Abstract
Purpose
The control of nausea and vomiting induced by chemotherapy is paramount for overall treatment success in cancer patients. Antiemetic therapy during chemotherapy in lymphoma patients generally consists of anti-serotoninergic drugs and dexamethasone. The aim of this trial was to evaluate the efficacy of a single dose of palonosetron, a second-generation serotonin type 3 (5-HT3) receptor antagonist, in patients with aggressive non-Hodgkin's lymphoma receiving moderately emetogenic chemotherapy (MEC) containing steroids.
Methods
Patients received a single intravenous bolus of palonosetron (0.25 mg) before administration of chemotherapy. Complete response (CR) defined as no vomiting and no rescue therapy during overall phase (0–120 h) was the primary endpoint. Complete control (CC) defined as CR and only mild nausea was a secondary endpoint.
Results
Eighty-six evaluable patients entered in the study. A CR was observed in 74 patients (86.0%) during the overall phase; the CR during the acute (0–24 h) and delayed (24–120 h) phases was 90.7% and 88.4%, respectively. CC was 89.5% during the acute and 84.9% during the delayed phase; the overall CC was 82.6%.
Conclusions
This was the first trial, which demonstrated the efficacy of a single dose of palonosetron in control CINV in patients with aggressive non-Hodgkin’s lymphoma receiving MEC regimen containing steroids.
Similar content being viewed by others
Introduction
Although chemotherapy-induced nausea and vomiting (CINV) are not life-threatening adverse events, they can nevertheless adversely affect the quality of life, and thus control of CINV plays a key role in the treatment of cancer patients undergoing chemotherapy. Antiemetic guidelines [1–3] have defined the emetic risk of antineoplastic agents [4] as high (>90% emetic risk), moderate (30–90%), low (10–30%), and minimal (<10%), the figures in parentheses representing the percentage of patients having emetic episode(s) when no prophylactic antiemetic protection provided. CINV prophylaxis for highly emetogenic chemotherapy (HEC) includes a three-drug regimen: a 5-HT3 receptor antagonist (5-HT3RA), dexamethasone and a neurokinin-1 (NK-1) receptor antagonist; for moderately emetogenic chemotherapy (MEC), standard prophylaxis includes a two-drug regimen: a 5-HT3RA and dexamethasone or methyl-prednisone, both given on the day of chemotherapy, with the administration of either dexamethasone or a 5-HT3RA for 3-4 days after treatment. Currently, standard antiemetic therapy in patients with lymphomas undergoing MEC is a combination therapy with a 5-HT3RA and steroids [5].
The first generation 5-HT3RAs (ondansetron, granisetron, dolasetron, and tropisetron) have demonstrated considerable efficacy in preventing acute (0–24 h after chemotherapy) CINV which is mostly serotonin related, but there is no clinical evidence to justify their use beyond 24 h after chemotherapy for prevention of delayed (24–120 h after chemotherapy), in part substance P-related, emesis [6]. Palonosetron is a second-generation 5-HT3RA, and is approved by FDA for treatment of delayed emesis [7]. The characteristics of palonosetron distinguish it from other 5-HT3RAs [7, 8]. In particular, it has a prolonged half-life (∼40 h) and a high binding affinity (approximately 2,500-fold higher than that of serotonin), in addition showing allosteric interactions and positive cooperativity with the 5-HT3 receptor [9, 10]. The actual role of palonosetron in comparison with the other available 5-HT3RAs is discussed controversially in all three main antiemetic guidelines. There is some evidence that palonosetron may be superior to first generation 5-HT3RAs in providing control of both nausea and vomiting in patients undergoing either MEC or HEC [11–15]. Due to its unique pharmacological characteristics [7–10], palonosetron can protect patients from CINV during the overall emetic risk period after chemotherapy (0–120 h), even when employed without corticosteroids.
The aim of this multicentre, open-label, non-randomized, phase II study was to evaluate the efficacy and safety of a single intravenous bolus of palonosetron (0.25 mg) for the prevention of CINV during 5 days post-chemotherapy in patients with aggressive non-Hodgkin's lymphoma (NHL) treated with anthracycline-containing regimens.
