Abstract
Background
Over one thousand pediatric kidney transplant candidates are added to the waitlist annually, yet the prospective time spent waiting is unknown for many. Our study fills this gap by identifying variables that impact waitlist time and by creating an index to predict the likelihood of a pediatric candidate receiving a transplant within 1 year of listing. This index could be used to guide patient management by giving clinicians a potential timeline for each candidate’s listing based on a unique combination of risk factors.
Methods
A retrospective analysis of 3757 pediatric kidney transplant candidates from the 2014 to 2020 OPTN/UNOS database was performed. The data was randomly divided into a training set, comprising two-thirds of the data, and a testing set, comprising one-third of the data. From the training set, univariable and multivariable logistic regressions were used to identify significant predictive factors affecting wait times. A predictive index was created using variables significant in the multivariable analysis. The index’s ability to predict likelihood of transplantation within 1 year of listing was validated using ROC analysis on the training set. Validation of the index using ROC analysis was repeated on the testing set.
Results
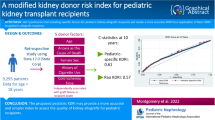
A total of 10 variables were found to be significant. The five most significant variables include the following: blood group, B (OR 0.65); dialysis status (OR 3.67); kidney disease etiology, SLE (OR 0.38); and OPTN region, 5 (OR 0.54) and 6 (OR 0.46). ROC analysis of the index on the training set yielded a c-statistic of 0.71. ROC analysis of the index on the testing set yielded a c-statistic of 0.68.
Conclusions
This index is a modest prognostic model to assess time to pediatric kidney transplantation. It is intended as a supplementary tool to guide patient management by providing clinicians with an individualized prospective timeline for each candidate. Early identification of candidates with potential for prolonged waiting times may help encourage more living donation including paired donation chains.
Graphical Abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Kidney allografts remain a scarce resource despite the increasing demand for kidneys over the last decade [1,2,3]. To create a more equitable system for organ allocation based on this shortage, the Organ Procurement and Transplantation Network (OPTN), operating under the United Network for Organ Sharing (UNOS), routinely updates their kidney allocation system (KAS) to increase accessibility to candidates who are traditionally less likely to receive an organ offer (e.g., highly sensitized patients, racial minorities) [4, 5]. While the OPTN has updated the KAS with moderate success in decreasing racial allocation disparities [4, 5], issues related to allograft availability remain for both adult and pediatric recipients leading to increased waitlist times [1]. For pediatric patients listed in 2016, 76.2% underwent transplant within 3 years; however, 14.2% were still waiting [1]. Additionally, 20% of the kidneys available for transplant were discarded per the 2020 OPTN/SRTR annual report, reaching an all-time high for kidney non-utilization and contributing to the scarce supply of kidney organs [2].
Currently, most pediatric kidney transplantation research focuses on post-transplant outcomes, donor availability, the effects of the 2014 and 2021 KAS updates, and racial disparities. Literature addressing specific factors impacting waitlist outcomes in adults shows that multiple comorbidities, minority status, prolonged time on dialysis, and frequent hospitalizations lead to higher mortality and delayed transplantation among waitlisted candidates [6,7,8,9,10,11,12]. Limited literature is available about pediatric candidates less than 18 years old. Our study, the first of its kind, seeks to better understand what factors contribute to pediatric kidney waitlist times and then use these factors to create a novel index which clinicians may use to better estimate the likelihood of deceased donor kidney transplantation within 1 year of listing.
Methods
Study population
We performed a retrospective, multi-center, longitudinal analysis of de-identified data from 3757 patients provided by the United Network for Organ Sharing (UNOS) database from 2014 to 2020. Exclusion criteria included patients who were 18 years of age or older, who had a previous transplant of any kind, who were on an additional waitlist for another organ, who had a concurrent transplant, who had a live donor transplant, and who were listed prior to the implementation of the 2014 KAS allocation policy change. Patients who were removed from the waitlist for reasons other than transplantation were censored as our only measured outcome was receipt of transplant within 1 year of listing.
