Summary
Objective
The low-density lipoprotein cholesterol goals in the 2019 European Society of Cardiology/European Atherosclerosis Society dyslipidaemia guidelines necessitate greater use of combination therapies. We describe a real-world cohort of patients in Austria and simulate the addition of oral bempedoic acid and ezetimibe to estimate the proportion of patients reaching goals.
Methods
Patients at high or very high cardiovascular risk on lipid-lowering treatments (excluding proprotein convertase subtilisin/kexin type 9 inhibitors) from the Austrian cohort of the observational SANTORINI study were included using specific criteria. For patients not at their risk-based goals at baseline, addition of ezetimibe (if not already received) and subsequently bempedoic acid was simulated using a Monte Carlo simulation.
Results
A cohort of patients (N = 144) with a mean low-density lipoprotein cholesterol of 76.4 mg/dL, with 94% (n = 135) on statins and 24% (n = 35) on ezetimibe monotherapy or in combination, were used in the simulation. Only 36% of patients were at goal (n = 52). Sequential simulation of ezetimibe (where applicable) and bempedoic acid increased the proportion of patients at goal to 69% (n = 100), with a decrease in the mean low-density lipoprotein cholesterol from 76.4 mg/dL at baseline to 57.7 mg/dL overall.
Conclusions
The SANTORINI real-world data in Austria suggest that a proportion of high and very high-risk patients remain below the guideline-recommended low-density lipoprotein cholesterol goals. Optimising use of oral ezetimibe and bempedoic acid after statins in the lipid-lowering pathway could result in substantially more patients attaining low-density lipoprotein cholesterol goals, likely with additional health benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) remains the leading cause of death in Europe, with more than 4 million associated deaths every year [1]. Aside from increased mortality, CVD is a major cause of disability [2, 3] and reduced quality of life [4] and is associated with poor clinical outcomes [2, 3]. As well as impacting patients, CVD causes considerable economic burden with direct healthcare costs amounting to €111 billion per year in Europe [2]. Increased low-density lipoprotein cholesterol (LDL-C) is widely accepted as a proven and direct cause of atherosclerotic CVD [1, 5,6,7] and its major clinical sequelae [5, 8]. Each 1 mmol/L (38.67 mg/dL) LDL‑C reduction corresponds to an approximately 20% proportional risk reduction in atherosclerotic CVD events and 10% reduction in all-cause mortality [1, 5, 9], independently of the LDL‑C lowering mechanism [10,11,12,13].
Although there are well-established lipid-lowering therapies (LLTs), treatment recommendations, and risk-based goals for LDL‑C lowering in Europe [1], the population-level achievement of LDL‑C goals is limited by barriers such as statin intolerance, the limited efficacy of ezetimibe, and the cost and restricted reimbursement of proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors [14,15,16]. In a European multinational (18 countries) observational study (DA VINCI), the risk-based LDL‑C goal defined by the 2019 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) guidelines was achieved in only 33% of patients prescribed LLT for primary or secondary prevention in primary or secondary care [17]. Similar findings were reported for the Austrian cohort of the DA VINCI study [18]. Many patients in routine clinical practice remain suboptimally treated and thus at increased cardiovascular (CV) risk; as a result, they need intensification of LLT for further LDL‑C lowering. Statins plus ezetimibe will only achieve LDL‑C goals on average in about 40–45% of high and very high risk patients, meaning that at least one third of these patients will require use of additional oral therapy or injectable PCSK9 inhibitor [6, 15, 17, 19,20,21] or inclisiran.
Bempedoic acid is a first-in-class, adenosine triphosphate citrate lyase (ACL) inhibitor, once daily, oral LDL‑C lowering treatment that can be combined with other LLTs in patients with hypercholesterolaemia (heterozygous familial and nonfamilial) or mixed dyslipidaemia who, despite current oral LLTs, are not reaching their therapeutic goals [22,23,24,25].
Bempedoic acid and its fixed-dose combination with ezetimibe were approved by the European Medicines Agency based on pivotal randomised controlled phase 3 trials in a spectrum of patients receiving maximum-tolerated statin dose (CLEAR Harmony [25], CLEAR Wisdom [23], and a fixed-dose combination study (1002FDC-053; [26])) and patients receiving no or low-dose statin (CLEAR Serenity [24] and CLEAR Tranquility [22]).
Bempedoic acid has been endorsed in consensus statements and scientific society guidance, which reinforce that it is an affordable oral treatment option that is easy to use and suitable for people who are not at goal with existing lipid-lowering treatments [6, 27,28,29].
