Summary
Background
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has undergone different molecular changes, sprouting genetic variants of the original wildtype. Clinical comparisons between patients infected with alpha versus delta are scarce.
Methods
In this retrospective observational study, adult patients hospitalized with coronavirus disease 2019 (COVID-19) due to confirmed SARS-CoV‑2 alpha or delta infection were included. Patient characteristics, virologic and laboratory parameters, as well as the clinical course were compared in patients infected with alpha vs. delta variants.
Results
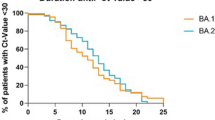
A total of 106 patients infected with alpha and 215 patients infected with delta were included. Patients infected with the delta variant were admitted to hospital earlier after symptom onset (6 vs. 7 days, p < 0.001). Blood levels of C‑reactive protein (43.3 vs. 62.9 mg/l, p = 0.02) and neutrophil count (3.81 vs. 4.53 G/l, p = 0.06) were lower in delta patients. Furthermore, at hospital admission cycle threshold (CT) values were significantly lower in patients infected with the delta variant (22.3 vs. 24.9, p < 0.001). Patients infected with the delta variant needed supplemental oxygen less often during disease course (50% vs. 64%, p = 0.02). Furthermore, there was a statistically non-significant trend towards a lower ICU admission rate among delta patients (16% vs. 24%, p = 0.08)
Conclusion
Patients diagnosed with the delta variant were admitted to the hospital earlier, had a less severe course of disease and a higher viral replication on admission. This may provide a window of opportunity for antivirals in the hospital setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe acute respiratory syndrome corona virus 2 (SARS-CoV2) has caused a global pandemic resulting in deaths in excess of about 3 million [1]. Since the first clinical cases of coronavirus disease 2019 (COVID-19) emerged in late 2019 [2], it has acquired numerous mutations resulting in the appearance and spread of viral variants. In September 2020, mutations of the spike protein on the surface of SARS-CoV‑2 were responsible for the emergence of variant B.1.1.7 (alpha variant) [3]. Further down the road in December 2020, it was deemed a “variant of concern” (VoC), implying higher transmissibility, virulence and/or immunity to previously built antibodies [4]. In addition to the D614G mutation which arose in Europe as B.1 [5] in early 2020 and is now found in all SARS-CoV‑2 strains, B.1.1.7 is defined by a total of 23 mutations including the N501 mutation resulting in higher affinity to the receptor binding domain (RBD) of angiotensin-converting enzyme 2 (ACE2) receptors [6]. B.1.1.7 has been suspected to precipitate higher viral loads and a reduction by a small proportion in neutralization though RBD antibodies [7] and is associated with higher hazards for hospitalization and all cause death [8]; however, the virus kept mutating, spawning new variants over the course of this pandemic. With the earliest documented sample in India during October 2020, B.1.617.2. (delta variant) soon was deemed a VoC after first findings indicated a higher transmission rate [9] and a lower responsiveness to convalescent antibodies [10]. B1.617.2 which only has the D614G mutation in common with B.1.1.7 [11] has been associated with significantly higher viral loads in infected persons [12] and a higher risk for hospitalization [13]. The virologic differences between the alpha and delta variant have been well-characterized but comparisons of clinical characteristics remain scarce. In this study we aimed to describe and compare patient characteristics, the symptomatology, and clinical course of patients infected with the alpha and delta variants in one large treatment center in Austria.
Methods
Study design and accumulation of data
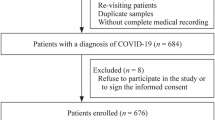
This retrospective study was performed at the department of Tropical Medicine and Infectious Diseases at the Clinic Favoriten in Vienna, Austria. All consecutive patients hospitalized for the treatment of COVID-19 from 1 May 2021 to 31 August 2021, were included if they had PCR proven SARS-CoV‑2 infection and had information available on the SARS-CoV‑2 variant as assessed by PCR. The time frame for this explorative study was chosen to enable a realistic comparison between the two genetic variants, since the delta variant became increasingly more prevalent in Austria after June 2021. Patients in whom infection was not confirmed by PCR testing were excluded. Furthermore, patients in whom the mutation was not determined were excluded from this study.