Statistical analysis
Statistical analysis was performed using Stata 17.0 (Stata Corp). The data was randomly divided into a training set, comprising of two-thirds of the data, and a testing set comprising one-third of the data. A univariable and multivariable logistic regression analysis was performed on the training set to detect factors that were significant (p-value < 0.05) in predicting time spent on the waitlist. The primary outcome for this analysis was receipt of a transplant within 1 year of candidate listing. Only variables that were significant (p-value < 0.05) in the univariable analysis were included in the multivariable analysis.
Missing data
Variables with incomplete observations underwent multiple imputation via predictive mean matching with fifth nearest neighbor discriminant analysis. Five iterations of imputation were performed for each variable with missing data. Variables that underwent multiple imputation included the following: BMI-for-age and height-for-age. Percent completion of the data before and after imputation is shown in Table SM1 in Supplementary Materials.
Variables
The variables considered for this study are shown in Table 1. Variables were recorded at the time of listing and taken directly from the UNOS/OPTN database. Continuous variables were categorized into clinically relevant groupings with reference ranges determined using clinical judgement. Reference variables can be seen in Table 2. BMI-for-age and height-for-age were used in lieu of BMI. Due to the different sizes of growing pediatric patients, BMI that is not adjusted for age has poor predictive value in the pediatric population [13]. Both of the above anthropometric variables are validated measurements for ages 0–19 years, per the World Health Organization (WHO); the measurements are standardized based on z-scores set by the WHO 2007 child growth standards [14]. These variables were created using the “zanthro” package provided by Stata, which utilizes the WHO 2007 growth standards [15].
Due to the heterogeneity of our population's primary diagnoses and these diagnoses being coded using non-standardized language in the UNOS database, a new variable was created to provide an accurate reflection of the prevalence of the diseases in our cohort. Each data point was manually selected and placed into appropriate groupings of matching or similar pathologies so that each etiology was appropriately coded for. Each diagnosis was then turned into its own dummy variable for analysis. The specific diagnoses included in each etiology grouping can be seen in Table SM2 in the Supplementary Materials.
The following characteristics were included in the univariable analysis: age (years); blood group, A, B, O, and AB; BMI-for-age; height-for-age; dialysis status; race/ethnicity, white, African American, Hispanic, Asian-American, Native American, Native Pacific Islander, and multiracial; cPRA value; weight (kilograms); kidney disease etiology, acquired kidney defect, amyloidosis, BK virus nephropathy, cancer-associated nephropathy, diabetes, drug-induced nephropathy, heart failure/hypertension, HIV-associated nephropathy, hypoplasia/aplasia/dysplasia, immune complex-associated nephropathy, ischemic/septic nephropathy, MELAS, metabolic pathway disorders, nephrotic/nephritic syndromes, nephrocalcinosis, neurogenic bladder, prematurity-associated nephropathy, SLE, tubular dysfunction, unspecified autoimmune disease, unspecified familial kidney disease, unspecified glomerulonephritis, unspecified interstitial nephritis, vasculitis, and unknown etiology; insurance type, private and public; and UNOS region, 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, and 11 (see Supplementary Materials for OPTN region map [16]).
Risk index
Only variables that were significant in the multivariable analysis were used to create the risk index. The development of the index was modeled after the liver transplant length of stay index by Rana et al. [17]. The presence or absence of each significant variable, coded as either one or zero, respectively, was multiplied by the logarithmic function of their corresponding odds ratio. The exponential function of the sum of these values yielded an index score. The index was validated for its ability to predict transplantation within 1 year of listing using ROC analysis on both the training and testing sets.