This analysis aimed (1) to estimate the proportion of patients within an Austrian real-world cohort who would need additional oral LLT according to the 2019 ESC/EAS dyslipidaemia guidelines and (2) to simulate the effects of intensifying lipid-lowering therapy by addition of ezetimibe and bempedoic acid on attainment of LDL‑C goals.
Patients, materials and methods
SANTORINI patient cohort
The SANTORINI study (NCT04271280) is a multinational, multicentre, non-interventional, prospective, observational study, designed to describe how LLTs are used in the real world and to what extent these approaches achieve guideline recommendations [6, 30]. Patients with high or very high CV risk according to the investigator’s assessment were included in 14 European countries and were treated with LLT according to routine clinical practice. Aggregate baseline data from the Austrian patient cohort (from 17 March 2020 to 31 July 2021) of the SANTORINI observational study were used for this analysis (Table 1).
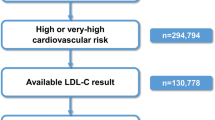
Patients from the SANTORINI Austrian cohort were eligible for inclusion in the simulation (Table 1) if they were receiving any LLT, had a known statin regimen (if on statins), and had a non-missing baseline LDL‑C value (directly recorded or calculated using the Friedewald formula) [31]. Patients who at baseline were documented to be on no LLT (n = 76; assumed to be newly identified patients) or on a PCSK9 inhibitor (N = 61; assumed to have gone through treatment intensification) were excluded from the simulation. No statin intensification was simulated because it was assumed that LLT was at the maximum-tolerated regimen at baseline for those patients already on a statin or ezetimibe. Patients were stratified into high and very high CV risk groups using the risk classifications by the 2019 ESC/EAS guidelines [1].
Simulation of the lipid-lowering therapy pathway and LDL-C reduction
We used a Monte Carlo simulation approach as reported previously [32,33,34,35] to simulate the addition of oral bempedoic acid after ezetimibe in the LLT pathway in the Austrian SANTORINI cohort (Fig. 1).
In the simulation, it was first determined whether the baseline LDL‑C value of patients (on an existing LLT) met their individual risk-based goal, as defined by the 2019 ESC/EAS guidelines (i.e., < 70 mg/dL or 1.8 mmol/L for those at high CV risk and < 55 mg/dL or 1.4 mmol/L for those at very high CV risk [1]). For patients not at goal, an LLT intensifying algorithm was applied (Fig. 1). The algorithm sequentially simulated the addition of ezetimibe (10 mg) and, optionally, bempedoic acid (180 mg) in case of non-achievement of LDL‑C treatment goal. The effect of the simulated treatment relied on probabilistically generated LDL-C-reduction efficacies sampled from probabilistic density functions derived from clinical trial data for each drug. The number of patients receiving treatment, the number reaching their LDL‑C goal, and the overall LDL‑C value for the patient cohort were estimated after each step of the simulation. For patients with LDL‑C levels higher than their individual goal and not already receiving ezetimibe treatment, the effect of adding ezetimibe treatment on LDL‑C was simulated. For patients still not at goal (either with ezetimibe at baseline or after addition of ezetimibe in the simulation), the effect of adding bempedoic acid treatment on LDL‑C was simulated.
The efficacy of ezetimibe was simulated in a similar way to that reported by Cannon et al. (2017), using a beta distribution with a mean LDL‑C reduction from baseline of 22.7% [36] and standard deviation (SD) of 16.5% [37]. The alpha and beta parameters of the distribution used were not reported by Cannon et al. [33]. In the present simulation, a beta distribution with alpha = 1.6 and beta = 5.4 was used, providing a reasonable approximation of the reported treatment effect (mean, 22.9%; SD, 14.8%) (Table 1).
The efficacy of bempedoic acid was simulated as reported previously [38] using lognormal distributions derived from the treatment effects observed in the CLEAR studies, for which patient-level data were available [38]. The lognormal distribution was selected because it allows for increases in LDL‑C level as well as decreases. For patients receiving moderate- or high-dose statin at baseline, the efficacy distribution for bempedoic acid was estimated on the basis of the pooled patient-level data from CLEAR Harmony [25] and CLEAR Wisdom (Fig. 2a, [23]). For patients receiving no or low-dose statin at baseline, the efficacy distribution for bempedoic acid was estimated on the basis of the pooled patient-level data from CLEAR Serenity [24] and CLEAR Tranquility (Fig. 2b, [22]). Table 2 presents the parameters of the distributions applied for modelling of the trial data.