Patient medical records were used to collect data on patient characteristics including demographic information and information on comorbidities, comedications, laboratory and clinical follow-up data.
Laboratory analysis
At the hospital, infection with SARS-CoV‑2 was diagnosed using the cobas® SARS-CoV‑2 kit with material from nasopharyngeal swabs on the Cobas 6800 (Roche Molecular Systems, Branchburg, NJ, USA) platform by Roche and CT values were used as a surrogate for viral loads [14]. Swabs were routinely obtained on admission and repeated at the discretion of the attending physician until discharge. Variants were detected by melting curve analysis using the VirSNiP SARS-CoV‑2 Spike Kits by TIB MOLBIOL on the cobas® z480 by Roche. All samples were processed and analyzed at the hospital department of laboratory medicine.
Definition of variables and endpoints
The self-reported first day of COVID-19 symptoms (e.g. headache, fever, cough, rhinitis, dyspnea, fatigue, myalgia, and arthralgia) were recorded and defined as day 1 of symptomatic infection. Need for nasal oxygen supplementation and development of severe respiratory failure with at least need for high flow oxygen therapy (HFOT) were chosen as primary outcome parameters. Furthermore, time of symptom onset until hospitalization as well as length of stay were calculated.
Statistical analysis
P-values < 0.05 were considered as statistically significant. For statistical analysis, SPSS 27 software (SPSS, Inc., Chicago, IL, USA) was used. For statistical analysis, mainly non-parametric tests were conducted. Mann-Whitney U‑test was applied for evaluation of disparities in a parameter between two groups. The χ2-test was used to evaluate frequencies between two groups. In cases of expected frequencies of an event below five observations, Fisher’s exact test was applied. Illustrations of the collected data, such as boxplots, were created using GraphPad Prism 9 and cleared of outliners to improve visualization.
The study was approved by the local ethics committee.
Results
Characteristics of hospitalized patients
From May 1st to August 31st, 2021, 408 patients were hospitalized for COVID-19 and 87 patients had to be excluded because of missing results of the mutation analysis. Therefore, 321 patients were included in the analysis. Of these 106 tested positive for the alpha variant, whereas 215 tested positive for the delta variant. The first patient at the hospital with the delta variant was admitted on the 5th of June and the last patient with a detected alpha variant was admitted on the 11th of July (Fig. 1). Among all patients, gender was evenly distributed but there was a tendency towards more women being hospitalized with delta compared to admissions with the alpha variant (54% vs. 43%, p = 0.08). The median age in the alpha and the delta group were 55 years (interquartile range, IQR 45–64 years) and 52 years (IQR 41–65 years), respectively (p = 0.17). More baseline characteristics are shown in Table 1.
Admission and course of disease
Time from symptom onset to hospital admission was significantly shorter in patients with the alpha variant compared to those with delta (6 vs. 7 days, p < 0.01, Fig. 2).
Type of reported symptoms showed no disparities between groups and need for supplemental oxygen at the time of admission was not significantly different (59% vs 53%, p = 0.32). Total duration of hospitalization was comparable between alpha (median 9 days, IQR 7–16) and delta (median 9 days, IQR 6–14, p = 0.65). About 55% of all admitted patients needed oxygen at some point during hospitalization. Patients with the alpha variant needed supplemental oxygen in 64% of the cases as compared to 50% of patients with the delta variant (p = 0.02) without a significant difference in the proportion of patients requiring high flow oxygen in both groups (37% vs. 32%, p = 0.31).
Of the patients with the alpha variant 26 (24%) were admitted to the ICU, compared to 35 (16%) patients with the delta variant (p = 0.08), 24 (7.5%) patients infected with alpha and 18 patients (8.4%) infected with delta died (p = 0.39). Overall risk for oxygen supplementation during hospitalization was lower in patients with delta vs. alpha (odds ratio, OR = 0.52; 95% confidence interval, CI 0.32–0.83). Patients infected with the alpha variant tended to have a higher risk for an ICU admission (OR = 0.6; 95% CI 0.34–1.06).