Patients and methods
This study (EudraCT number 2006-003189-33, NCT number 01018758) was conducted according to the Declaration of Helsinki and Good Clinical Practice guidelines. The study protocol was approved by local ethics committees, and all patients gave written informed consent to participate before study entry. Patients with histologically or cytologically confirmed aggressive NHL, at any stage, were eligible. Patients were required to be >18 years of age, with an Eastern Cooperative Oncology Group performance status of zero to one and acceptable hepatic and renal functions, scheduled to receive at least one moderately emetogenic agent on day 1, according to the modified Hesketh classification [4, 16]. Patients with diagnosis of Hodgkin's lymphoma or leukemia, and candidates for multiple day/high-dose chemotherapy or bone marrow/peripheral blood stem cell transplantation were excluded.
Treatment plan
Patients received a single intravenous bolus of palonosetron (0.25 mg), over 30 s, beginning 30 min before chemotherapy on day 1. Patients were assessed from day 1 throughout day 5 after the start of chemotherapy, and the antiemetic response was evaluated during the acute, delayed and overall phases, as well on each day.
Patients were followed for safety and tolerability, and adverse events were considered by the investigator to be possibly, probably or definitely related to study medication until the start of the next chemotherapy cycle. Patients were asked to fill in a diary beginning on day 1 until day 5, reporting the occurrence and severity of emesis and nausea episodes, as well as the use of rescue medication. At the end of the study, patient global satisfaction with antiemetic therapy was measured using a visual analogue scale (VAS). After chemotherapy, rescue medication including dexamethasone and/or metoclopramide for nausea and vomiting was permitted upon request of the patient and recorded in patient's diary.
Study endpoints and assessments
The primary endpoint was the overall rate of patients achieving a complete response (CR), defined as no emetic episodes and no use of rescue medication during the overall phase. Secondary endpoints were evaluated during the acute, delayed and overall phases and included CR rate during the acute and delayed phases, rate of complete control (CC; defined as CR with a maximum grade of mild nausea), percentage of patients experiencing emesis and nausea (severity graded according to Likert scale), patient global satisfaction with antiemetic therapy, as measured by VAS, and safety profile of palonosetron. Severity of nausea was graded according to Likert scale: 0-none, 1-mild; 2-moderate; 3-severe, according to subjective assessment by each patient.
Statistical analysis
The efficacy of palonosetron was evaluated upon a one-stage Fleming study design for determination of response rates based on a single treatment group [17].
A sample size of 77 patients was estimated using the exact method (binomial) and assuming that π = 20 (null hypothesis) is the largest value for the proportion of responders for which the treatment is considered ineffective, and π = 35 (alternative hypothesis) the smallest value for the proportion of responders for which the treatment is considered effective, with a probability of type 1 error equal to 0.05 (one-tail), and a power of 90%. Eighty-five patients were planned for enrolment, considering a loss of 10% (lost to follow-up, withdrawal of informed consent, administrative reasons). The safety cohort included all patients who received at least one dose of the study medication after registration.
Results
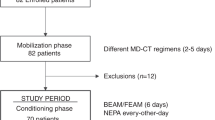
Between June 2006 and July 2008, a total of 91 patients with NHL were prospectively recruited by ten Italian centers belonging to the Gruppo Italiano per lo Studio dei Linfomi (GISL). Five patients were considered not eligible: four were low grade NHL and one patient had an ECOG = 3. Demographic and baseline data of the 86 evaluable patients are shown in Table 1. The majority of patients had diffuse large B cell lymphoma (77.9%), stage III and IV disease (67.4%) and received CHOP+/−R (cyclophosphamide, doxorubicin, vincristine and prednisone, ± rituximab) chemotherapy (74.4%).
Efficacy
Regarding the primary endpoint, CR was observed in 74 of 86 patients (86.0%) during the overall phase. CR during the acute and delayed phases was 90.7% and 88.4% (Fig. 1), respectively. The CC was 89.5% during the acute and 84.9% during the delayed phase was; the overall CC was 82.6% (Table 2). Table 2 shows the proportion of patients who did not experience both emesis and nausea, during the delayed and overall phases and on individual days. During the overall study period, the emesis-free rate was 88.4%, while the nausea-free rate was 74.4%; no patient experienced severe nausea. The median patient global satisfaction with antiemetic therapy was 8.0 (range, 1–10).