Treatment effects for bempedoic acid in patients receiving: a moderate or high-dose statin, Pooled Patient-Level Data from CLEAR Harmony and CLEAR Wisdom (Pool 1); n = 1922; b no or low-dose statin as background therapy, Pooled Patient-Level Data from CLEAR Serenity and CLEAR Tranquility (Pool 2); n = 399. Green bars represent the patient distribution for the ratio of LDL‑C at week 12 versus LDL‑C at baseline observed in the pooled CLEAR trial data. The blue curves represent the fitted lognormal distributions (LDL‑C low-density lipoprotein cholesterol)
The effect of treatment on LDL‑C levels was estimated using Monte Carlo simulation with probabilistic sampling of the treatment effects; we ran 10,000 simulations of the complete set of patients. Simulations were performed using R Version 4.0.3 [39]. Variables were double programmed independently by 2 statisticians and checked, and the simulation programme was run and checked by a second statistician. After each of the 10,000 simulations, the mean LDL‑C value of the patient cohort was calculated after the addition of ezetimibe and after the addition of bempedoic acid in the simulation. The median, the 2.5% quartile, and the 97.5% quartile of these 10,000 LDL‑C means were calculated. Similarly, the number of patients at goal was estimated at the end of each simulation step, then the median, the 2.5% quartile, and the 97.5% quartile of these 10,000 LDL‑C numbers were calculated on completion of the simulation.
Results
The baseline characteristics of high and very high-risk individuals of the Austrian SANTORINI cohort (N = 310) are presented in Table 3. The mean age was 65 years, 36% were female, 73% with existing cardiovascular disease (secondary prevention) and 38% diabetic. The mean LDL‑C was 93.58 mg/dL (SD 57.73), with 39.0% of patients on statin monotherapy, 12.5% on ezetimibe monotherapy or with statins, 19.6% PCSK9i (alone or in combination) and 26.1% on no lipid-lowering therapy (Table 4). From this cohort, for the purpose of the simulation, patients who were not on any LLT at baseline (n = 76) were excluded, as it was assumed that they were newly identified individuals of high risk needing initiation with statin or statin intolerant individuals, who would need to go through statin optimization. Patients who were already on PCSK9 inhibitors at baseline were also excluded (n = 61) assuming that these patients, based on prescription criteria in Austria for PCSK9 inhibitors, were on their maximum-tolerated regimen of lipid-lowering therapy and would not qualify for ezetimibe or bempedoic acid add-on; therefore, the simulation cohort used was a subset of the overall SANTORINI cohort (n = 144; see also Table 1).
The mean LDL‑C of this cohort was 76.4 mg/dL, with 94% (n = 135) of patients on statins, the vast majority of whom were on moderate or high intensity statin (99.3%, n = 134); 24% (n = 35) were on ezetimibe, either as monotherapy or in combination (Table 4). Fifty-two patients (36.1%) had LDL‑C values meeting their risk-based ESC/EAS 2019 recommended goal. Goal attainment was similar independent of CV risk level (i.e., high or very high risk) (Fig. 3b). In addition, for those patients for whom the physician reported using the 2019 ESC/EAS guidelines for risk classification, we compared the physician-reported CV risk with the calculated risk using the patient data and medical history. Interestingly, there was an underestimation of the true CV risk for a proportion of patients (Fig. 3a).
Comparison of physician-reported versus calculated CV risk using the ESC/EAS classification (a) and goal attainment overall and by CV risk (b) in the simulation cohort. CV risk was calculated as per the risk classification reported in ESC/EAS 2019 guidelines. LDL‑C goal attainment was determined according to the ESC/EAS 2019 recommendations (CV cardiovascular, EAS European Atherosclerosis Society, ESC European Society for Cardiology)
In the simulation, out of the 92 patients not at goal, 72 were not receiving ezetimibe at baseline and thus were simulated to receive ezetimibe. A third of these patients (33%, n = 24 out of 72) reached their risk-based goal (Fig. 1). Another 68 patients were not at goal after ezetimibe (20 on ezetimibe at baseline and 48 still not at goal after simulation of ezetimibe) and thus were allocated bempedoic acid add-on therapy in the simulation. Addition of bempedoic acid was estimated to result in additional 35% (n = 24 out of 68) of patients reaching their goal.