Results
Demographics
Total sample size following exclusionary criteria was 3757 patients. Our study cohort was composed primarily of adolescent patients between the ages of 14 and 18 years old (39%) with a progressive decrease in frequency in lower age groups. Only 6% of our study population was 1 year old or younger. Group O blood type was the most common blood group at 54%, followed by group A at 31%. Group B and group AB comprised 13% and 3% of the study cohort, respectively. Growth parameter BMI-for-age had a normal distribution with most patients (59%) falling between z-scores − 2.0 and 1.0. Height-for-age had a normal distribution with a slight positive skew. The majority of patients (75%) fell between z-scores − 2.0 and 3.0. Thirty-six percent of our study population weighed 50 kg or more, while 21% of patients weighed between 10 and 20 kg. Only 4% weighed less than 10 kg. Over half of our patients were on dialysis (59%). Ninety-one percent of our cohort had a cPRA value of zero. Regarding race, 39% of our study was White, 31% Hispanic, 21% African American, and 5% Asian. The remaining 4% were Native American, Native Pacific Islander, or multiracial. The four most common kidney disease etiologies were kidney hypoplasia, dysplasia, and aplasia (50%); nephrotic and nephritic syndromes (20%); ischemic or septic nephropathy (5%); and vasculitis (5%). Unknown etiologies comprised 7% of the cohort. Almost two-thirds of our study population had some form of public insurance (63%), approximately one-third (31%) had private insurance, and 6% had other payment sources, such as charity or self-pay. Finally, 21% of our study population was located in region 5, while approximately 70% of our population was evenly distributed among regions 2, 3, 4, 7, 8, 9, 10, and 11. Only 8% of our study population was located in regions 1 or 6.
Univariable and multivariable analysis
Table 2 includes all factors assessed in the univariable analysis. Only variables significant in the univariable analysis were included in the multivariable analysis, shown in Table 3. Variables that were significant and examined in the multivariable analysis include the following: age (years), < 1, > 10, and ≤ 14; blood group, B and AB; height-for-age, z-score > 3; dialysis status; race/ethnicity, Asian; weight (kilograms), ≥ 0 and < 10, and ≥ 10 and < 20; kidney disease etiology, hypoplasia/aplasia/dysplasia, nephrotic/nephritic syndromes, SLE, and vasculitis; insurance type, public; and UNOS region, 2, 3, 4, 5, 6, 8, 9, and 10.
Variables that were significant (p-value < 0.05) in the multivariable analysis include the following: blood group, B and AB; dialysis status; weight (kilograms), ≥ 0 and < 10, and ≥ 10 and < 20; kidney disease etiology, SLE; and OPTN region, 5, 6, 9, and 10. The most significant predictive factors for likelihood to transplantation within 1 year of listing include the following: blood group, B (OR 0.65, p-value = 0.00); dialysis status (OR 3.67, p-value = 0.00); kidney disease etiology, SLE (OR 0.38, p-value = 0.00); and OPTN region, 5 (OR 0.54, p-value = 0.00) and 6 (OR 0.46, p-value = 0.00).
Risk index
Significant variables (p-value < 0.05) in the multivariable analysis were used to create the risk index, which can be calculated using the following equation:
The risk index was stratified into quartiles and then graphed against their median time on the waitlist (Fig. 1). The index quartiles were also used to create a Kaplan–Meier failure estimate curve displaying event likelihood (transplantation within 1 year of listing) over time (Fig. 2). Patients with a lower index score had higher median wait times with those in the bottom tenth percentile having a median wait time of 532 days. Patients with a higher index score had lower median wait times with the top tenth percentile having a median wait time of 142 days. ROC analysis of the index against the training set yielded a c-statistic of 0.71 (Fig. 3a). Examined against the testing set, ROC analysis of the index revealed a c-statistic of 0.68 (Fig. 3b).
Risk index scores stratified into quartiles and then graphed against their median wait time. As index scores increase, median wait time steadily decreases. Median wait time for those in quartile 4 is less than half of the wait time for patients in quartile 1. The values for each quartile: Quartile 1: ≤ 1.00; Quartile 2: 1.00-1.64; Quartile 3: 1.64-3.67; and Quartile 4: >3.67.