Tolerability
Palonosetron was well tolerated and no patient experienced a severe adverse event. The most common grade 1–2 adverse events were constipation (7.0%), headache (5.8%), asthenia (7.0%) and dizziness (1.2%). No grade 3 and 4 adverse events and no significant changes in laboratory tests or vital signs were observed during the study period.
Discussion
The results of this multicentre clinical trial demonstrate that a single dose of palonosetron (0.25 mg) before chemotherapy, without supplementing with additional dexamethasone, is effective and well tolerated by patients with aggressive NHL treated with MEC. Uncontrolled emesis associated with chemotherapy is sometimes such a negative experience that it may even lead to refusal by the patient to undergo potentially life-saving treatments for their malignancy [18, 19]. Currently, antiemetic guidelines [1–3] for MEC suggest the use of a 5-HT3RA and dexamethasone on day 1, followed by dexamethasone on days 2 and 3 to prevent delayed CINV. This recommendation stems from clinical evidence showing that corticosteroids increase the effect of other antiemetics [20] such as low-dose and high-dose metoclopramide [21], first generation 5-HT3RAs [22, 23], and a NK-1 receptor antagonist [24, 25]. Clinicians, however, have some concerns about the use of dexamethasone in clinical practice because of its potential side effects [5]. Palonosetron, due to its unique pharmacological characteristics [6–10], may be of benefit in avoiding or minimizing the use of steroids [26, 27].
Two previous studies have assessed the efficacy of first generation 5-HT3RA (ondansetron and granisetron) in malignant lymphoma patients undergoing CHOP like chemotherapy: one study [28] compared ondansetron and metoclopramide, while Numbenjapon et al. compared granisetron (GRAN) and metoclopramide [29], both combined with corticosteroid (CS). Antiemetic prophylaxis in the OND study was: OND 8 mg/methylprednisolone 80 mg i.v. before chemotherapy and OND 8 mg p.o. after 8 h and at bedtime. OND 8 mg tid days 2–3, and 8 mg tid prn days 4–5, and prednisolone 75–100 mg qds days 2–5. In the acute phase, no emesis was registered in 92%, and no nausea in 79% of the OND/CS-treated group. The ultimate aim—neither nausea nor emesis—was reached in 77% of OND/CS-treated patients. The control of delayed nausea was obtained in 81% of patients [28]. Antiemetic prophylaxis in the Numbenjapon study [29] was GRAN 1 mg with 8 mg dexamethasone before chemotherapy and GRAN 1 mg daily on days 2–5. In the acute phase patients achieved a control response of 87.5% during the acute phase and 95.8% during the delayed phase.
In the present trial, most patients were treated with CHOP+/−R (cyclophosphamide 750 mg/sqm i.v., doxorubicin 50 mg/sqm i.v. and vincristine 1.4 mg/sqm i.v. on day 1, prednisone 100 mg daily o.s. for 5 days ±/− rituximab 375 mg/sqm i.v. on day 1), which is considered the standard of care for aggressive NHL patients [30]. With a similar chemotherapeutic regimen, the GELA (Groupe d'Etude des Lymphomes de l'Adulte) trial [30], which assessed the additional of rituximab to the CHOP regimen, has shown an incidence of nausea and vomiting of any grade of 40–48%, with 4–8% of grades 3–4. In our trial, the incidence of nausea of any grade ranged from 4.7% to 18.6%, and the rate of vomiting of any grade ranged from 0% to 8.1% during the 5 days of observation. It is also worthwhile noting that this population is younger and at a higher risk of emesis, than that of the GELA trial. The primary endpoint of our study was reached since 86.0% of patients achieved a CR during the overall study period. The secondary endpoints were also met as the percentage of CC in the acute and late phases was 89.5% and 84.9%, respectively.
Palonosetron was well tolerated and the incidence and severity of adverse events were low. The modality of administration by bolus infusion over 30″, differently than first generation 5-HT3RAs, allows to reduce the overall treatment time and the staff costs. Finally, the antiemetic efficacy being equal, a single dose of palonosetron is less expensive than several infusions of first generation antagonists. The weakness of our study is absence of dexamethasone-containing control arm, but recent randomized trials [31, 32] have investigated if the use of palonosetron might provide the opportunity to reduce the total corticosteroid dose with no loss of efficacy in delayed MEC, in patients receiving chemotherapeutic regimens which don’t include steroid administration.
