Summary
Background
Potential additive effects of polypharmacy are rarely considered in adverse events of geriatric patients living in long-term care facilities. Our aim, therefore, was to identify adverse events in this setting and to assess plausible concomitant drug causes.
Methods
A cross-sectional observational study was performed in three facilities as follows: (i) adverse event identification: we structurally identified adverse events using nurses’ interviews and chart review. (ii) Analysis of the concomitantly administered drugs per patient was performed in two ways: (ii.a) a review of summary of product characteristics for listed adverse drug reactions to identify possible causing drugs and (ii.b) a causality assessment according to Naranjo algorithm.
Results
(i) We found 424 adverse events with a median of 4 per patient (range 1–14) in 103 of the 104 enrolled patients (99%). (ii.a) We identified a median of 3 drugs (range 0–11) with actually occurring adverse events listed as an adverse drug reaction in the summary of product characteristics. (ii.b) Causality was classified in 198 (46.9%) of adverse events as “doubtful,” in 218 (51.2%) as “possible,” in 7 (1.7%) as “probable,” and in 1 (0.2%) adverse event as a “definitive” cause of the administered drugs. In 340 (80.2%) of all identified adverse events several drugs simultaneously reached the highest respective Naranjo score.
Conclusion
Patients in long-term facilities frequently suffer from many adverse events. Concomitantly administered drugs have to be frequently considered as plausible causes for adverse events. These additive effects of drugs should be more focused in patient care and research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Geriatric patients in long-term care (LTC) facilities are multimorbid and, therefore, suffer from many (non)specific symptoms and geriatric syndromes [1]. Disease-related symptoms should be distinguished from adverse drug reactions (ADR) that result from drug therapy [2]. The latter can lead to hospital admissions and have a considerable impact on morbidity and mortality with high costs in the health care system [3,4,5]. Polypharmacy makes a significant contribution to the clinical consequences deriving from ADRs in geriatric patients [6]. For this reason, a structured analysis of adverse events (AE) and drug-related causes in these patients is of high interest for routine care.
Distinguishing whether an observed AE was caused by a disease (i.e. symptom) or by a drug (ADR) poses a challenge for healthcare professionals [7, 8]. The correct attribution is required for appropriate treatment strategies but can result only from structured detection, analysis and classification. Geriatric patients are frequently cognitively impaired or suffer from speech or hearing disorders. Hence, information provided by the patients is often insufficient. In LTC facilities, therefore, chart documentation and nurses’ interviews are the most valuable sources for AE detection [9, 10]. So far, no specific method exists to analyze and classify AE in LTC facility residents with polypharmacy. The Naranjo algorithm has previously been used for causality assessment in this collective [11, 12]. It allows a detailed assessment of every detected AE and every single administered drug. This algorithm provides further information on drug-related causes when combined with established methods for patient safety, such as drug-drug interactions and potentially inappropriate medications [13].
Causality scores like the Naranjo score, however, do not consider simultaneously contributing drugs. For some ADRs, it has been shown that the number of specific drugs causes their clinical manifestations. For example, patients are exposed to an increased risk of falling when they take two or more drugs which increase the risk of falling [14]. Concerning anticholinergic ADRs, it is common to calculate an anticholinergic burden to quantify the risk for an adverse outcome [15]. Little is known, however, about additive drug effects in other events. Therefore, data about potential additive effects in this vulnerable patient collective are of great interest for routine care.
The aim of this study was to identify AEs occurring in LTC facility patients and to assess plausible concomitant drug causes.
Patients, material and methods
Definitions
We defined an AE as an outcome that occurs while a patient is taking a drug, but is not or not necessarily attributable to it and an ADR as an appreciably harmful or unpleasant reaction, resulting from an intervention related to the use of a medicinal product [16]. We used the term drug not only for the effective substance but for the whole product prescribed in the medication chart of the patient. A drug therefore could contain more than one active substance. We considered all drugs administered to the patient during the acquisition period. Continuous and on-demand medications were assessed separately because the temporal relationship between AE and administration of the drug could be different in that case.
