Summary
The potential mid-term and long-term consequences after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections are as yet unknown. This is the first report of bronchoscopically verified organizing pneumonia as a complication of coronavirus disease 2019 (Covid19). It caused persisting dyspnea, impaired pulmonary function, and radiological abnormalities over 5 weeks after onset of symptoms. While organizing pneumonia frequently requires treatment with systemic corticosteroids, in this case it resolved spontaneously without treatment after 6 weeks. Healthcare professionals should consider organizing pneumonia in patients with persisting respiratory symptoms after Covid19.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
The ongoing Covid-19 pandemic causes a huge burden to healthcare providers worldwide [1, 2]. The potential mid-term and long-term clinical consequences for patients after Covid-19 infections are as yet unknown. Radiological studies and clinical courses have indicated possible organizing pneumonia as a consequence of Covid19 pneumonia [3, 4]. Establishing a histological diagnosis of suspected organizing pneumonia is important as it frequently requires treatment with systemic corticosteroids [5]. We report one of the first case of histologically verified organizing pneumonia in a patient with Covid19 pneumonia.
Case description
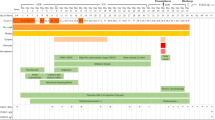
A 49-year-old previously healthy man had fever up to 39 °C and a dry cough starting on 22 March 2020. Prior to that a family member had experienced similar symptoms after spending time in northern Italy, which was considered the European SARS-CoV‑2 hotspot at that time. A pharyngeal swab for PCR was not obtained since he did not fulfil the case definition during that point of time. His family physician treated him with penicillin.
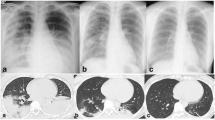
His fever disappeared but he remained substantially short of breath during minor exertion. Suspecting Covid19 he saw a pulmonologist on 15 April. Physical findings were unremarkable and the chest X‑ray showed interstitial opacities with subpleural reticular densities predominantly in the lower fields (Fig. 1). On 20 April the computed tomography (CT) scan showed subpleural patchy ground glass opacities predominantly in the upper lobes (Fig. 2). The lower lobes in addition to ground glass showed arcade-like bands of parenchymal consolidation, peribronchial consolidation and mild bronchiolectasis (Fig. 3). The CT pattern was suggestive of organizing pneumonia. He was referred to the pneumology department for further diagnostic work-up.
On 22 April pulmonary function tests showed a borderline restrictive ventilatory defect (total lung capacity 82%) without evidence of airflow obstruction. Diffusion capacity of the lung for carbon monoxide (DLCO) was reduced (59%) and blood gases showed mild hypoxemia with substantial hypocapnia (arterial partial pressure of oxygen [paO2] 65 mm Hg, arterial partial pressure of carbon dioxide [paCO2] 28 mm Hg, alveolararterial difference in partial pressure of oxygen [AaDO2] 51 mm Hg). Blood tests were normal apart from mildly elevated alanine aminotransferase and gamma-glutamyl transferase. The SARS-CoV‑2 PCR from a nasopharyngeal swab was negative. Serum neutralizing antibodies against SARS-CoV‑2 were positive proving the suspected Covid19 infection.
On 27 April bronchoscopy was performed with the patient under general anesthesia. Endobronchial findings were normal. Bronchoalveolar lavage from the middle lobe showed 41% alveolar macrophages and 59% lymphocytes. T cells were minimally elevated and the CD4/CD8 ratio was normal. Activated T cells and natural-killer-like T cells were substantially elevated (19% and 25% of lymphocytes, respectively). Bacterial culture and SARS-CoV‑2 PCR from the lavage were negative. Cytology obtained by endobronchial ultrasound-guided biopsy of a mildly enlarged subcarinal lymph node showed normal lymphocytes. Lung histology obtained by fluoroscopy-guided transbronchial biopsy from the right lower lobe demonstrated granulation tissue in the alveoli and bronchioles, typical of organizing pneumonia (Fig. 4).
At the follow-up visit on 4 May originally intended to discuss potential treatment options following histological verification of organizing pneumonia, the patient reported substantial spontaneous improvements in well-being and dyspnea, prompting repeated functional assessments. Compared to previous testing lung volumes were normalized (TLC 98%) and gas exchange improved (DLCO 70%, paO2 81 mm Hg, paCO2 29 mm Hg, AaDO2 33 mm Hg). Chest X‑ray findings were also substantially improved (Fig. 1). Given the patients current clinical and functional status consensual agreement was made not to treat with systemic corticosteroids. Follow-up by chest X‑ray and pulmonary function tests were scheduled. The final diagnosis was organizing pneumonia following Covid19.