Both studies demonstrated that a reduced dexamethasone dosing regimen offers high and similar protection as 3-day dosing, as demonstrated by the equivalent complete response rates in the 5-day observation interval [31, 32].
This was the first trial, which demonstrated the efficacy of a single dose of palonosetron in control CINV in patients receiving MEC regimen containing steroids.
References
Herrstedt J (2008) Antiemetics: an update and the MASCC guidelines applied in clinical practice. Nat Clin Pract Oncol 5(1):32–43
Kris MG, Hesketh PJ, Somerfield MR et al (2006) American Society of Clinical Oncology guideline for antiemetics in oncology: update 2006. J Clin Oncol 24(18):2932–2947
Roila F, Hesketh PJ, Herrstedt J (2006) Prevention of chemotherapy- and radiotherapy-induced emesis: results of the 2004 Perugia International Antiemetic Consensus Conference. Ann Oncol 17(1):20–28
Grunberg SM, Osoba D, Hesketh PJ et al (2005) Evaluation of new antiemetic agents and definition of antineoplastic agent emetogenicity—an update. Support Care Cancer 13(2):80–84
Vardy J, Chiew KS, Galica J et al (2006) Side effects associated with the use of dexamethasone for prophylaxis of delayed emesis after moderately emetogenic chemotherapy. Br J Cancer 94(7):1011–1015
Geling O, Eichler HG (2005) Should 5-hydroxytryptamine-3 receptor antagonists be administered beyond 24 hours after chemotherapy to prevent delayed emesis? Systematic re-evaluation of clinical evidence and drug cost implications. J Clin Oncol 23(6):1289–1294
Siddiqui MA, Scott LJ (2004) Palonosetron Drugs 64(10):1125–1132, discussion 1133-4
Wong EH, Clark R, Leung E et al (1995) The interaction of RS 25259-197, a potent and selective antagonist, with 5-HT3 receptors, in vitro. Br J Pharmacol 114(4):851–859
Rojas C, Stathis M, Thomas AG et al (2008) Palonosetron exhibits unique molecular interactions with the 5-HT3 receptor. Anesth Analg 107(2):469–478
Rojas C, Thomas AG, Alt J et al (2009) Palonosetron triggers 5-HT(3) receptor internalization and causes prolonged inhibition of receptor function. Eur J Pharmacol 626(2–3):193–199
Aapro MS, Grunberg SM, Manikhas GM et al (2006) A phase III, double-blind, randomized trial of palonosetron compared with ondansetron in preventing chemotherapy-induced nausea and vomiting following highly emetogenic chemotherapy. Ann Oncol 17(9):1441–1449
Eisenberg P, Figueroa-Vadillo J, Zamora R et al (2003) Improved prevention of moderately emetogenic chemotherapy-induced nausea and vomiting with palonosetron, a pharmacologically novel 5-HT3 receptor antagonist: results of a phase III, single-dose trial versus dolasetron. Cancer 98(11):2473–2482
Gralla R, Lichinitser M, Van Der Vegt S et al (2003) Palonosetron improves prevention of chemotherapy-induced nausea and vomiting following moderately emetogenic chemotherapy: results of a double-blind randomized phase III trial comparing single doses of palonosetron with ondansetron. Ann Oncol 14(10):1570–1577
Rubenstein E, Gralla R, Eisenberg P, et al (2003) Palonosetron (PALO) compared with ondansetron (OND) or dolasetron (DOL) for prevetion of acute and delayed chemotherapy-induced nausea and vomiting (CINV). Combined results of two phase III trials. In: Proc Am Soc Clin Oncol 22: (abstr 2932)
Saito M, Aogi K, Sekine I et al (2009) Palonosetron plus dexamethasone versus granisetron plus dexamethasone for prevention of nausea and vomiting during chemotherapy: a double-blind, double-dummy, randomised, comparative phase III trial. Lancet Oncol 10(2):115–124
Hesketh PJ, Kris MG, Grunberg SM et al (1997) Proposal for classifying the acute emetogenicity of cancer chemotherapy. J Clin Oncol 15(1):103–109
Fleming TR (1982) One-sample multiple testing procedure for phase II clinical trials. Biometrics 38(1):143–151
Hesketh PJ (2008) Chemotherapy-induced nausea and vomiting. N Engl J Med 358(23):2482–2494