Kaplan-Meier failure estimates for each index quartile displaying likelihood of transplantation within one year of listing. A higher index score is associated with increased event likelihood. A reference line at 365 days is present, representing the one year from listing threshold we designated as our "failure" event. Following the one year mark, index scores in the first quartile start to lag much further behind the other three quartiles with regards to event likelihood. At around 1320 days (approximately 3.5 years) quartile 3 overtakes quartile 4, now having an event likelihood of 93%
Discussion
The novel pediatric kidney transplant waitlist index developed by this study includes 10 variables that were all determined to be significant (p-value < 0.05) in the multivariable analysis. They include the following: blood group, B and AB; dialysis status; weight (kilograms), ≥ 0 and < 10, and ≥ 10 and < 20; kidney disease etiology, SLE; and OPTN region, 5, 6, 9, and 10. ROC analysis of the index against the training and testing sets revealed a c-statistic of 0.71 and 0.68, respectively, indicating that this index is a modest prognosticator of the likelihood of pediatric kidney transplantation within 1 year of listing. A resulting c-statistic of 0.5 indicates random association while a c-statistic of 1.0 indicates a perfect association.
Our study is the first of its kind to investigate multiple factors affecting waitlist times specific to pediatric kidney transplantations. Previous literature analyzing factors impacting waitlist times has been focused on the adult population and identified different factors for adults compared to our findings for pediatrics. The adult studies identified factors such as PRA status, blood type, and age to be significant predictors affecting waitlist time for deceased-donor kidney transplant, and increased comorbidity burden was associated with waitlist mortality [6, 7]. Additionally, hospitalization within the first year of waitlisting was associated with a lower likelihood of receiving a kidney transplant and worse 5-year survival, which progressively decreased with increased hospital length of stay [8]. In adults, factors of age, diabetes, cardiovascular disease, and chronic obstructive pulmonary disease also contributed to increased mortality [8]. Racial disparities were also identified and have been identified in pediatric patients as well [11].
Black and Hispanic patients are both found to have decreased likelihood of receiving a transplant compared to non-Hispanic White patients, with disparities persisting into young adulthood [11, 12, 18]. However, reports by Melanson et al. indicate amelioration of these disparities through the 2014 KAS update [5]. Despite the longstanding history of racial disparities among pediatric and adult kidney transplant patients, our study did not find race to be a significant factor for predicting time to transplantation. One possibility for this finding is that minority patients become transplant candidates at a more advanced stage of disease due to racial bias upstream in their care, preventing them from being preemptively waitlisted. Another possibility is that the KAS update objective to reduce racial disparities in transplantation has been successful. Per the annual OPTN/UNOS reports, discrepancies in rate of transplantation between white and minority patients have continued to decline [2, 19].
Our pediatric waitlist index includes several variables that have been independently reported as predictive risk factors for decreased rates of transplantation. For example, blood group B has been widely reported as being associated with decreased likelihood of organ transplant, with much of the literature suggesting the implementation of ABO incompatible (ABOi) transplants to compensate for this disproportionate gap in transplants between blood groups [1, 20, 21]. Additionally, geographic variation in access to transplantation has been documented as an independent risk factor for decreased rates of transplantation. As shown by Mathur et al. in 2010, areas with increasing kidney failure incidence have diminished access to the transplant waitlist when compared to patients in low kidney failure incidence areas even after accounting for local donation rates [22]. Areas with moderate to high kidney failure incidence corresponded most with UNOS regions 2, 3, 4, 5, 9, 10, and 11 [22]. Further, research by Reese et al. in 2014 reported similar findings of geographic variation in wait times for pediatric patients with wait times most increased in areas corresponding to regions 2, 5, and 9 [23]. These findings are similar to our study which found regions 5, 6, and 9 to be associated with a decreased likelihood of transplantation. Overall inequities in wait times among OPTN regions have been attributed to inadequate supply of locally procured organs in the face of increasing demand in regions with a high proportion of highly sensitized minority patients [24]. Additionally, the differing criteria for organ acceptance versus rejection for each individual transplant center have been suggested as a contributing factor toward regional variation in wait times [25].