Overall, the cumulative number of patients at goal in the cohort was estimated to increase from 52 (36.1%) at baseline to 76 (52.8%) and 100 (69.4%) after addition of ezetimibe and bempedoic acid, subsequently (Fig. 4). The distribution of patient LDL‑C levels at baseline and at the end of the simulation is presented in Fig. 5. The proportion of patients with LDL‑C lower than 55 and 70 mg/dL was substantially increased after the treatment simulation. For example, the proportion of patients with LDL‑C lower than 55 mg/dL almost doubled from 35–67%, and the proportion of patients with LDL‑C lower than 70 mg/dL increased from 55–80%. The mean LDL‑C for the whole cohort lowered from 76.4 mg/dL at baseline to 65.4 mg/dL and 57.7 mg/dL, after the sequential simulation of ezetimibe and bempedoic acid respectively (Fig. 4). At the end of the simulation, 74.3% of the overall cohort of 144 patients were receiving ezetimibe and 47.2% were receiving bempedoic acid.
Discussion
In our simulation, the cumulative number of patients at their risk-based LDL‑C goal in the Austrian cohort was estimated to almost double after addition of ezetimibe and bempedoic acid, from 36% at baseline to a total of 69%. The mean absolute LDL‑C reduction for the whole cohort after this stepwise approach with oral combination treatment was −18.7 mg/dL, from 76.4 mg/dL at baseline to 57.7 mg/dL, with 80% of patients being at an LDL‑C level ≤ 70 mg/dL (Fig. 5).
Strengths of this analysis include (1) the use of a contemporary patient cohort from clinical centres in Austria, (2) particular attention paid to ensuring the accuracy of the LLT and LDL‑C data recorded, and (3) our model accounting for simulating a cohort to a realistic degree and considering the variability of LDL‑C reductions between different patients in response to LLT.
The baseline characteristics and treatment utilisation in the Austrian SANTORINI cohort of high and very high-risk individuals reflect contemporary data within 2 years after the 2019 ESC/EAS guideline update. Despite a high-risk patient cohort with the majority of patients with existing CV disease, treatment patterns remain similar to that reported in the previous European and Austrian DA VINCI study [17, 18], suggesting that guideline implementation in routine practice is lagging behind. CV risk underestimation and underutilisation of combination therapies as shown in our analysis may explain the low goal attainment overall. This analysis simulates how utilising the oral therapies of ezetimibe and bempedoic acid in combination with statins of any intensity would improve attainment of goals and substantially increase the proportion of patients reaching their risk-based goals before utilising PCSK9. In our analysis, a third of patients would still need further optimisation of treatment, such as addition of a PCSK9 inhibitor. Two previous simulation studies in selected German cohorts showed that addition of bempedoic acid to the LLT pathway may help reduce the need for a PCSK9 inhibitor at a population level and subsequently lower the annual overall treatment cost of therapy for healthcare systems [35, 38]. A further simulation study described the expected LDL‑C reduction after initiating bempedoic acid and estimated the potential absolute cardiovascular event risk reduction in patients with ASCVD [40]. Cardiovascular outcomes data for bempedoic acid were expected at the time of this manuscript preparation [41].
Treatment effects for bempedoic acid were simulated using lognormal distributions, which allow for both increases and reductions in LDL‑C, and closely matched the observed patient-level data from the trials. We took a conservative approach in estimating the efficacy of bempedoic acid by using all observed values of LDL‑C from the patient-level data at 12 weeks from baseline; the best-fitted distributions were used, but these potentially underestimate the treatment effect of bempedoic acid in this population. On the contrary, since no patient-level data were available for ezetimibe, we used an efficacy of 22.7% mean LDL‑C reduction simulated via a beta distribution as used by Cannon et al. [33], although its efficacy is reported between 15 and 22% due to relatively high interindividual variation [1]. Because the beta distribution is constrained to values between 0 and 100%, patients receiving ezetimibe in the simulation could only have a reduction in LDL‑C, which may not fully reflect clinical observations [42, 43]. In our analysis, we took a pragmatic approach to assume that the patients who were on a statin at baseline were at their maximum-tolerated dose, after having excluded those who were on no LLT; statin dose intensification was not further simulated. Out of the 310 patients in the SANTORINI Austrian cohort, 39% were on statin monotherapy at baseline and the majority of them were already on moderate or high intensity statin, while another 11% were on statin and ezetimibe combination therapy; this is consistent to that observed in the Austrian analysis of the DA VINCI study [18] where the vast majority of those on statin were indeed at moderate/high intensity. After excluding 26% of patients from the SANTORINI cohort who were on no LLT at baseline (assuming they were either treatment naïve, newly identified high-risk individuals, statin intolerant or not optimally treated and in need of further statin intensification), we mimic a cohort who has been maximised on their statin (and/or ezetimibe use) yet not at goal and would benefit from further oral lipid lowering therapy. It is possible that not all patients in the simulation cohort were at maximum tolerated statin dose, however, we believe that this is the closest to real-world practice.