Sharma R, Tobin P, Clarke SJ (2005) Management of chemotherapy-induced nausea, vomiting, oral mucositis, and diarrhoea. Lancet Oncol 6(2):93–102
Herrstedt J, Aapro MS, Smyth JF et al (1998) Corticosteroids, dopamine antagonists and other drugs. Support Care Cancer 6(3):204–214
Allan SG, Cornbleet MA, Warrington PS et al (1984) Dexamethasone and high dose metoclopramide: efficacy in controlling cisplatin induced nausea and vomiting. Br Med J (Clin Res Ed) 289(6449):878–879
The Italian Group for Antiemetic Research (1995) Dexamethasone, granisetron, or both for the prevention of nausea and vomiting during chemotherapy for cancer. N Engl J Med 332(1):1–5
Roila F, Tonato M, Cognetti F et al (1991) Prevention of cisplatin-induced emesis: a double-blind multicenter randomized crossover study comparing ondansetron and ondansetron plus dexamethasone. J Clin Oncol 9(4):675–678
Hesketh PJ, Grunberg SM, Gralla RJ et al (2003) The oral neurokinin-1 antagonist aprepitant for the prevention of chemotherapy-induced nausea and vomiting: a multinational, randomized, double-blind, placebo-controlled trial in patients receiving high-dose cisplatin--the Aprepitant Protocol 052 Study Grou. J Clin Oncol 21(22):4112–4119
Warr DG, Hesketh PJ, Gralla RJ et al (2005) Efficacy and tolerability of aprepitant for the prevention of chemotherapy-induced nausea and vomiting in patients with breast cancer after moderately emetogenic chemotherapy. J Clin Oncol 23(12):2822–2830
Giuliani F, Cilenti G, Nugnes I, et al (2008) Palonosetron for prevention of acute and delayed nausea and vomiting induced by moderately emetogenic adjuvant FOLFOX-4 regimen in colorectal cancer (CRC) patients: a phase II study of the Gruppo Oncologico dell'Italia Meridionale (GOIM). In: Eur J Cancer Supplements
Aapro MS (2007) Palonosetron as an anti-emetic and anti-nausea agent in oncology. Ther Clin Risk Manag 3(6):1009–1020
Jorgensen M, Victor MA (1996) Antiemetic efficacy of ondansetron and metoclopramide, both combined with corticosteroid, in malignant lymphoma patients receiving non-cisplatin chemotherapy. Acta Oncol 35(2):159–163
Numbenjapon T, Sriswasdi C, Mongkonsritragoon W et al (2002) Comparative study of low-dose oral granisetron plus dexamethasone and high-dose metoclopramide plus dexamethasone in prevention of nausea and vomiting induced by CHOP-therapy in young patients with non-Hodgkin's lymphoma. J Med Assoc Thai 85(11):1156–1163
Coiffier B, Lepage E, Briere J et al (2002) CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346(4):235–242
Aapro M, Fabi A, Nole F et al (2010) Double-blind, randomised, controlled study of the efficacy and tolerability of palonosetron plus dexamethasone for 1 day with or without dexamethasone on days 2 and 3 in the prevention of nausea and vomiting induced by moderately emetogenic chemotherapy. Ann Oncol 21(5):1083–1088
Celio L, Frustaci S, Denaro A, et al (2010) Palonosetron in combination with 1-day versus 3-day dexamethasone for prevention of nausea and vomiting following moderately emetogenic chemotherapy: a randomized, multicenter, phase III trial. Support Care Cancer
Acknowledgements
The authors thank the patients, nurses and data managers who participated in this trial. They also thank Italfarmaco S.p.A. for providing palonosetron.
Conflicts of interest
The authors indicated no potential conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Di Renzo, N., Montanini, A., Mannina, D. et al. Single-dose palonosetron for prevention of chemotherapy-induced nausea and vomiting in patients with aggressive non-Hodgkin's lymphoma receiving moderately emetogenic chemotherapy containing steroids: results of a phase II study from the Gruppo Italiano per lo Studio dei Linfomi (GISL). Support Care Cancer 19, 1505–1510 (2011). https://doi.org/10.1007/s00520-010-0974-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00520-010-0974-y