Such center-specific practices must be considered as there are no specific criteria set by the KAS that patients need to meet to be waitlisted [26]. Parameters such as GFR and dialysis status exist in the KAS to aid in calculation of wait times for candidates (i.e., pediatric patients’ time on dialysis prior to listing will count toward their wait time; patients with longer wait times are considered higher priority). Additionally, listing protocol for each center may be further varied based on the patient’s disease. For example, children with congenital malformations may be listed at earlier stages in their disease if it is anticipated they will require a transplant compared to older children with acquired kidney failure, leading to a “prolonged” wait time. King et al. found that variations in wait time among patients of similar characteristics (e.g., disease status, sensitization, comorbidities, age) were smaller compared to the overall variation between centers within specific regions [25]. These findings suggest that center-specific listing and transplant protocols, rather than patient characteristics themselves, have significantly more influence on wait time than previously thought.
Age was not found to be a significant predictor of likelihood of transplantation. This does not align with the previous literature as, historically, patients have a progressive increase in likelihood for transplantation with decreasing age, likely due to receiving higher pediatric priority points and decreased likelihood of sensitization compared to adolescents [27, 28]. One consideration is that younger, smaller candidates pose more difficulties in size-matching donor kidneys, as well as increased risk for thrombosis due to small vessel size [29, 30]. Our findings that candidates weighing less than 20 kg have as much as a 57% decreased likelihood of transplantation within a year of listing would support this notion. However, advances in infant kidney transplantation have allowed for decreased rates of graft failure with improved long-term outcomes, thereby removing the need to prolong wait times while the patient grows to an adequate height and weight [29,30,31]. Such advances are likely to contribute toward younger age groups not being statistically significant in our study.
Heavier weight groups were not found to be statistically significant in either the univariable or multivariable analysis. Anthropometric variables BMI-for-age and height-for-age were also not found to be significant predictors of likelihood to transplantation. These variables are likely to be impacted by disease severity as kidney failure has a well-known effect on bone mineralization and vertical growth [32,33,34]. Given the heterogeneity of kidney failure etiology and age of disease presentation, these growth parameters may be a poor predictor of wait time, as shown in our study. Further analysis of our data does not show a correlation between any growth parameters and age.
Interestingly, cPRA was not found to be a significant predictor of likelihood to transplantation in either direction. This does not align with previous findings showing significant increases in the rate of transplantation for highly sensitized patients with elevated cPRA values, an intended result by the 2014 KAS update [35,36,37,38,39]. Previous literature has also shown a resultant significant decline in rate of transplantation for those with lower cPRA values, primarily those with a value of zero percent [38, 39]. Our findings are likely due to priority points being assigned to patients with increasing cPRA values, counterbalanced by the difficulty in finding a donor that has minimal to no reactive antigens [26].
Systemic lupus erythematous was the only kidney disease etiology found to be a significant predictor with patients in our study being 62% less likely to receive a transplant within one year of listing. It has been thought that allowing for disease remission and symptom quiescence via an extended waiting period would prevent post-transplantation complications and allograft loss [41,42,43]. This practice is a likely contributor to our finding however, evidence that this longer wait time provides any benefit has been mixed, with some studies showing an increased risk of graft failure [42,43,44].
Finally, dialysis status was a significant predictive variable for likelihood to transplantation. Patients who are on dialysis are over three times as likely to receive a transplant within a year of listing compared to their non-dialysis peers. This finding is similar to that of Shelton et al. and is also in line with the KAS protocol, which counts time on dialysis prior to listing towards wait time, which in turn increases listing priority [26, 40].
