 17:206–211
Watanabe S (2001) Methadone: the renaissance. J Palliat Care 17:117–120
Weschules DJ, Bain KT (2008) A systematic review of opioid conversion ratios used with methadone for the treatment of pain. Pain Med 9:595–612
Acknowledgement
The scientific work of the Division of Palliative Medicine, Erlangen, and the departments of Palliative Medicine in Cologne and Goettingen are substantially supported by the German Cancer Aid (Deutsche Krebshilfe e.V.). The scientific work of the Department of Palliative Medicine, University Clinic of Cologne is supported by the Federal Ministry for Education and Science (BMBF 01KN0706).
Conflict of interest
Christoph Ostgathe receives remuneration from Mundipharma, Nycomed, Grünenthal and Cephalon and funding from Mundipharma. Raymond Voltz receives remuneration from Mundipharma, Cephalon and Lilly and funding from Mundipharma and Cephalon. Rainer Sabatowski receives remuneration from Grünenthal, Nycomed, MSD and Janssen-Cilag and is advisor for Cephalon. Friedemann Nauck receives remuneration from Mundipharma, Cephalon, Archimedes, Nycomed and Sanovi Aventis and funding from Sanofi Aventis. Jan Gärtner receives remuneration from Mundipharma, Cephalon, Pfizer and Archimedes and funding from Mundipharma and Cephalon. The authors declare to have no conflicts of interest regarding this study and that they have full control of all primary data. They agree to allow the journal to review their data if requested.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ostgathe, C., Voltz, R., Van Aaaken, A. et al. Practicability, safety, and efficacy of a “German model” for opioid conversion to oral levo-methadone. Support Care Cancer 20, 2105–2110 (2012). https://doi.org/10.1007/s00520-011-1320-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-011-1320-8