Baseline laboratory and viral load at admission
Laboratory parameters at time of admission are depicted in Table 2. C‑reactive protein (CRP) was significantly higher in patients who tested positive for the alpha mutation with a median of 62.9 mg/l (IQR 28.9–110.4 mg/l) compared to 43.3 mg/l (14.6–100 mg/l) in the delta group (p = 0.02). CRP itself highly correlated with the need for at least HFOT as well as ICU admissions (p < 0.001) Neutrophil count also tended to be higher in alpha (median 4.53 G/l, IQR 3.18–5.66 G/l) versus delta patients (median 3.81 G/l, IQR 2.56–5.74 G/l, p = 0.06, Table 2).
Furthermore, CT-values at the day of hospitalization were significantly lower in alpha patients. The median values were 24.9 cycles for alpha and 22.3 cycles for delta (p < 0.001, Fig. 3).
Vaccination status
In patients with the alpha variant 40/106 patients had information on vaccination status. Among those, 33 were unvaccinated, 5 partially and 2 fully vaccinated. In patients with the delta variant, data were available in 168/215 patients. Of those, 127 were unvaccinated, 7 had received one dose and 34 were fully vaccinated. The percentages of fully vaccinated patients in their respective groups were 2% in alpha and 15% in delta.
Discussion
In this retrospective observational study, differences in patients admitted for COVID-19 caused by the alpha and delta SARS-CoV‑2 variants were observed. Patients infected with the delta variant had a lower rate of need for oxygen supplementation at admission. Furthermore, there was a trend towards a lower risk for ICU admission during their course of disease. Additionally, patients with the delta variant showed significantly decreased inflammation markers including CRP and elevated white cell count on admission, both of which are closely associated with HFOT and ICU admission in this study as well as being linked to higher severity of disease in literature [15,16,17]. Interestingly, there were no significant differences in terms of patient demographics and comorbidities which could otherwise explain the discrepancies regarding disease severity. A difference in mortality or length of hospital stay could not be detected in the two groups.
Despite the lower disease severity as measured by the requirement for oxygen supplementation or laboratory inflammation markers, patients infected with the delta variant were hospitalized 1 day earlier. In these patients CT-values on admission were significantly lower which indicates a higher viral load and was previously ascribed to infections with the delta variant in general [12]. It can be speculated that patients infected with delta had a higher perception and severity of felt symptoms in the absence of objective findings of disease severity, which led to a faster admission; however, a significant difference in the spectrum of reported symptoms and the severity between patients in alpha versus delta could not be found. In addition, a positive correlation of more symptoms and higher viral load was not reported in literature [18].
Another reason for earlier hospitalization could also be the rising awareness of the disease caused by the delta variant and the potential for adverse outcomes in combination with the increased availability of testing sites. This could have motivated patients to seek emergency care more readily and family doctors and primary care facilities to send patients more frequently for admission at the hospital. This is problematic as hospital beds may rapidly become scarce amidst a pandemic and alternative care pathways centered on home-based care could hold off pressure from hospitals [19].
The increasing availability and uptake of vaccinations which had been increasingly rolled out during the delta wave, may provide an alternative explanation of the lower disease severity in patients infected with delta observed at admission [20]; however, only 15% of patients were fully vaccinated and an additional 7% were partly vaccinated which is unlikely to fully explain the milder symptoms on admission although information on vaccination status was not available in all patients.
Regardless of the reason, patients seeking healthcare early may benefit from therapeutic interventions like antiviral therapeutics and monoclonal antibodies. Those seem to provide maximum benefit in terms of avoiding complications which has been shown in outpatient setting with agents such as the antiviral drug molnupiravir and the monoclonal antibody sotrovimab [21, 22], which managed to reduce progression of disease significantly compared to their respective placebo group; however, similar studies in hospitalized patients often failed to show benefits [23, 24] with the possible exception of seronegative patients as observed in the RECOVERY trial, where mortality could be successfully reduced in patients receiving treatment with monoclonal antibodies [25]. Similarly, the antiviral remdesivir has recently been shown to prevent progression when given early [26], whereas death may not be prevented when started later in disease among hospitalized patients [27].
With earlier admissions because of emerging variants including delta or omicron, there may be a new window of opportunity for antivirals in the hospital setting which needs to be investigated further [28].
This study provides important insides into changing patient characteristics in the light of emerging SARS-CoV‑2 variants which is necessary to guide appropriate care pathways and therapeutic interventions.