There are certain limitations associated with this study, including the virtual basis of the analysis. But since we are extrapolating from meticulously collected real-world cohort data and since the calculations of treatment effects were performed in a conservative manner, we believe that our results are realistic and robust. The total number of patients included in the final calculation is quite low and may therefore not be representative of the Austrian high-cardiovascular risk population. Data capture was limiting and therefore we were unable to differentiate who was statin intolerant (not willing or able to tolerate statins) or treatment naïve/newly diagnosed patients and therefore these patients were excluded from the analysis. As per EAS/ESC 2019 guidelines and local treatment algorithms, the patients who were not on LLT despite having high or very high CV risk, should as a first step initiate statins, but this was out of scope for this simulation.
Furthermore, the study might be prone to selection bias because the SANTORINI study recruited patients that were deemed to be of high or very high CV risk and in need of lipid treatment. In our cohort, around 20% of individuals had HeFH which is somewhat higher than the overall proportion reported in epidemiological studies. This may be related to a selection bias since HeFH patients are most often being enrolled in registries such as the SANTORINI study and centers for lipid management. Lastly, the treatment effect of add-on LLT can only be expected if the medication is taken compliantly; in our analysis we did not account for non-adherence, neither did we account for adverse effects/safety, following similar approach to previous simulation studies.
In conclusion, optimising further the oral LLT pathway after statins by the use of bempedoic acid and ezetimibe add-on could result in substantial improvements in the number of patients reaching their LDL‑C goals.
References
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41(1):111–88. https://doi.org/10.1093/eurheartj/ehz455.
EHN. European Heart Network. European cardiovascular disease statistics in 2017. 2017. http://www.ehnheart.org/cvd-statistics.html. Accessed 4 July 2022.
Agabiti Rosei E, Salvetti M. Management of hypercholesterolemia, appropriateness of therapeutic approaches and new drugs in patients with high cardiovascular risk. High Blood Press Cardiovasc Prev. 2016;23(3):217–30. https://doi.org/10.1007/s40292-016-0155-2.
Munir H, Morais JA, Goldfarb M. Health-related quality of life in older adults with acute cardiovascular disease undergoing early mobilization. CJC Open. 2021;3(7):888–95. https://doi.org/10.1016/j.cjco.2021.02.013.
Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459–72. https://doi.org/10.1093/eurheartj/ehx144.
Averna M, Banach M, Bruckert E, Drexel H, Farnier M, Gaita D, et al. Practical guidance for combination lipid-modifying therapy in high- and very-high-risk patients: A statement from a European Atherosclerosis Society Task Force. Atherosclerosis. 2021;325:99–109. https://doi.org/10.1016/j.atherosclerosis.2021.03.039.
National Institute for Health and Care Excellence. Bempedoic acid with ezetimibe for treating primary hypercholesterolaemia or mixed dyslipidaemia [TA694]. 2021. https://www.nice.org.uk/guidance/ta694. Accessed 4 July 2022.
Borén J, Chapman MJ, Krauss RM, Packard CJ, Bentzon JF, Binder CJ, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2020;41(24):2313–30. https://doi.org/10.1093/eurheartj/ehz962.
Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81. https://doi.org/10.1016/s0140-6736(10)61350-5.
Ray KK, Reeskamp LF, Laufs U, Banach M, Mach F, Tokgözoğlu LS, et al. Combination lipid-lowering therapy as first-line strategy in very high-risk patients. Eur Heart J. 2022;43(8):830–3. https://doi.org/10.1093/eurheartj/ehab718.
Ference BA, Yoo W, Alesh I, Mahajan N, Mirowska KK, Mewada A, et al. Effect of long-term exposure to lower low-density lipoprotein cholesterol beginning early in life on the risk of coronary heart disease: a Mendelian randomization analysis. J Am Coll Cardiol. 2012;60(25):2631–9. https://doi.org/10.1016/j.jacc.2012.09.017.
Holmes MV, Asselbergs FW, Palmer TM, Drenos F, Lanktree MB, Nelson CP, et al. Mendelian randomization of blood lipids for coronary heart disease. Eur Heart J. 2015;36(9):539–50. https://doi.org/10.1093/eurheartj/eht571.
Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337. https://doi.org/10.1093/eurheartj/ehab484.
Barrios V, Soronen J, Carter AM, Anastassopoulou A. Lipid management across Europe in the real-world setting: a rapid evidence review. Curr Med Res Opin. 2021;37(12):2049–59. https://doi.org/10.1080/03007995.2021.1973396.
