Summary
Background and aims
Liver fatty acid-binding protein (L-FABP) is a small cytoplasmic protein. The aim of the current study was to investigate L-FABP levels and to determine their diagnostic value for non-alcoholic fatty liver disease (NAFLD).
Methods
We enrolled in this study 24 consecutive patients with NAFLD who were diagnosed with elevated transaminases and with steatosis by ultrasonograph. The control group consisted of 22 healthy control subjects matched for age and gender. Serum levels of L-FABP were determined by enzyme-linked immunosorbent assay.
Results
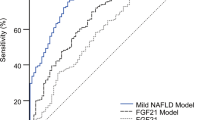
L-FABP levels in NAFLD patients were higher than in the control group (levels were 41,976 ± 18,998 and 17048 ± 5021 pg/mL, respectively). A strong correlation was found between serum L-FABP concentrations and aspartate aminotransferase, alanine aminotransferase, body mass index, glucose and γ-glutamyltransferase levels. A level of 284,000 pg/mL L-FABP had 73 % sensitivity and 100 % specificity. Positive and negative predictive values for L-FABP were 100 and 79%, respectively.
Conclusions
Serum L-FABP can be considered as a new diagnostic marker for detecting non-alcoholic fatty liver disease.
Zusammenfassung
Hintergrund und Ziele
Das Leber-Fettsäurebindungsprotein (L-FABP) ist ein kleines zytoplasmatisches Protein. Ziel der vorliegenden Studie war es, die L-FABP Konzentrationen zu bestimmen und ihren diagnostischen Wert bei der nicht-alkoholischen Fettlebererkrankung (NAFLD) zu erheben.
Methodik
Wir schlossen 24 konsekutive Patienten mit NAFLD, die durch erhöhte Transaminasen und mittels Ultraschall erhobener Steatose diagnostiziert worden war, in diese Studie ein. Die Kontrollgruppe bestand aus 22 gesunden Kontrollpersonen, die im Alter und Geschlecht der Gruppe mit NAFLD entsprachen.
Die Serumkonzentrationen des L-FABPs wurden mit ELISA bestimmt.
Ergebnisse
Die L-FABP Spiegel waren bei den Patienten mit NAFLD höher als in der Kontrollgruppe (41.976 ± 18.998 pg/mL im Vergleich zu 17048 ± 5021 pg/mL). Es wurde eine starke Korrelation zwischen den L-FABP Konzentrationen und AST, ALT, BMI, Glucose und gamma GT Werten gefunden. Eine Konzentration der L-FABP von 284.000 pg/mL hatte eine Sensitivität von 73 % und eine Spezifität von 100 %. Der positive Vorhersagewert der L-FABP lag bei 100 %, der negative bei 79 %.
Schlussfolgerungen
Die Serum L-FABP kann als neuer diagnostischer Marker zur Entdeckung einer nicht alkoholischen Fettlebererkrankung aufgefasst werden.

Similar content being viewed by others
References
Chitturi S, Farrell G, George J. Non-alcoholic steatohepatitis in the Asia-Pacific region: future shock? J Gastroenterol Hepatol. 2004;1:368–74.
Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37(4):917–23.
Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–21.
Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–9.
Angelico F, Del Ben M, Conti R, Francioso S, Feole K, Fiorello S, et al. Insulin resistance, the metabolic syndrome, and nonalcoholic fatty liver disease. J Clin Endocrinol Metab. 2005;90(3):1578–82.
Lee D, Wada K, Taniguchi Y, Al-Shareef H, Masuda T, Usami Y, Aikawa T, Okura M, Kamisaki Y, Kogo M. Expression of fatty acid binding protein 4 is involved in the cell growth of oral squamous cell carcinoma. Oncol Rep. 2014;31(3):1116–20.
Jeon WS, Park SE, Rhee EJ, Park CY, Oh KW, Park SW, Lee WY. Association of serum adipocyte-specific fatty acid binding protein with fatty liver index as a predictive indicator of nonalcoholic fatty liver disease. Endocrinol Metab (Seoul). 2013;28(4):283–7.
Kim YC, Cho YK, Lee WY, Kim HJ, Park JH, Park DI, Sohn CI, Jeon WK, Kim BI, Park SE, Rhee EJ, Park CY, Oh KW, Park SW, Kim SW, Ryu SH. Serum adipocyte-specific fatty acid-binding protein is associated with nonalcoholic fatty liver disease in apparently healthy subjects. J Nutr Biochem. 2011;22(3):289–92.
Masetti M, Bianchi G, Gianotti G, Giovagnoli M, Vizioli L, Zorzi V, Rossi V, Forti P, Zoli M. Adipocyte-fatty acid binding protein and non-alcoholic fatty liver disease in the elderly. Aging Clin Exp Res. 2014;26(3):241–7.