There were some limitations. This was a single center study which only examined a small sample size over a set period; however, despite fluctuating incidences of infection, admission practises in this large treatment center have remained stable over the 4 months of the study. Also, evaluation of symptom onset often relied on subjective information reported by the patient; however, when only analyzing patients, who had a positive test before they developed symptoms, the median time until admission was 6 days in the delta group compared to the alpha group with a median time of 9 days, supporting the main finding of our study.
In addition, vaccination status was only known for a limited number of patients. Therefore, no conclusions regarding a differential vaccine efficacy between the alpha and delta variant can be drawn within this study population.
In conclusion, this study describes a cohort of consecutively hospitalized patients for infection with SARS-CoV-2 at the transition from alpha to delta in the summer of 2021. Patients infected with the delta variant had a higher viral replication and were admitted earlier in the course of disease which may provide a window of opportunity for early interventions including antiviral substances and monoclonal antibodies which must be further evaluated in this setting.
References
Karlinsky A, Kobak D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. Elife. 2021;10:e69336.
Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–9.
Volz E, Mishra S, Chand M, Barrett JC, Johnson R, Geidelberg L, et al. Transmission of SARS-CoV‑2 Lineage B.1.1.7 in England: insights from linking epidemiological and genetic data. medRxiv, 2020.12.30.20249034. 2021.
Galloway SE, Paul P, MacCannell DR, Johansson MA, Brooks JT, MacNeil A, et al. Emergence of SARS-coV‑2 B.1.1.7 lineage—United States, december 29, 2020-january 12, 2021. Mmwr Morb Mortal Wkly Rep. 2021;70(3):95–9.
Worobey M, Pekar J, Larsen BB, Nelson MI, Hill V, Joy JB, et al. The emergence of SARS-CoV‑2 in Europe and North America. Science. 2020;370(6516):564–70.
Starr TN, Greaney AJ, Hilton SK, Ellis D, Crawford KHD, Dingens AS, et al. Deep mutational scanning of SARS-CoV‑2 receptor binding domain reveals constraints on folding and ACE2 binding. Cell. 2020;182(5):1295–310.e20.
Harvey WT, Carabelli AM, Jackson B, Gupta RK, Thomson EC, Harrison EM, et al. SARS-CoV‑2 variants, spike mutations and immune escape. Nat Rev Microbiol. 2021;19(7):409–24.
Grint DJ, Wing K, Houlihan C, Gibbs HP, Evans SJW, Williamson E, et al. Severity of severe acute respiratory system Coronavirus 2 (SARS-coV-2) alpha variant (B.1.1.7) in England. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab754.
Earnest R, Uddin R, Matluk N, Renzette N, Siddle KJ, Loreth C, et al. Comparative transmissibility of SARS-CoV‑2 variants Delta and Alpha in New England, USA. medRxiv, 2021.10.06.21264641. 2021.
Planas D, Veyer D, Baidaliuk A, Staropoli I, Guivel-Benhassine F, Rajah MM, et al. Reduced sensitivity of SARS-CoV‑2 variant Delta to antibody neutralization. Nature. 2021;596(7871):276–80.
Salleh MZ, Derrick JP, Deris ZZ. Structural evaluation of the spike glycoprotein variants on SARS-coV‑2 transmission and immune evasion. Int J Mol Sci. 2021;22(14):7425.
Teyssou E, Delagrèverie H, Visseaux B, Lambert-Niclot S, Brichler S, Ferre V, et al. The Delta SARS-CoV‑2 variant has a higher viral load than the Beta and the historical variants in nasopharyngeal samples from newly diagnosed COVID-19 patients. J Infect. 2021;83(4):e1–e3.
Twohig KA, Nyberg T, Zaidi A, Thelwall S, Sinnathamby MA, Aliabadi S, et al. Hospital admission and emergency care attendance risk for SARS-CoV‑2 delta (B.1.617.2) compared with alpha (B.1.1.7) variants of concern: a cohort study. Lancet Infect Dis. 2022. https://doi.org/10.1016/S1473-3099(21)00475-8.
Rao SN, Manissero D, Steele VR, Pareja J. A narrative systematic review of the clinical utility of cycle threshold values in the context of COVID-19. Infect Dis Ther. 2020;9(3):573–86.