De Luca L, Arca M, Temporelli PL, Meessen J, Riccio C, Bonomo P, et al. Current lipid lowering treatment and attainment of LDL targets recommended by ESC/EAS guidelines in very high-risk patients with established atherosclerotic cardiovascular disease: Insights from the START registry. Int J Cardiol. 2020;316:229–35. https://doi.org/10.1016/j.ijcard.2020.05.055.
Fox KM, Tai MH, Kostev K, Hatz M, Qian Y, Laufs U. Treatment patterns and low-density lipoprotein cholesterol (LDL-C) goal attainment among patients receiving high- or moderate-intensity statins. Clin Res Cardiol. 2018;107(5):380–8. https://doi.org/10.1007/s00392-017-1193-z.
Ray KK, Molemans B, Schoonen WM, Giovas P, Bray S, Kiru G, et al. EU-wide cross-sectional observational study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prev Cardiol. 2021;28(11):1279–89. https://doi.org/10.1093/eurjpc/zwaa047.
Siostrzonek P, Brath H, Zweiker R, Drexel H, Hoelzl R, Hemetsberger M, et al. Lipid lowering therapy in primary and secondary prevention in Austria: are LDL‑C goals achieved? : Results from the DA VINCI study. Wien Klin Wochenschr. 2022;134(7–8):294–301. https://doi.org/10.1007/s00508-021-01978-w.
Katzmann JL, Sorio-Vilela F, Dornstauder E, Fraas U, Smieszek T, Zappacosta S, et al. Non-statin lipid-lowering therapy over time in very-high-risk patients: effectiveness of fixed-dose statin/ezetimibe compared to separate pill combination on LDL‑C. Clin Res Cardiol. 2022;111(3):243–52. https://doi.org/10.1007/s00392-020-01740-8.
Kotseva K, Wood D, De Bacquer D, De Backer G, Rydén L, Jennings C, et al. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol. 2016;23(6):636–48. https://doi.org/10.1177/2047487315569401.
van de Borne P, Peeters A, Janssens L, Leone A, Lemmens R, Verhaegen A, et al. Lipid-lowering therapy and risk-based LDL‑C goal attainment in Belgium: DA VINCI observational study. Acta Cardiol. 2022;20:1–10. https://doi.org/10.1080/00015385.2022.2030568.
Ballantyne CM, Banach M, Mancini GBJ, Lepor NE, Hanselman JC, Zhao X, et al. Efficacy and safety of bempedoic acid added to ezetimibe in statin-intolerant patients with hypercholesterolemia: A randomized, placebo-controlled study. Atherosclerosis. 2018;277:195–203. https://doi.org/10.1016/j.atherosclerosis.2018.06.002.
Goldberg AC, Leiter LA, Stroes ESG, Baum SJ, Hanselman JC, Bloedon LT, et al. Effect of Bempedoic acid vs placebo added to maximally tolerated statins on low-density lipoprotein cholesterol in patients at high risk for cardiovascular disease: the CLEAR wisdom randomized clinical trial. JAMA. 2019;322(18):1780–8. https://doi.org/10.1001/jama.2019.16585.
Laufs U, Banach M, Mancini GBJ, Gaudet D, Bloedon LT, Sterling LR, et al. Efficacy and safety of bempedoic acid in patients with hypercholesterolemia and statin intolerance. J Am Heart Assoc. 2019;8(7):e11662. https://doi.org/10.1161/jaha.118.011662.
Ray KK, Bays HE, Catapano AL, Lalwani ND, Bloedon LT, Sterling LR, et al. Safety and efficacy of bempedoic acid to reduce LDL cholesterol. N Engl J Med. 2019;380(11):1022–32. https://doi.org/10.1056/NEJMoa1803917.
Ballantyne CM, Laufs U, Ray KK, Leiter LA, Bays HE, Goldberg AC, et al. Bempedoic acid plus ezetimibe fixed-dose combination in patients with hypercholesterolemia and high CVD risk treated with maximally tolerated statin therapy. Eur J Prev Cardiol. 2020;27(6):593–603. https://doi.org/10.1177/2047487319864671.
Colivicchi F, Di Fusco SA, Scicchitano P, Caldarola P, Murrone A, Valente S, et al. Updated clinical evidence and place in therapy of bempedoic acid for hypercholesterolemia: ANMCO position paper. J Cardiovasc Med (Hagerstown). 2021;22(3):162–71. https://doi.org/10.2459/jcm.0000000000001108.
