Summary
Background
Recent reports have noted increasing rates of anal cancer among high-income countries worldwide; however, little is known about these trends in Austria.
Methods
Data on anal cancer from 1983 to 2016 were obtained from Statistics Austria. All tumors (n = 3567) were classified into anal squamous cell carcinomas (ASCC), anal adenocarcinomas (AADC), and others (unspecified carcinoma and other specific carcinoma). Anal cancer incidence rates were calculated in 5‑year cycles and incidence average annual percentage change (AAPC) to evaluate trends by sex, histology and age group.
Results
The incidence rate of anal cancer was higher among females than males (relative risk, RR = 1.66, 95% confidence interval, CI: 1.55–1.79, p < 0.0001). From 1983 through 2016, incident anal cancer increased significantly (0.92 per 100,000 person-years to 1.85 per 100,000 person-years, AAPC = 1.93, 95% CI: 1.52 to 2.34, p < 0.0001), particularly among those 40–69 years old. From 1983 through 2016, the increasing anal cancer incidence was primarily driven by ASCC (0.47–1.20 per 100,000 person-years, AAPC = 2.23, 95% CI: 1.58 to 2.88, p < 0.0001) and others (other than ASCC and AADC, AAPC = 1.78, 95% CI: 1.01–2.55), yet stable in AADC (AAPC = 0.88, 95% CI: −0.48–2.25).
Conclusions
Despite being a rare cancer in Austria, the increase in anal cancer incidence rate from 1983 to 2016 was substantial, particularly in ASCC. The observed rising trends reflect the need to investigate associated risk factors that have increased over time to inform preventive measures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anal cancer is a relatively uncommon malignancy, accounting for approximately 4% of all cancers of the lower gastrointestinal tract [1]. Worldwide incidence of this cancer is 1–2 per 100,000 person-years in average risk groups, with the incidence being slightly higher for women compared to men [2, 3]. Although rare, reports have shown that incidence has increased in many high-income countries, including Canada, the United States of America [4], Denmark [5], and the United Kingdom [6, 7]. These increases are largely occurring for anal squamous cell carcinomas (ASCC), with smaller changes or decreases for adenocarcinomas (AADC), and the reasons are not entirely clear [2, 8]. Anal cancer has a relatively high mortality rate, with a 5-year survival rate among those diagnosed with stage 4 of below 50% [9]. Therefore, preventing further increases in incidence is imperative to reduce further morbidity and mortality.
The majority of ASCC cases are considered to be caused by human papillomavirus (HPV) infection [10], and risk factors include number of sexual partners, receptive anal intercourse, smoking [8, 10], history of sexually transmitted infections [11], and immune deficiency, i.e. infection with human immunodeficiency virus (HIV) or immunosuppressive drugs [8]. These risk factors are similar for cervical cancer, another malignancy caused by HPV infection [12].
Epidemiological data on anal cancer in Austria is sparse; one published report gives the number of cases between 2008 and 2012 at 230 and 454 for men and women, respectively [12], but the contemporary trends of anal cancer incidence in Austria are unknown. Using the most recent and updated information on anal cancer incidence (1983–2016) from Statistics Austria, the objective of the present analysis was to systematically describe the national cancer incidence rates over more than 30 years.
Methods
Anal cancer cases were defined according to the International Classification of Diseases version (ICD)-10, with code C21 identified as anal cancer from the Austrian Cancer Registry (derived on 19 December 2018). For histological classification, all tumors were classified into three categories based on ICD oncology version 3 (ICD-O-3) codes, per World Health Organization (WHO) category conventions [13]: anal squamous cell carcinoma (ASCC, 8050–8076); anal adenocarcinomas (AADC), and “other” (unspecified carcinoma 8010-8034 and other specified carcinoma, all remaining morphology codes). Age groups were defined in 10-year intervals starting at age 30 years (<30, 30–39, 40–49, 50–59, 60–69, 70–79, 80+ years).