Participants and setting
We conducted a cross-sectional observation study in three LTC facilities in Germany. After written informed consent of the residents or their legal representative and the responsible general practitioner, residents in the participating LTC facilities were enrolled in the study. We included residents of facilities with different ownerships (welfare, municipal or private associations) to approach a representative sample of 100 residents. Inclusion criteria were: informed consent, age ≥65 years, long-term/chronic medicines ≥3 and multimorbidity with ≥3 comorbidities at the time of recruitment, more than 8 weeks stay in the LTC facility, and a life expectancy of more than 6 months according to nurses’ present information. The study was conducted over a time period of 10 months.
Study design and data collection
We conducted a structured analysis of AEs.
(i) AE identification
We used two complement sources of information for our structured data collection: Firstly, an interview about individual AEs with nurses involved in daily care and, secondly, a review of residents’ records (electronic and chart documentation, laboratory values) for documented events and their temporal occurrence. To ensure standardized identification of AEs, a checklist of events was applied to both methods. The listed events comprised the most relevant AEs or ADRs for geriatric patients and LTC residents based on the literature [17,18,19]: blackened stool, bleeding/hematoma, confusion/disorientation, constipation, depression/anxiety, diarrhea, dizziness/vertigo, dry mouth, ear disorders, eye disorders, falls, hallucination, hyperglycemia/hypoglycemia, hyperhidrosis, hyperkalemia/hypokalemia, hypernatremia/hyponatremia, nausea, pain, restlessness, skin disorders/pruritus, insomnia, urinary incontinence, vomiting (in alphabetical order). Additional relevant reported or documented events were collected as well. We considered reported and documented symptoms during a time period of the prior 30 days (considered as 1 resident month) for new and continuous symptoms. Data collection was performed at two measurement points per patient at intervals of 6–8 weeks by two clinical pharmacists. All detected AEs and the corresponding system organ class were classified based on the common terminology criteria for adverse events (CTCAE) [20].
(iia) Review of summary of product characteristics
We systematically collected data from the medical charts (continuous drugs, on demand drugs and their frequency of use, date of first administration). We checked all summaries of product characteristics (SmPCs) of the actually administered drugs for listed ADRs. A drug would be considered as “potentially causing” if the listed ADR in the SmPC represented a synonym for the detected AE or possibly caused it (e.g. dizziness in cases of falls). For the analysis of additive effects, we counted the number of potentially causing drugs. Prescribed drugs were characterized by their code in the anatomical therapeutic chemical classification system (ATC code).
(iib) Causality assessment according to the Naranjo algorithm
We used the Naranjo algorithm for causality assessment. All further relevant information, such as the duration of the AE, underlying diseases, clinical consequences (e.g. from hospital report), laboratory values, and patient-specific conditions were collected and used to determine the Naranjo score. The most likely associated drugs were the ones that reached the highest Naranjo score concerning the single analyzed AE. Naranjo distinguishes between definitive with a total score ≥9, probable with 5 < total score < 8, possible with 1 < total score < 4 and doubtful with a total score ≤ 0 [21, 22].
Inconclusive evaluations in all steps (i, ii.a, and ii.b) were discussed and finalized by mutual agreement in an expert panel. This panel consisted of four experienced clinical pharmacists.
Statistical analysis
To ensure comparable patient parameters between the three LTC facilities independent of the allocation to a single facility, main patient parameters were statistically analyzed. For this purpose, a Kruskal Wallis test with pairwise comparison was performed. Analyzed parameters were age, gender, number of diagnoses and number of continuous and on demand drugs, as well as the number of AEs in the patients and the maximum Naranjo score per patient. The data analysis was performed using IBM SPSS Statistics Version 25.0 (IBM Corporation, Armonk, NY, USA) and Microsoft Office Excel 2013 (Microsoft Corporation, Redmond, WA, USA). P-values ≤ 0.05 were considered as statistically significant.
Results
Patient characteristics
In the participating parts of the LTC facilities, 182 patients were potentially available for the study and 154 met the inclusion criteria. From these, 104 patients or their legal guardian gave their informed consent as well as their responsible physician and were enrolled in the study. Patients were mostly female (72.1%) and in median 86 (range: 66–101) years old (Table 1). Patients did not differ between the three LTC facilities according to the following parameters: age (p = 0.311), gender (p = 0.684), number of diagnoses (p = 0.070) and number of continuous (p = 0.629) and on demand drugs (p = 0.911).