Laufs U, Friede T, Koenig W, Landmesser U, Nowak B, Zimmermann W‑H, et al. Joint statement on benefit assessment of bempedoic acid Nilemdo® and bempedoic acid / ezetimibe Nustendi®. Joint statement by DGK/DACH/DDG/DGE/DGFF/DGIM/DGfN. 2021.
Schettler VJJ. Guideline-based procedure in the treatment of hypercholesterolaemia. Dial Aktuell. 2020;2020(24):345–8.
Ray KK, Haq I, Bilitou A, Aguiar C, Arca M, Connolly DL, et al. Evaluation of contemporary treatment of high- and very high-risk patients for the prevention of cardiovascular events in Europe—Methodology and rationale for the multinational observational SANTORINI study. Atheroscler Plus. 2021;43:24–30. https://doi.org/10.1016/j.athplu.2021.08.003.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502.
Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. Br Med J. 2003;326(7404):1423. https://doi.org/10.1136/bmj.326.7404.1423.
Cannon CP, Khan I, Klimchak AC, Reynolds MR, Sanchez RJ, Sasiela WJ. Simulation of lipid-lowering therapy intensification in a population with atherosclerotic cardiovascular disease. JAMA Cardiol. 2017;2(9):959–66. https://doi.org/10.1001/jamacardio.2017.2289.
Allahyari A, Jernberg T, Hagström E, Leosdottir M, Lundman P, Ueda P. Application of the 2019 ESC/EAS dyslipidaemia guidelines to nationwide data of patients with a recent myocardial infarction: a simulation study. Eur Heart J. 2020;41(40):3900–9. https://doi.org/10.1093/eurheartj/ehaa034.
Blaum C, Brunner FJ, Goßling A, Kröger F, Bay B, Lorenz T, et al. Target populations and treatment cost for bempedoic acid and PCSK9 inhibitors: a simulation study in a contemporary CAD cohort. Clin Ther. 2021;43(9):1583–600. https://doi.org/10.1016/j.clinthera.2021.07.019.
Cannon CP, Blazing MA, Giugliano RP, McCagg A, White JA, Theroux P, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372(25):2387–97. https://doi.org/10.1056/NEJMoa1410489.
Descamps O, Tomassini JE, Lin J, Polis AB, Shah A, Brudi P, et al. Variability of the LDL‑C lowering response to ezetimibe and ezetimibe + statin therapy in hypercholesterolemic patients. Atherosclerosis. 2015;240(2):482–9. https://doi.org/10.1016/j.atherosclerosis.2015.03.004.
Katzmann JL, Becker C, Bilitou A, Laufs U. Simulation study on LDL cholesterol target attainment, treatment costs, and ASCVD events with bempedoic acid in patients at high and very-high cardiovascular risk. PLoS ONE. 2022;17(10):e276898. https://doi.org/10.1371/journal.pone.0276898.
R Core Team. R Foundation for Statistical Computing. R: a language and environment for statistical computing. 2021. https://www.R-project.org/. Accessed 4 July 2022.
Gunn LH, McKay AJ, Feng A, Louie MJ, Ballantyne CM, Ray KK. Estimated cardiovascular benefits of bempedoic acid in patients with established cardiovascular disease. Atheroscler Plus. 2022;49:20–7. https://doi.org/10.1016/j.athplu.2022.05.003.
Nicholls S, Lincoff AM, Bays HE, Cho L, Grobbee DE, Kastelein JJ, et al. Rationale and design of the CLEAR-outcomes trial: evaluating the effect of bempedoic acid on cardiovascular events in patients with statin intolerance. Am Heart J. 2021;235:104–12. https://doi.org/10.1016/j.ahj.2020.10.060.
Morrone D, Weintraub WS, Toth PP, Hanson ME, Lowe RS, Lin J, et al. Lipid-altering efficacy of ezetimibe plus statin and statin monotherapy and identification of factors associated with treatment response: a pooled analysis of over 21,000 subjects from 27 clinical trials. Atherosclerosis. 2012;223(2):251–61. https://doi.org/10.1016/j.atherosclerosis.2012.02.016.
Pandor A, Ara RM, Tumur I, Wilkinson AJ, Paisley S, Duenas A, et al. Ezetimibe monotherapy for cholesterol lowering in 2,722 people: systematic review and meta-analysis of randomized controlled trials. J Intern Med. 2009;265(5):568–80. https://doi.org/10.1111/j.1365-2796.2008.02062.x.
Acknowledgements
We would like to thank all the SANTORINI Investigators and patients who participated in the observational study. We acknowledge Carina Dinkel-Keuthage and Annie Burden for their support in statistical analysis and quality control of the data.