Discussion
Radiological changes during Covid19 pneumonia peak around 10 days after onset of symptoms and gradually decrease thereafter [6,7,8]. Ground glass opacities are predominant upon onset of symptoms and progressively transform into multifocal consolidation with septal thickening [9,10,11]. This radiomorphological course is indicative for an evolution towards organizing pneumonia, which is a common response to lung injury [12].
Organizing pneumonia is characterized by proliferation of granulation tissue in the alveoli or alveolar ducts, with or without obliteration of distal bronchioles [5]. It can occur without an apparent cause (cryptogenic organizing pneumonia) or as a consequence of viral infections including influenza, severe acute respiratory syndrome coronavirus 1 (CoV-1) and Middle East respiratory syndrome [13,14,15,16,17,18,19,20] as well and many other underlying causes [5]. Clinical and radiological features point towards the diagnosis, which is verified by surgical or transbronchial lung biopsy [21, 22]. The clinical and radiological course of organizing pneumonia is highly variable, ranging from mild with spontaneous remission to progressive and relapsing [22]. Patients with organizing pneumonia frequently require treatment with systemic corticosteroids. So far organizing pneumonia following Covid19 has been suspected on a radiological basis and has been found in post-mortem studies [23, 24]. One case report described organizing pneumonia following Covid19 diagnosed by thoracoscopic lung biopsy [25]. To our knowledge this is the first short report of bronchoscopically verified organizing pneumonia following Covid19.
Prognosis and response to treatment in organizing pneumonia following Covid19 is so far unknown. Since corticosteroid use might be associated with increased mortality in patients with acute coronavirus pneumonia [26] histological verification of suspected organizing pneumonia seems mandatory.
Conclusion
This is one of the first reports of organizing pneumonia as a complication of Covid19. It was the cause of persisting dyspnea, impaired pulmonary function, and radiological abnormalities 5 weeks after onset of symptoms. It improved spontaneously without treatment 6 weeks after the first symptoms. Healthcare professionals should consider organizing pneumonia in patients with persisting respiratory symptoms after Covid19.
References
Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049–55.
Zhang Y, Xu J, Li H, Cao BA. Novel Coronavirus (COVID-19) outbreak: a call for action. Chest. 2020;157(4):e99–e101.
Hani C, Trieu NH, Saab I, et al. COVID-19 pneumonia: a review of typical CT findings and differential diagnosis. Diagn Interv Imaging. 2020;101(5):263–8.
Kory P, Kanne JP. SARS-CoV‑2 organising pneumonia: ‘Has there been a widespread failure to identify and treat this prevalent condition in COVID-19? BMJ Open Respir Res. 2020;7(1), https://doi.org/10.1136/bmjresp-2020-000724.
Cordier JF. Cryptogenic organising pneumonia. Eur Respir J. 2006;28(2):422–46.
Pan F, Ye T, Sun P, et al. Time course of lung changes on chest CT during recovery from 2019 novel Coronavirus (COVID-19) pneumonia. Radiology. 2020;295(3):715–21.
Huang L, Han R, Ai T, et al. Serial quantitative chest CT assessment of COVID-19: deep-learning approach. Radiology. 2020;2(2):e200075.
Rubin GD, Ryerson CJ, Haramati LB, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner society. Chest. 2020;158(1):106–16.
Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus disease 2019 (COVID-19): a systematic review of imaging findings in 919 patients. AJR Am J Roentgenol. 2020;1:7.
Wang Y, Dong C, Hu Y, et al. Temporal changes of CT findings in 90 patients with COVID-19 pneumonia: a longitudinal study. Radiology. 2020;296(2):E55–E64.
Chua F, Armstrong-James D, Desai SR, et al. The role of CT in case ascertainment and management of COVID-19 pneumonia in the UK: insights from high-incidence regions. Lancet Respir Med. 2020;8(5):438–40.