(i) AE identification
From a total of 104 patients, at least 1 AE was identified in 103 (99.0%). We identified 424 AEs, with a detected median of 4 (Q25/Q75: 2/5, range 1–14) AEs per patient, which equals 2.05 AEs per resident month. The identified AEs and the number of affected patients are shown in Table 2. The system organ classes renal and urinary disorder (87 patients), gastrointestinal disorder (43 patients), skin and subcutaneous tissue disorders (37 patients) were most common in our patient collective. Altogether, 72 different AE categories were detected, 185 AEs were identified in the patient records and 195 AEs by the nurses’ interviews, with 44 AEs in concordance of both methods. We found a significant difference in the detected number of AEs between the observed LTC facilities (p = 0.020). Following the pairwise comparison, we only found differences between the municipal LTC facility with 3 (Q25/Q75: 2/4) AEs and the private LTC facility with a median of 4 (Q25/Q75: 3/6.25) AEs (p = 0.022).
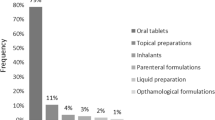
(ii.a) Review of summary of product characteristics
To analyze the concomitantly administered drugs, we assessed 3725 combinations of AEs and corresponding drugs. For this analysis five drug/AE pairs had to be excluded because no information from the SmPC was available (moisturizing eye drops, medical device). Considering every identified AE, patients had a median of 3 potentially causing drugs according to the SmPC, with a range from 0 to 11 drugs (Q25/Q75: 2/4; details in Fig. 1). The most frequently (n ≥ 10) detected AEs and the affected system organ classes are shown in Table 3. The ATC classes prescribed most often (C, N, A, B, H) were frequently among the potentially causing drugs for the most common system organ classes (Fig. 2).
Potentially causing drugs according Summary of Product Characteristics differentiated into the ATC classes for the most frequently detected system organ classes. AE(s) adverse event(s), ATC anatomical therapeutic chemical/defined daily dose classification, CTCAE common criteria for the terminology of adverse events, SmPC summary of products characteristics. ATC classes: A: alimentary tract and metabolism, B: blood and blood forming organs, C: cardiovascular system, H: systemic hormonal preparations, excluding sex hormones and insulins, N: nervous system
(ii.b) Causality assessment according to the Naranjo algorithm
All 3730 drug/AE pairs were included in the causality assessment. From the 424 identified AEs, 198 (46.9%) were classified as ADR with “doubtful”, 218 (51.2%) “possible”, 7 (1.7%) “probable”, and 1 (0.2%) “definitive” cause (Table 4). We found no significant differences in the maximum Naranjo scores per patient between the three LTC facilities (p = 0.964). On the basis of 424 detected AEs, only 1 drug in 84 AEs (19.8%) and several drugs in 340 AEs (80.2%) reached the highest score (Table 4). According to Naranjo these need to be considered as the most likely causing drug(s).
The probable and definitive ADRs were as follows: angioedema (severity grade according to CTCAE 4) induced by enalapril, urticaria (grade 2) induced by amoxicillin and clavulanic acid, hypoglycemia (grade 1) induced by insulin glargine, paresthesia (grade 2) induced by tapentadol and a complex case of occurring hallucinations (grade 3) in combination with confusion (grade 3), dizziness (grade 3) and somnolence (grade 3, in total 4 detected AEs) which were attributable to digitoxin (highest Naranjo score). In this case, the patient also received high doses of oxycodone and duloxetine. It can be seen as a mixed intoxication based on the hospital report. In the algorithm, digitoxin reached a one-point higher score than oxycodone/duloxetine because measurement of the increased blood level was available only for digitoxin.
All of the detected AEs and ADRs were managed adequately by the nurses, for example, by informing a physician or arranging a hospital admission for the affected patient. Thus, no further action was required due to this study.
Discussion
In our study we addressed AEs in geriatric patients living in LTC facilities. We assessed which type of AEs occurred and also investigated potential additive effects of polypharmacy. With nearly all (99%) patients affected by AEs, we demonstrated the relevance of this topic. We found the identified AEs potentially caused by up to 11 different administered drugs. The Naranjo algorithm showed at least possible drug causes in half of these AEs. Thereby, multiple drugs were equally likely involved 80% of the time. Our results point out that AEs should be systematically recorded in routine practice in LTC facilities. In order to prevent ADRs, additive effects need to be considered in any strategies developed.