Ozbek M, Erdogan M, Dogan M, et al. Serum heart-type fatty acid binding protein (H-FABP) levels in acromegaly patients. J Endocrinol Invest. 2011;34:576–9.
Akbal E, Ozbek M, Gunes F, et al. Serum heart type fatty acid binding protein levels in metabolic syndrome. Endocrine. 2009;36:433–7.
Oktay B, Akbal E, Firat H, et al. Evaluation of the relationship between heart type fatty acid binding protein levels and the risk of cardiac damage in patients with obstructive sleep apnea syndrome. Sleep Breath. 2008;12:223–8.
Negishi K, Noiri E, Doi K, et al. Monitoring of urinary L-type fatty acid-binding protein predicts histological severity of acute kidney injury. Am J Pathol. 2009;174:1154–9.
Nielsen SE, Sugaya T, Hovind P, et al. Urinary liver-type fatty acidbinding protein predicts progression to nephropathy in type 1 diabetic patients. Diabetes Care. 2010;33:1320–4.
Sasaki H, Kamijo-Ikemori A, Sugaya T, et al. Urinary fatty acids and liver-type fatty acid binding protein in diabetic nephropathy. Nephron Clin Pract. 2009;112:148–56.
Guzmán C, Benet M, Pisonero-Vaquero S, Moya M, García-Mediavilla MV, Martínez-Chantar ML, González-Gallego J, Castell JV, Sánchez-Campos S, Jover R. The human liver fatty acid binding protein (FABP1) gene is activated by FOXA1 and PPARα; and repressed by C/EBPα: Implications in FABP1 down-regulation in nonalcoholic fatty liver disease. Biochim Biophys Acta. 2013;1831(4):803–18.
Furuhashi M, Hotamisligil GS. Fatty acid-binding proteins: role in metabolic diseases and potential as drug targets. Nat Rev Drug Discov. 2008;7:489–503.
Özenirler S, Degertekin CK, Erkan G, Elbeğ Ş, Tuncer C, Kandilc U, Akyol G. Serum liver fatty acid binding protein shows good correlation with liver histology in NASH. Hepatogastroenterology. 2013;60(125):1095–100.
Long D, Mu Y, Yang D. Molecular dynamics simulation of ligand dissociation from liver fatty acid binding protein. PLoS One. 2009;4:e6081.
Pelsers MM, Morovat A, Alexander GJ, et al. Liver fatty acid-binding protein as a sensitive serum marker of acute hepatocellular damage in liver transplant recipients. Clin Chem. 2002;48:2055–7.
Ishimitsu T, Ohta S, Saito M, et al. Urinary excretion of liver fatty acid-binding protein in health-check participants. Clin Exp Nephrol. 2005;9:34–9.
Akbal E, Köklü S, Koçak E, Cakal B, Güneş F, Başar O, Tuna Y, Senes M. Liver fatty acid-binding protein is a diagnostic marker to detect liver injury due to chronic hepatitis C infection. Arch Med Res. 2013;44(1):34–8. doi:10.1016/j.arcmed.2012.11.007.
Hamaguchi M, Kojima T, Itoh Y, Harano Y, Fujii K, Nakajima T, Kato T, Takeda N, Okuda J, Ida K, Kawahito Y, Yoshikawa T, Okanoue T. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol. 2007;102(12):2708–15.
Pelsers MM, Morovat A, Alexander GJ, et al. Liver fatty acid-binding protein as a sensitive serum marker of acute hepatocellular damage in liver transplant recipients. Clin Chem. 2002;48:2055–7.
Chen A, Tang Y, Davis V, Hsu FF, Kennedy SM, Song H, Turk J, Brunt EM, Newberry EP, Davidson NO. Liver fatty acid binding protein (L-FABP) modulates murine stellate cell activation and diet-induced nonalcoholic fatty liver disease. Hepatology. 2013;57(6):2202–12.
van den Broek MA, Bloemen JG, Dello SA, et al. Randomized controlled trial analyzing the effect of 15 or 30 min intermittent Pringle maneuver on hepatocellular damage during liver surgery. J Hepatol. 2011;55:337–45.
Van de Poll MC, Derikx JP, Buurman WA, et al. Liver manipulation causes hepatocyte injury and precedes systemic inflammation in patients undergoing liver resection. World J Surg. 2007;31:2033–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akbal, E., Koçak, E., Akyürek, Ö. et al. Liver fatty acid-binding protein as a diagnostic marker for non-alcoholic fatty liver disease. Wien Klin Wochenschr 128, 48–52 (2016). https://doi.org/10.1007/s00508-014-0680-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00508-014-0680-8