Our index not only includes significant predictive factors impacting the likelihood of transplantation but may also provide important insights about potential prolonged waitlist times for a given candidate. For example, our index was inversely related to wait time; patients with an index score in the bottom ten percent have a median wait time over twice as long as those in the top ten percent. This important finding is likely to have clinical implications. Our index may provide early identification of candidates at risk for prolonged waitlist time, for whom interventions might be made to lower morbidity while awaiting a donor kidney and to find potential living donors to obviate waitlist time.
Such implications have yet to be applied to countries outside of the United States as this index is based on US population-specific factors. Further research is needed utilizing foreign transplant databases as variables that will be significant may differ due to diverse patient characteristics that are dissimilar to those seen in the US. Patient characteristics such as comorbidities, age of disease presentation, and age of listing may differ due to societal influences, including healthcare accessibility, racial biases in healthcare, and environmental factors contributing to the level of obesity, diabetes, and heart disease in the general population.
Potential limitations
The UNOS database is subject to inaccurate data input as exemplified by the non-standardized and mistakenly coded diagnoses that necesitated recoding and reorganization of the data. However, the strength of this database lies in its longitudinal nature and massive sample size. Even after excluding data prior to the 2014 KAS update, we were able to maintain a large sample size, thereby increasing the power of our study. An additional limitation includes the very slight model performance mismatch as ROC analysis yielded differing c-statistics between the training and testing sets, although this result is to be expected. C-statistic discordance can be due to under-representative data in either set; however, this was mitigated by sampling randomization when splitting the dataset into the two cohorts.
Conclusions
This retrospective, multi-center, longitudinal analysis of 3757 pediatric kidney transplant candidates was performed to identify predictive factors impacting time spent on the deceased donor waitlist. A pediatric waitlist index was created after identifying 10 significant candidate factors that influence likelihood of transplantation within 1 year of being placed on the waitlist. Our index had a c-statistic of 0.71 and 0.68 when derived from the training and testing sets, respectively. The most important factors in this index are blood group, dialysis status, kidney disease etiology, and UNOS region. This index is intended to be used as a supplementary tool to help guide clinical management of pediatric transplant candidates. We hope that the modest prognostication provided by our model may empower clinicians and families to reduce waitlist morbidity, find more living donors, and utilize more paired donation chains to optimize long-term pediatric patient outcomes. Further research is needed to optimize this index and further increase its predictive power, as well as to generate an index that is applicable to populations outside of the United States.
Data availability
Data utilized in this study were from the United Network for Organ Sharing public database. Statistical analysis utilized Stata 17.0 (Stata Corp).
Change history
04 June 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00467-024-06401-w
Abbreviations
- cPRA:
-
Calculated panel reactive antibody
- GFR:
-
Glomerular filtration rate
- HLA:
-
Human leukocyte antigen
- KAS:
-
Kidney allocation system
- OPTN:
-
Organ Procurement and Transplantation Network