Prevalence of AE and ADR in LTC residents
More than half of our identified AEs could be associated with drug use. Our rate of probable and definitive ADRs was similar to other studies in the LTC setting (0.04 vs. up to 0.10 ADRs per observed resident month), although studies should be compared with caution [9, 23]. Nevertheless, the causality assessment leaves us with a high number of possible ADRs. Especially for AEs which were ongoing for a longer period, causality assessment was challenging in the routine setting. Information to evaluate the exact temporal connection between AE and drug use was frequently missing and therefore could have led to lower Naranjo scores. To resolve this problem, a regular and structured routine assessment of AEs and potentially causing drugs might increase the chance to identify ADRs and protect patients from the consequences.
Our overall rate of identified AEs was higher than results seen in other studies (2.05 AEs vs 0.03–0.12 per observed resident month) [9, 23]. This indicates that we identified a noticeable amount of the general symptom burden of LTC residents that results from underlying diseases or age-related changes. This is consistent with the fact that incontinence, pain, sleep disorders and psychopathological symptoms are widely found in LTC residents [24]. Therefore, a regular routine AE assessment can support ADR detection as well as structured symptom evaluation.
Additive effects of polypharmacy
The suspected AE was listed as an ADR in the respective SmPC in a median of 3 and up to 11 administered drugs per patient. In 80% of all identified AEs, various drugs reached the highest Naranjo score simultaneously. This means that they were equally likely to cause the AE. This coincidence can increase the chance of AE occurrence independently from single causality scores. This result also raises the question whether ADRs resulting from additive effects have been underestimated. In cases with “probable” or “definitive” ADRs (Naranjo ≥5), we found results from only one drug with the highest Naranjo score; however, in four of these AEs, the drug with the highest Naranjo (digitoxin) was only part of a mixed intoxication with duloxetine and oxycodone based on the hospital report for the affected patient. In this case, the sole consideration of the causality assessment could mask an additive effect of at least 3 concomitantly given drugs. This shows that additive effects need to be considered in every detected AE independently from the single causality. Besides ADRs from well-known drug classes (e.g. vascular ADRs from drugs affecting blood and blood-forming organs), in a substantial amount of AEs, we found involvement of varying ATC-classes that are less familiar (e.g. nervous system ADRs in drugs affecting the cardiovascular system). This underlines the complexity of geriatric patient treatment and the need for interdisciplinary medication reviews that include an assessment of drug-related problems, such as drug-drug interactions, potentially inappropriate medication, as well as ADRs [25, 26]. In routine care, however, potential additive effects are often not taken into account. In particular, new and unclear symptoms could be misinterpreted as new diseases and sometimes even lead to prescribing cascades [27, 28].
Implications for practice
Firstly, our study shows the need for a good data base and a regular routine assessment of AEs that occur in LTC facilities. We found a very low concordance rate of only 10% between AEs detected in nurses’ interviews and those mentioned in the patient record analysis. This demonstrates the potential of information loss in LTC facilities due to heterogeneous and incomplete AE documentation [29]. It also indicates the potential of recall bias in the nurses. The identification of every occurring AE allows a better assessment of simultaneously occurring events. We found in our study, for example, a combination of vomiting and diarrhea that indicated an infection rather than an ADR. Furthermore, the information on patients’ current symptoms contributes to appropriate proposals for medication changes in cases of identified ADRs.
Secondly, our results support the development of strategies with improved consideration of the additive effects of polypharmacy. Combining an AE assessment with structured medication reviews improves the drug cause analysis of AEs as well as the detection and interpretation of drug-related problems. Ongoing prospective evaluation of AEs and potential drug-related causes contributes to prevent patients from experiencing negative events. This process could be further accelerated by electronic assistance. Electronic documentation of AEs and computer-assisted signal detection of ADRs can support problem solving in a narrow timeframe since physicians and pharmacists are usually not permanently present in the LTC facilities [11, 30]. Database-supported comparison of the events with patients’ medication can assist pharmacists in a comprehensive medication review. Currently, such electronic solutions are rarely used in the LTC setting in Germany. They could also support future research by providing information on the additive effects of various combined drugs and underlying diseases.
Thirdly, our data suggest the need for improvement in interdisciplinary communication in LTC facilities. In interprofessional teams with nurses, pharmacists and physicians, systematic information about AEs, medication reviews and actual health conditions could be transmitted more effectively in patient-orientated practice.