Statistical analyses
Age-specific incidence rates for anal cancer were calculated in 5‑year cycles to obtain a stable estimation (the last cycle contains only 4 years: 2013–2016). Age standardized rates were calculated by year and sex using the European standard population [14].
Average annual percent changes (AAPCs) in incidence were calculated to describe trends from 1983 to 2017. In addition, APCs were described by sex, histology, and age group to identify trends by subgroups. Comparison of crude incidence rates between the years 1983–1987 and 2013–2016 by age and sex was done by the exact Fisher test using SAS version 9.4 (SAS Institute, Cary NC, USA). Time trend analysis and calculation of adjusted incidence rates were done by Joinpoint software (Joinpoint Regression Program, Version 4.7.0.0. February, 2019; Statistical Research and Applications Branch, National Cancer Institute, Bethesda, Maryland, USA). The maximum number of joinpoints was set to two, the minimum number to either side of the end and between joinpoints to two, respectively. A p-value <0.05 was considered to be statistically significant. No adjustment for multiple testing was done therefore p-values are to be interpreted exploratorily only. This study does not require an approval by an institutional review board because only publicly accessible records were used without any contact with individuals.
Results
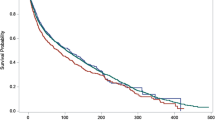
Between 1983 and 2016, a total of 1099 and 2468 cases of anal cancers were identified in males and females, respectively (Table 1). Overall, anal cancer incidence rates increased significantly from 1983 (0.92 per 100,000 person-years) through 2016 (7.84 per 100,000 person-years), with an APC of 1.93 (95% CI 1.5–2.3) (Fig. 1, Supplementary Table 1). The incidence rates of anal cancer were consistently higher among females compared with males (odds ratio, OR 1.66, 95% CI 1.55–1.79), and exhibited increases in both sexes over time (male: 0.35 per 100,000 person-years to 1.50 per 100,000 person-years, APC 1983–1989 of 16.5, 95% CI 2.8–32.0, APC 1989–2016 of 2.0, 95% CI 1.3–2.8; female: 1.30 per 100,000 person-years to 2.39 per 100,000 person-years, APC of 1.9, 95% CI 1.4–2.3).
In subgroups by age, the increase in anal cancer incidence rates was particularly evident among those aged 40–69 years (Figs. 2 and 3, Supplementary Table 2). In the male population, anal cancer incidence rate increased from 0.20 (95% CI 0.03–0.38) to 0.64 (95% CI 0.34–0.94) among 40–49 years age band, increased from 0.35 (95% CI 0.09–0.62) to 2.53 (95% CI 1.91–3.16) among 50–59 years age band, and increased from 0.73 (95% CI 0.28–1.19) to 3.20 (95% CI 2.35–4.04) among 60–69 years age band. In the female population, these increases were from 0.49 (95% CI 0.21–0.77) to 1.17 (95% CI 0.76–1.58) among 40–49 years age band, 1.58 (1.05–2.12) to 4.74 (3.88–5.59) among 50–59 age band, and from 2.38 (95% CI 1.72–3.04) to 5.15 (95% CI 4.12–6.17) among 60–69 years age band. The incidence rates of anal cancer rose in males and females. The increases in each age group appear to be similar, except a significant age and sex interaction (p = 0.03) observed among those 60–69 years old with the annual increase in males exceeding that of females.
Across sub-types of anal cancer, the increasing anal cancer incidence was primarily driven by ASCC (APC 2.23, 95% CI 1.58–2.88) and “others” (neither ASCC nor AADC) (APC 1.78, 95% CI 1.01–2.55), while incidence was stable for AADC (APC 0.88, 95% CI −0.48–2.25).
Discussion
These analyses examined anal cancer incidence trends over more than 30 years in Austria. These trends have not been previously detailed and add further evidence for a global trend of increasing anal cancer rates. Between 1983 and 2016, the age-standardized rate of anal cancer was found to increase by an average of 1.93% per year, with particular increases among those aged 40–69 years. Particularly, the increasing rate of ASCC was driving the overall increase in incidence, while AADC incidence remained relatively stable. In addition, females were more likely to be diagnosed with anal cancer and exhibited higher annual percent changes than males.