Herold T, Jurinovic V, Arnreich C, Lipworth BJ, Hellmuth JC, von Bergwelt-Baildon M, et al. Elevated levels of IL‑6 and CRP predict the need for mechanical ventilation in COVID-19. J Allergy Clin Immunol. 2020;146(1):128–136.e4.
Cavalcante-Silva LHA, Carvalho DCM, Lima ÉA, Galvão JGFM, da Silva JSF, Sales-Neto JM, et al. Neutrophils and COVID-19: the road so far. Int Immunopharmacol. 2021;90:107233.
Tomar B, Anders H‑J, Desai J, Mulay SR. Neutrophils and neutrophil extracellular traps drive necroinflammation in COVID-19. Cells. 2020;9(6):1383.
Lee S, Kim T, Lee E, Lee C, Kim H, Rhee H, et al. Clinical course and molecular viral shedding among asymptomatic and symptomatic patients with SARS-CoV‑2 infection in a community treatment center in the republic of korea. JAMA Intern Med. 2020;180(11):1447–52.
Kripalani S, Theobald CN, Anctil B, Vasilevskis EE. Reducing hospital readmission rates: current strategies and future directions. Annu Rev Med. 2014;65:471–85.
Chia PY, Ong SWX, Chiew CJ, Ang LW, Chavatte J‑M, Mak T‑M, et al. Virological and serological kinetics of SARS-CoV‑2 Delta variant vaccine breakthrough infections: a multicentre cohort study. Clin Microbiol Infect. 2021. https://doi.org/10.1016/j.cmi.2021.11.010.
Jayk Bernal A, Gomes da Silva MM, Musungaie DB, Kovalchuk E, Gonzalez A, Delos RV, et al. Molnupiravir for oral treatment of Covid-19 in nonhospitalized patients. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2116044.
Gupta A, Gonzalez-Rojas Y, Juarez E, Crespo Casal M, Moya J, Falci DR, et al. Early treatment for Covid-19 with SARS-coV‑2 neutralizing antibody sotrovimab. N Engl J Med. 2021;385(21):1941–50.
A Neutralizing Monoclonal Antibody for Hospitalized Patients with Covid-19. New England Journal of Medicine. 2020;384(10):905–14.
Cao B, Hayden FG. Antiviral monotherapy for hospitalised patients with COVID-19 is not enough. Lancet. 2020;396(10259):1310–1.
Group RC, Horby PW, Mafham M, Peto L, Campbell M, Pessoa-Amorim G, et al. Casirivimab and imdevimab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. medRxiv, 2021.06.15.21258542. 2021.
Gottlieb RL, Vaca CE, Paredes R, Mera J, Webb BJ, Perez G, et al. Early remdesivir to prevent progression to severe Covid-19 in outpatients. N Engl J Med. 2021. https://doi.org/10.1056/NEJMoa2116846.
Ader F, Bouscambert-Duchamp M, Hites M, Peiffer-Smadja N, Poissy J, Belhadi D, et al. Remdesivir plus standard of care versus standard of care alone for the treatment of patients admitted to hospital with COVID-19 (DisCoVeRy): a phase 3, randomised, controlled, open-label trial. Lancet Infect Dis. 2021. https://doi.org/10.1016/S1473-3099(21)00485-0.
Sundararaj Stanleyraj J, Sethuraman N, Gupta R, Thiruvoth S, Gupta M, Ryo A. Treating COVID-19: are we missing out the window of opportunity? J Antimicrob Chemother. 2020;76(2):283–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. Rumpf, B. Lickefett, C. Baumgartner, V. Kauer, M. Karolyi, E. Pawelka, T. Seitz, M. Traugott, P. Triska, A. Bergthaler, H. Laferl, C. Wenisch and A. Zoufaly declare that they have no competing interests.
Ethical standards
The study was approved by the local ethics committee.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors Benedikt Rumpf and Benno Lickefett contributed equally.
Anonymous data could be shared on demand.
Rights and permissions
About this article
Cite this article
Rumpf, B., Lickefett, B., Baumgartner, C. et al. Comparison of clinical characteristics among patients infected with alpha vs. delta SARS-CoV-2 variants. Wien Klin Wochenschr 134, 850–855 (2022). https://doi.org/10.1007/s00508-022-02084-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-022-02084-1