Conclusion
Nearly every long-term care resident suffered from adverse events (AEs), with half of them at least possibly caused by drugs. In four fifths of these AEs, several concomitantly given drugs were equally associated causes. Therefore, potential additive effects need to be considered independently from single causality and should be more focused in further research. A routinely implemented structured search for AEs and additive effects of polypharmacy contributes to medication reviews and interdisciplinary collaboration and will help to meet the needs of this complex patient collective and to protect them from negative consequences.
References
Gordon AL, Franklin M, Bradshaw L, Logan P, Elliott R, Gladman JR. Health status of UK care home residents: a cohort study. Age Ageing. 2014;43(1):97–103.
Wierenga PC, Buurman BM, Parlevliet JL, et al. Association between acute geriatric syndromes and medication-related hospital admissions. Drugs Aging. 2012;29(8):691–9.
Chan M, Nicklason F, Vial JH. Adverse drug events as a cause of hospital admission in the elderly. Intern Med J. 2001;31(4):199–205.
Schneeweiss S, Hasford J, Göttler M, Hoffmann A, Riethling AK, Avorn J. Admissions caused by adverse drug events to internal medicine and emergency departments in hospitals: a longitudinal population-based study. Eur J Clin Pharmacol. 2002;58(4):285–91.
Kongkaew C, Hann M, Mandal J, et al. Risk factors for hospital admissions associated with adverse drug events. Pharmacotherapy. 2013;33(8):827–37.
Field TS, Gurwitz JH, Avorn J, et al. Risk factors for adverse drug events among nursing home residents. Arch Intern Med. 2001;161(13):1629–34.
Bäckström M, Mjörndal T, Dahlqvist R. Spontaneous reporting of adverse drug reactions by nurses. Pharmacoepidemiol Drug Saf. 2002;11(8):647–50.
Hohl CM, Robitaille C, Lord V, et al. Emergency physician recognition of adverse drug-related events in elder patients presenting to an emergency department. Acad Emerg Med. 2005;12(3):197–205.
Gurwitz JH, Field TS, Avorn J, et al. Incidence and preventability of adverse drug events in nursing homes. Am J Med. 2000;109(2):87–94.
Morimoto T, Gandhi TK, Seger AC, Hsieh TC, Bates DW. Adverse drug events and medication errors: detection and classification methods. Qual Saf Health Care. 2004;13(4):306–14.
Handler SM, Hanlon JT, Perera S, et al. Assessing the performance characteristics of signals used by a clinical event monitor to detect adverse drug reactions in the nursing home. AMIA Annu Symp Proc. 2008;6:278–82.
Carnovale C, Gentili M, Fortino I, et al. The importance of monitoring adverse drug reactions in elderly patients: the results of a long-term pharmacovigilance programme. Expert Opin Drug Saf. 2016;15(2):131–9.
Lavan AH, Gallagher P. Predicting risk of adverse drug reactions in older adults. Ther Adv Drug Saf. 2016;7(1):11–22.
Schiek S, Hildebrandt K, Zube O, Bertsche T. Fall-risk-increasing adverse reactions-is there value in easily accessible drug information? A case-control study. Eur J Clin Pharmacol. 2019;75(6):849–57.
Salahudeen MS, Duffull SB, Nishtala PS. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatr. 2015;15:31.
Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet. 2000;356(9237):1255–9.
Handler SM, Hanlon JT, Perera S, et al. Consensus list of signals to detect potential adverse drug reactions in nursing homes. J Am Geriatr Soc. 2008;56(5):808–15.
Thürmann P, Jaehde U. Drug therapy safety in nursing homes: cross-sectional analysis and feasibility of a multidisciplinary approach. Final report federal ministry of health. 2011. https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/5_Publikationen/Gesundheit/Berichte/Abschlussbericht_Arzneimitteltherapiesicherheit_in_Alten-_und_Pflegeheimen_Querschnittsanalyse_und_Machbarkeit_eines_multidisziplinaeren_Ansatzes.pdf. Accessed 20 Jan 2020.
Härkänen M, Kervinen M, Ahonen J, Voutilainen A, Turunen H, Vehviläinen-Julkunen K. Patient-specific risk factors of adverse drug events in adult inpatients—evidence detected using the global trigger tool method. J Clin Nurs. 2015;24(3–4):582–91.