These results are in line with other reports from high-income countries. In Australia, incidence of ASCC increased linearly by an APC of 1.6%, with recent decreases in AADC [15]. Larger increases were noted in France, where incidence of ASCC among women increased by 3.4% between 2005 and 2012, and 2.6% among men during the same time period [16]. Changes in incidence in the USA were similar to those in France, with ASCC increasing by 2.9%, and non-significant decreases in AADC [4].
The reasons for the observed trends are speculative, but likely reflect changing behavior related to known risk factors. As mentioned previously, anal HPV infection is believed to be a necessary factor in the development of ASCC, as almost all cases test positive for HPV DNA [17]. The risk of HPV increases with higher number of male sexual partners and receptive anal intercourse [11]. Today, people are more likely to have extramarital sex and have more sexual partners than people in the 1970s, and the prevalence of anal intercourse among heterosexual couples has increased [18]. These practices may have resulted in an increase in population HPV infection, and a subsequent increase in anal cancer incidence.
Another important risk factor for anal cancer is infection with HIV. A meta-analysis from North America found that the incidence ratio of anal cancer comparing those with HIV to those without was 28, and the incidence was as high as 131 per 100,000 individuals among men living with HIV [19]. While the incidence and mortality of HIV infection has decreased dramatically since the introduction of antiretroviral therapies (ART) [20], ART may not reduce the risk of anal cancer among those already with the infection [21]. In fact, longer time living with HIV is associated with increased risk of the cancer [22], unless treatment is initiated early [23]. Despite significant decreases in HIV incidence, people living with this infection are a high-risk group for anal cancer and should remain a priority for both primary and secondary prevention.
It is possible that these increasing trends may reverse when younger generations reach an age when anal cancer is usually diagnosed. The widespread use of HPV vaccination [9], participation in screening programs [24], and a changing sexual culture [25] may contribute to a reduction in anal cancer incidence in the future. Additionally, the reductions in new HIV infections [20] and global reductions in tobacco smoking [26] may also place younger generations at lower risk for anal cancer. Primary prevention with the HPV vaccine will continue to be important in reducing the incidence of anal cancer. In Austria, routine vaccination began in 2014 for boys and girls starting at the age of 9 years, but vaccination coverage is not currently known [12]. In the USA, the Advisory Committee on Immunization Practices recommended use of the quadrivalent HPV vaccine for prevention of anal cancer [27]. This vaccine was shown to protect against precancerous anal epithelial cells, particularly among high-risk groups, and risk of persistent infection was dramatically reduced [28]. These results show that HPV vaccination is an important tool in the prevention of anal cancer development, and higher rates of uptake are required.
Organized screening programs using Pap-tests for cervical cancer are widespread; coverage with Austria’s program ranges from 70–76% depending on the region [12]. While there is no established program for anal cancer screening, results from a recent pooled report suggest that data collected at cervical cancer screening can be used to identify women who should be screened for anal cancer [29]. In this study, 41% of immunocompetent women with cervical HPV-16 also had anal HPV-16, compared to only 2% who did not have the cervical strain. Therefore, high-risk cervical HPV appears to be a determinant for anal cancer risk, and routine cervical cancer screening could be used as a prevention tool for anal cancer as well [24].
Another possible reason for the increase of incidence of anal cancer is implementation of colorectal cancer screening programs, because the anus is also investigated during colonoscopy [30]. In Austria, an opportunistic colorectal screening program with primary screening colonoscopy was implemented in 2015. Therefore, the rise in anal cancer diagnosis in the last decade might be due to implementation of colorectal cancer screening programs.