- UNOS:
-
United Network for Organ Sharing
References
Hart A, Lentine KL, Smith JM et al (2021) OPTN/SRTR 2019 annual data report: kidney. Am J Transplant 21:21–137. https://doi.org/10.1111/ajt.16502
Lentine KL, Smith JM, Hart A et al (2022) OPTN/SRTR 2020 annual data report: kidney. Am J Transplant 22:21–136. https://doi.org/10.1111/ajt.16982
Bastani B (2020) The present and future of transplant organ shortage: some potential remedies. J Nephrol 33:277–288
Chopra B, Sureshkumar KK (2015) Changing organ allocation policy for kidney transplantation in the United States. World J Transplant 5:38. https://doi.org/10.5500/wjt.v5.i2.38
Melanson TA, Hockenberry JM, Plantinga L et al (2017) New kidney allocation system associated with increased rates of transplants among Black and Hispanic patients. Health Aff 36:1078–1085. https://doi.org/10.1377/hlthaff.2016.1625
Ryu JH, Koo TY, Ha JY et al (2018) Factors associated with waiting time to deceased donor kidney transplantation in transplant candidates. Transplant Proc 50:1041–1044. https://doi.org/10.1016/J.TRANSPROCEED.2018.02.038
Pérez Fernández M, Martínez Miguel P, Ying H et al (2019) Comorbidity, frailty, and waitlist mortality among kidney transplant candidates of all ages. Am J Nephrol 49:103–110. https://doi.org/10.1159/000496061
Lynch RJ, Zhang R, Patzer RE et al (2017) First-year waitlist hospitalization and subsequent waitlist and transplant outcome. Am J Transplant 17:1031–1041. https://doi.org/10.1111/ajt.14061
Gill JS, Tonelli M, Johnson N et al (2005) The impact of waiting time and comorbid conditions on the survival benefit of kidney transplantation. Kidney Int 68:2345–2351. https://doi.org/10.1111/J.1523-1755.2005.00696.X
Meier-Kriesche HU, Kaplan B (2002) Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: a paired donor kidney analysis. Transplantation 74:1377–1381. https://doi.org/10.1097/00007890-200211270-00005
Patzer RE, Amaral S, Klein M et al (2012) Racial disparities in pediatric access to kidney transplantation: does socioeconomic status play a role? Am J Transplant 12:369. https://doi.org/10.1111/J.1600-6143.2011.03888.X
Laster M, Soohoo M, Hall C et al (2017) Racial-ethnic disparities in mortality and kidney transplant outcomes among pediatric dialysis patients. Pediatr Nephrol 32:685. https://doi.org/10.1007/S00467-016-3530-2
Vanderwall C, Randall Clark R, Eickhoff J, Carrel AL (2017) BMI is a poor predictor of adiposity in young overweight and obese children. BMC Pediatr 17:135. https://doi.org/10.1186/S12887-017-0891-Z
Khadilkar V, Khadilkar A (2011) Growth charts: a diagnostic tool. Indian J Endocrinol Metab 15:S166. https://doi.org/10.4103/2230-8210.84854
Vidmar SI, Cole TJ, Pan H (2013) Standardizing anthropometric measures in children and adolescents with functions for egen: update. Stata J 13:366–378
Regions - OPTN. In: Organ Procurement and Transplantation Network. https://optn.transplant.hrsa.gov/about/regions/. Accessed 23 Aug 2022
Rana A, Witte ED, Halazun KJ et al (2017) Liver transplant length of stay (LOS) index: a novel predictive score for hospital length of stay following liver transplantation. Clin Transplant 31. https://doi.org/10.1111/ctr.13141
Amaral S, Patzer R (2013) Disparities, race/ethnicity and access to pediatric kidney transplantation. Curr Opin Nephrol Hypertens 22:336–343. https://doi.org/10.1097/MNH.0B013E32835FE55B
Hart A, Smith JM, Skeans MA et al (2020) OPTN/SRTR 2018 annual data report: kidney. Am J Transplant 20:20–130. https://doi.org/10.1111/ajt.15672
Manook M, Mumford L, Barnett ANR et al (2019) For the many: permitting deceased donor kidney transplantation across low-titre blood group antibodies can reduce wait times for blood group B recipients, and improve the overall number of 000MM transplants - a multicentre observational cohort study. Transplant Int 32:431–442. https://doi.org/10.1111/tri.13389