U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute. Common terminology criteria for adverse events (CTCAE) version 4.03. 2010. https://www.eortc.be/services/doc/ctc/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. Accessed 20 Jan 2020.
Naranjo CA, Busto U, Sellers EM, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30(2):239–45.
Agbabiaka TB, Savović J, Ernst E. Methods for causality assessment of adverse drug reactions: a systematic review. Drug Saf. 2008;31(1):21–37.
Gurwitz JH, Field TS, Judge J, et al. The incidence of adverse drug events in two large academic long-term care facilities. Am J Med. 2005;118(3):251–8.
Elseviers MM, Vander Stichele RR, Van Bortel L. Drug utilization in Belgian nursing homes: impact of residents’ and institutional characteristics. Pharmacoepidemiol Drug Saf. 2010;19(10):1041–8.
Fog AF, Kvalvaag G, Engedal K, Straand J. Drug-related problems and changes in drug utilization after medication reviews in nursing homes in Oslo, Norway. Scand J Prim Health Care. 2017;35(4):329–35.
Halvorsen KH, Stadeløkken T, Garcia BH. A stepwise pharmacist-led medication review service in interdisciplinary teams in rural nursing homes. Pharmacy (Basel). 2019;7(4):148.
Rochon PA, Gurwitz JH. Optimising drug treatment for elderly people: the prescribing cascade. BMJ. 1997;315(7115):1096–9.
Davies EA, O’Mahony MS. Adverse drug reactions in special populations—the elderly. Br J Clin Pharmacol. 2015;80(4):796–807.
Ehrenberg A, Ehnfors M. The accuracy of patient records in Swedish nursing homes: congruence of record content and nurses’ and patients’ descriptions. Scand J Caring Sci. 2001;15(4):303–10.
Forster AJ, Jennings A, Chow C, Leeder C, van Walraven C. Supervised signal detection for adverse drug reactions in medication dispensing data. Comput Methods Programs Biomed. 2018;161:25–38.
Acknowledgements
We thank all participating co-workers of the LTC facilities and the attending physicians for their support. Furthermore, we thank PhD Johanna Freyer for her assistance with the ethics approval and Katharine Worthington for language editing.
Funding
A co-worker of the study (Monika Lexow) was financially supported in part by the Lesmueller Foundation, Munich, Germany, the German Pharmacist Foundation, Berlin, Germany and the Pharmacist Foundation Westfalen-Lippe, Münster, Germany.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conceptualization: Monika Lexow, Kathrin Wernecke, Ralf Sulzer, Thilo Bertsche, Susanne Schiek; methodology: Monika Lexow, Kathrin Wernecke, Thilo Bertsche, Susanne Schiek; formal analysis and investigation: Kathrin Wernecke, Susanne Schiek; investigation: Monika Lexow, Kathrin Wernecke; writing, original draft preparation: Monika Lexow, Kathrin Wernecke, Thilo Bertsche, Susanne Schiek; writing, review and editing: Monika Lexow, Kathrin Wernecke, Ralf Sultzer, Gordian L. Schmid, Thilo Bertsche, Susanne Schiek; visualization: Monika Lexow, Kathrin Wernecke, Susanne Schiek; supervision: Thilo Bertsche, Susanne Schiek; project administration: Monika Lexow; funding acquisition: Thilo Bertsche, Susanne Schiek.
Corresponding author
Ethics declarations
Conflict of interest
M. Lexow, K. Wernecke, G.L. Schmid, R. Sultzer, T. Bertsche, and S. Schiek declare that they have no competing interests.
Ethical standards
All procedures performed in this study involving human participants were approved both by the ethics committee of the Faculty of Medicine of Leipzig University as well as the ethics committee of the State Chamber of Physicians of Saxony (reference: 231/13-ff and EK-allg-26/14-1) and have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. All participants gave their informed consent prior to inclusion in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors M. Lexow and K. Wernecke contributed equally to the manuscript.
The authors T. Bertsche and S. Schiek contributed equally to the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lexow, M., Wernecke, K., Schmid, G.L. et al. Considering additive effects of polypharmacy. Wien Klin Wochenschr 133, 816–824 (2021). https://doi.org/10.1007/s00508-020-01750-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-020-01750-6