These results, showing increasing anal cancer incidence in Austria, provide further evidence of a broader trend among high-income countries. Although rare, anal cancer has a relatively high mortality rate, and may have long-lasting health consequences for those who survive the disease [31]. Despite these alarming observations, anal cancer benefits from being a preventable disease in most cases. Widespread HPV vaccination among boys and girls, as well as comprehensive sexual education, including information about screening for HPV-related diseases may be critical in reducing incidence. Additionally, anal cancer and other HPV-related cancers should continue to be a focus of care among high-risk groups, including those living with HIV. Further research should also be conducted on determinants of progression from anal HPV to cancer, and possible biomarkers associated with progression. Trends in anal cancer should be continually monitored to identify any other target groups that may warrant closer surveillance or prevention efforts.
Key points
-
Between 1983 and 2016 the age-standardized rate of anal cancer increased by an average of nearly 2% per year.
-
Females were more likely to be diagnosed with anal cancer and exhibited higher annual percent changes than males.
-
The increasing anal cancer incidence was primarily driven by anal squamous cell carcinomas and “others” but stable in adenocarcinomas.
References
Clark MA, Hartley A, Geh JI. Cancer of the anal canal. Lancet Oncol. 2004;5(3):149–57.
Islami F, Ferlay J, Lortet-Tieulent J, Bray F, Jemal A. International trends in anal cancer incidence rates. Int J Epidemiol. 2017;46(3):924–38.
Plummer M, de Martel C, Vignat J, Ferlay J, Bray F, Franceschi S. Global burden of cancers attributable to infections in 2012: a synthetic analysis. Lancet Glob Health. 2016;4(9):e609–16.
Shiels MS, Kreimer AR, Coghill AE, Darragh TM, Devesa SS. Anal cancer incidence in the United States, 1977–2011: distinct patterns by histology and behavior. Cancer Epidemiol Biomarkers Prev. 2015;24(10):1548–56.
Nielsen A, Munk C, Kjaer SK. Trends in incidence of anal cancer and high-grade anal intraepithelial neoplasia in Denmark, 1978–2008. Int J Cancer. 2012;130(5):1168–73.
Brewster DH, Bhatti LA. Increasing incidence of squamous cell carcinoma of the anus in Scotland, 1975–2002. Br J Cancer. 2006;95(1):87–90.
Robinson D, Coupland V, Moller H. An analysis of temporal and generational trends in the incidence of anal and other HPV-related cancers in southeast England. Br J Cancer. 2009;100(3):527–31.
Kang YJ, Smith M, Canfell K. Anal cancer in high-income countries: Increasing burden of disease. PLoS ONE. 2018;13(10):e205105.
Mensah FA, Mehta MR, Lewis JS Jr., Lockhart AC. The human papillomavirus vaccine: current perspective and future role in prevention and treatment of anal Intraepithelial neoplasia and anal cancer. Oncologist. 2016;21(4):453–60.
Daling JR, Madeleine MM, Johnson LG, Schwartz SM, Shera KA, Wurscher MA, et al. Human papillomavirus, smoking, and sexual practices in the etiology of anal cancer. Cancer. 2004;101(2):270–80.
Nelson VM, Benson AB 3rd. Epidemiology of anal canal cancer. Surg Oncol Clin N Am. 2017;26(1):9–15.
Bruni L, Albero G, Serrano B, Mena M, Gomez D, Munoz J, et al. Human papillomavirus and related diseases in the world. Summary report. Barcelona: ICO/IARC Information Centre on HPV and Cancer (HPV Information Centre); 2019.
Parkin D, Shanmugarathnam K, Sobin L, Ferlay J, Whelan S. Histological groups for comparative studies. Lyon: World Health Organization; 1998.
Pace M, Giampaolo L, Glickman M, Zupanic T. evision of the European standard population—report of Eurostat’s task force. Luxembourg: Publications Office of the European Union; 2013.
Soeberg MJ, Rogers K, Currow DC, Young JM. Trends in incidence and survival for anal cancer in New South Wales, Australia, 1972–2009. Cancer Epidemiol. 2015;39(6):842–7.