Kligerman SJ, Franks TJ, Galvin JR. From the radiologic pathology archives: organization and fibrosis as a response to lung injury in diffuse alveolar damage, organizing pneumonia, and acute fibrinous and organizing pneumonia. Radiographics. 2013;33(7):1951–75.
Asai N, Yokoi T, Nishiyama N, et al. Secondary organizing pneumonia following viral pneumonia caused by severe influenza B: a case report and literature reviews. BMC Infect Dis. 2017;17(1):572.
He H, Wang H, Li X, Tang X, Sun B, Tong Z. Successful management of refractory respiratory failure caused by avian influenza H7N9 and secondary organizing pneumonia: a case report and literature review. BMC Infect Dis. 2019;19(1):671.
Tse GM, To KF, Chan PK, et al. Pulmonary pathological features in coronavirus associated severe acute respiratory syndrome (SARS). J Clin Pathol. 2004;57(3):260–5.
Hsiao CH, Wu MZ, Chen CL, et al. Evolution of pulmonary pathology in severe acute respiratory syndrome. J Formos Med Assoc. 2005;104(2):75–81.
Hwang DM, Chamberlain DW, Poutanen SM, Low DE, Asa SL, Butany J. Pulmonary pathology of severe acute respiratory syndrome in Toronto. Mod Pathol. 2005;18(1):1–10.
Lai RQ, Feng XD, Gu YY, et al. Pathological changes of lungs in patients with severity acute respiratory syndrome. Zhonghua Bing Li Xue Za Zhi. 2004;33(4):354–7.
Kim I, Lee JE, Kim K‑H, Lee S, Lee K, Mok JH. Successful treatment of suspected organizing pneumonia in a patient with Middle East respiratory syndrome coronavirus infection: a case report. J Thorac Dis. 2016;8(10):E1190–E4.
Lee N, Hui D, Wu A, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. 2003;348(20):1986–94.
King TEJ. Organizing pneumonia. In: Schwarz MK, King TE Jr, editors. Interstitial lung disease. 5th ed. Shelton: People’s Medical Publishing House; 2011. p. 981.
Bradley B, Branley HM, Egan JJ, et al. Interstitial lung disease guideline: the British Thoracic Society in collaboration with the Thoracic Society of Australia and New Zealand and the Irish Thoracic Society. Thorax. 2008;63(Suppl 5):v1–v58.
Okamori S, Lee H, Kondo Y, et al. Coronavirus disease 2019-associated rapidly progressive organizing pneumonia with fibrotic feature: Two case reports. Medicine. 2020;99(35):e21804–e21804.
Flikweert AW, Grootenboers MJJH, Yick DCY, et al. Late histopathologic characteristics of critically ill COVID-19 patients: Different phenotypes without evidence of invasive aspergillosis, a case series. J Crit Care. 2020;59:149–55.
Bae I‑G, Hong K‑W, Yang JW, Moon K, Duk JK, Ju S, et al. Persistent pneumonic consolidations due to secondary organizing pneumonia in a patient recovering from COVID-19 pneumonia: A case report. research square. 2020; https://doi.org/10.21203/rs.3.rs-37580/v1
Yang Z, Liu J, Zhou Y, Zhao X, Zhao Q, Liu J. The effect of corticosteroid treatment on patients with coronavirus infection: a systematic review and meta-analysis. J Infect. 2020;81(1):e13–e20, https://doi.org/10.1016/j.jinf.2020.03.062.
Acknowledgements
The authors thank Michael Schleicher and Dr. Lim for language editing.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Contributions
G.-C. Funk, B. Thaler, C. Nell and G. Rainer wrote the case report. W. Pokieser contributed histology. A. Valipour reviewed and critically checked the text. G.-C. Funk is the guarantor of the paper, taking responsibility for the integrity of the work as a whole from inception to published article.
Corresponding author
Ethics declarations
Conflict of interest
G.-C. Funk, C. Nell, W. Pokieser, B. Thaler, G. Rainer and A. Valipour report no conflict of interest and have read and approved the submission.
Ethical standards
The patient gave informed consent for publication of this case. Anonymity is ascertained. Ethics committee approval was waived.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Funk, GC., Nell, C., Pokieser, W. et al. Organizing pneumonia following Covid19 pneumonia. Wien Klin Wochenschr 133, 979–982 (2021). https://doi.org/10.1007/s00508-021-01852-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-021-01852-9