Funding
This study was funded by Daiichi Sankyo Europe GmbH.
Author information
Authors and Affiliations
Contributions
All Austrian centres contributed with recruiting patients to the study. ALC and HT were in the steering committee of the SANTORINI study. All co-authors reviewed and provided their scientific input to the manuscript. The medical writing was supported by AB from Daiichi Sankyo.
Corresponding author
Ethics declarations
Conflict of interest
C. Gelsinger, T. Maca, R. Sock declare that they have no competing interests. S. Wolowacz is an employee of RTI Health Solutions. RTI Health Solutions received funding from Daiichi Sankyo Europe GmbH for the preparation of this manuscript. A. Bilitou, M. Koch, S. Wienerroither, and F. Diamand are employees of Daiichi Sankyo. Daiichi Sankyo Europe GmbH is the market authorisation holder in Europe, Switzerland, and the United Kingdom for bempedoic acid and bempedoic acid fixed-dose combination with ezetimibe. All co-authors received study fees from Daiichi Sankyo. H. Toplak has received honoraria for lecturing and consulting as well as research support from Daiichi Sankyo. H. Alber has received study fees from Daiichi Sankyo, and lecture and consulting fees from Daiichi Sankyo, Novartis, Amgen, and Sanofi-Aventis. J. Auer has received consulting work and lecture fees from Novartis, Amgen, Sanofi, and Daiichi Sankyo. M. Clodi has received lecture and consultant fees from Astra Zeneca, Boerhinger Ingelheim, Novo Nordisk, Novartis, Sanofi, Amgen, and Daiichi Sankyo. C. Ebenbichler has received grants and personal fees from Abbott, Amgen, AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Novartis, NovoNordisk, Sanofi, and Sobi. E. Fließer-Görzer has received presentation, study, and/or congress support from Novo Nordisk, AstraZeneca, Bristol-Myers Squibb, Bayer, Novartis, Eli Lilly, Allergan, Daiichi Sankyo, Amgen, Merck Sharpe & Dohme, Boehringer Ingelheim, and Sanofi Aventis. U. Hanusch has acted as investigator in clinical trials conducted by Bayer, Lilly, Amgen, Vertanical, and Novo Nordisk. B. Ludvik has received honoraria for lectures, advisory boards, and research support from Amgen, Sanofi, Novartis, and Daiichi Sankyo. A. Schober has received speaker fees and institutional research support from Daiichi-Sankyo. W. Speidl has received support for lectures, advisory board participation, clinical trials, and/or other research from Amgen, Daiichi Sankyo, Novartis, and Sanofi. T. Stulnig has received honoraria for lectures and/or consultation as well as travel support from Amgen, Daiichi-Sankyo, Novartis, Sanofi, Sobi; research support from Daiichi-Sankyo and Sanofi. R. Weitgasser has received research grants, speaker fees, and consultant advisory board fees (2017–2022) from the following: Abbott Diabetes Care, Amgen, AstraZeneca, Boehringer Ingelheim, Daiichi Sankyo, Eli Lilly, Medtrust, Merck Sharp & Dohme, Novo Nordisk, Roche Diabetes Care, Sanofi, and Spar. A. Zirlik has received consultant fees from Bayer Health Care, Boehringer Ingelheim, Rigel, Cardiorentis, Medscape Stealth Peptides, Sanofi Aventis, Medtronic, Norvatis and honoraria for lectures from Bayer Health Care, Astra Zeneca, Medtronic, ResMed, Boehringer Ingelheim, Rigel, Sanofi Aventis, Pfizer, Janssen-Cilag, Novartis, Bristol Myers Squibb, Thoratec, Abiomed, Daiichi Sankyo, Abbott and Cardiac Dimensions. A.L. Catapano has received honoraria, lecture fees, or research grants from the following: Amarin, Sigma-Tau, Menarini, Kowa, Recordati, Eli Lilly, AstraZeneca, Mediolanum, Pfizer, Merck, Sanofi, Aegerion, Amgen, Genzyme, Bayer, Sanofi, Regeneron, Daiichi Sankyo, and The Corpus. The work of A.L. Catapano is supported in part by the Italian Ministry of Health—Ricerca Corrente.
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants for being included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Toplak, H., Bilitou, A., Alber, H. et al. Simulation of bempedoic acid and ezetimibe in the lipid-lowering treatment pathway in Austria using the contemporary SANTORINI cohort of high and very high risk patients. Wien Klin Wochenschr 135, 364–374 (2023). https://doi.org/10.1007/s00508-023-02221-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-023-02221-4