Bouvier AM, Belot A, Manfredi S, Jooste V, Uhry Z, Faivre J, et al. Trends of incidence and survival in squamous-cell carcinoma of the anal canal in France: a population-based study. Eur J Cancer Prev. 2016;25(3):182–7.
Lin C, Franceschi S, Clifford GM. Human papillomavirus types from infection to cancer in the anus, according to sex and HIV status: a systematic review and meta-analysis. Lancet Infect Dis. 2018;18(2):198–206.
Twenge JM, Sherman RA, Wells BE. Changes in American adults’ sexual behavior and attitudes, 1972–2012. Arch Sex Behav. 2015;44(8):2273–85.
Silverberg MJ, Lau B, Justice AC, Engels E, Gill MJ, Goedert JJ, et al. Risk of anal cancer in HIV-infected and HIV-uninfected individuals in North America. Clin Infect Dis. 2012;54(7):1026–34.
Joint United Nations Programme on HIV/AIDS (UNAIDS). Global AIDS update. Geneva: World Health Organization; 2016.
Lim ST, Levine AM. Non-AIDS-defining cancers and HIV infection. Curr Infect Dis Rep. 2005;7(3):227–34.
Crum-Cianflone NF, Hullsiek KH, Marconi VC, Ganesan A, Weintrob A, Barthel RV, et al. Anal cancers among HIV-infected persons: HAART is not slowing rising incidence. AIDS. 2010;24(4):535–43.
Borges AH, Neuhaus J, Babiker AG, Henry K, Jain MK, Palfreeman A, et al. Immediate antiretroviral therapy reduces risk of infection-related cancer during early HIV infection. Clin Infect Dis. 2016;63(12):1668–76.
Wieland U, Kreuter A. Anal cancer risk: HPV-based cervical screening programmes. Lancet Infect Dis. 2019;19(8):799–800.
Eaton DK, Lowry R, Brener ND, Kann L, Romero L, Wechsler H. Trends in human immunodeficiency virus- and sexually transmitted disease-related risk behaviors among U.S. high school students, 1991–2009. Am J Prev Med. 2011;40(4):427–33.
GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the global burden of disease study 2015. Lancet. 2017;389(10082):1885–906.
Centers for Disease Control and Prevention (CDC). Recommendations on the use of quadrivalent human papillomavirus vaccine in males—advisory committee on immunization practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60(50):1705–8.
Palefsky JM, Giuliano AR, Goldstone S, Moreira ED Jr., Aranda C, Jessen H, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med. 2011;365(17):1576–85.
Lin C, Slama J, Gonzalez P, Goodman MT, Xia N, Kreimer AR, et al. Cervical determinants of anal HPV infection and high-grade anal lesions in women: a collaborative pooled analysis. Lancet Infect Dis. 2019;19(8):880–91.
Faber MT, Frederiksen K, Palefsky J, Kjaer SK. Risk of anal cancer following benign anal disease and anal cancer precursor lesions: a Danish nationwide cohort study. Cancer Epidemiol Biomarkers Prev. 2020;29(1):185–92. https://doi.org/10.1158/1055-9965.EPI-19-0601.
Knowles G, Haigh R, McLean C, Phillips H. Late effects and quality of life after chemo-radiation for the treatment of anal cancer. Eur J Oncol Nurs. 2015;19(5):479–85.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Heer, M. Hackl, M. Ferlitsch, T. Waldhör and L. Yang declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Caption Electronic Supplementary Material
508_2020_1622_MOESM1_ESM.docx
Supplemental Table 1: Sex-specific age-standardised incidence rates of anal cancer from 1983 through 2016 in Austria; Supplemental Table 2. Sex-specific crude incidence rates of anal cancer from 1983–1987 through 2013–2016 in Austria
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heer, E., Hackl, M., Ferlitsch, M. et al. Trends in incidence of anal cancer in Austria, 1983–2016. Wien Klin Wochenschr 132, 438–443 (2020). https://doi.org/10.1007/s00508-020-01622-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-020-01622-z