Redfield RR, Parsons RF, Rodriguez E et al (2012) Underutilization of A2 ABO incompatible kidney transplantation. Clin Transplant 26:489–494. https://doi.org/10.1111/j.1399-0012.2011.01543.x
Mathur AK, Ashby VB, Sands RL, Wolfe RA (2010) Geographic variation in end-stage renal disease incidence and access to deceased donor kidney transplantation: special feature. Am J Transplant 10:1069–1080. https://doi.org/10.1111/j.1600-6143.2010.03043.x
Reese PP, Hwang H, Potluri V et al (2014) Geographic determinants of access to pediatric deceased donor kidney transplantation. J Am Soc Nephrol 25:827–835. https://doi.org/10.1681/ASN.2013070684
Davis AE, Mehrotra S, McElroy LM et al (2014) The extent and predictors of waiting time geographic disparity in kidney transplantation in the United States. Transplantation 97:1049–1057. https://doi.org/10.1097/01.TP.0000438623.89310.DC
King KL, Ali Husain S, Schold JD et al (2020) Major variation across local transplant centers in probability of kidney transplant for wait-listed patients. J Am Soc Nephrol 31:2900–2911. https://doi.org/10.1681/ASN.2020030335
U.S. Department of Health and Human Services, OPTN Organ Procurement and Transplantation Network (2014) The new kidney allocation system (KAS) frequently asked questions. https://optn.transplant.hrsa.gov/professionals/by-topic/guidance/the-new-kidney-allocation-system-kas-frequently-asked-questions/. Accessed 23 Aug 2022
Bobanga ID, Vogt BA, Woodside KJ et al (2015) Outcome differences between young children and adolescents undergoing kidney transplantation. J Pediatr Surg 50:996–999
Smith JM, Ho PL, McDonald RA, North American Pediatric Renal Transplant Cooperative Study (2002) Renal transplant outcomes in adolescents: a report of the North American Pediatric Renal Transplant Cooperative Study. Pediatr Transplant 6:493–499
Jalanko H, Mattila I, Holmberg C (2015) Renal transplantation in infants. Pediatr Nephrol 31:725–735. https://doi.org/10.1007/S00467-015-3144-0
Salvatierra O, Millan M, Concepcion W (2006) Pediatric renal transplantation with considerations for successful outcomes. Semin Pediatr Surg 15:208–217. https://doi.org/10.1053/J.SEMPEDSURG.2006.03.007
Chavers B, Najarian JS, Humar A (2007) Kidney transplantation in infants and small children. Pediatr Transplant 11:702–708. https://doi.org/10.1111/J.1399-3046.2007.00768.X
Bacchetta J, Harambat J, Cochat P et al (2012) The consequences of chronic kidney disease on bone metabolism and growth in children. Nephrol Dial Transplant 27:3063–3071. https://doi.org/10.1093/ndt/gfs299
Neu AM (2006) Special issues in pediatric kidney transplantation. Adv Chronic Kidney Dis 13:62–69. https://doi.org/10.1053/J.ACKD.2005.10.001
Bonthuis M, Bakkaloglu SA, Vidal E et al (2023) Associations of longitudinal height and weight with clinical outcomes in pediatric kidney replacement therapy: results from the ESPN/ERA Registry. Pediatr Nephrol 38:3435–3443. https://doi.org/10.1007/S00467-023-05973-3
Jackson KR, Zhou S, Ruck J et al (2019) Pediatric deceased donor kidney transplant outcomes under the kidney allocation system. Am J Transplant 19:3079. https://doi.org/10.1111/AJT.15419
Stewart DE, Wilk AR, Toll AE et al (2018) Measuring and monitoring equity in access to deceased donor kidney transplantation. Am J Transplant 18:1924–1935. https://doi.org/10.1111/ajt.14922
Plumb L, Marks SD (2023) Transplant access for children: there is more to be done. Pediatr Nephrol 38:941–944. https://doi.org/10.1007/S00467-022-05787-9/METRICS
Engen RM, Smith JM, Bartosh SM (2022) The kidney allocation system and pediatric transplantation at 5 years. Pediatr Transplant 26:e14369. https://doi.org/10.1111/PETR.14369
Stewart DE, Kucheryavaya AY, Klassen DK et al (2016) Changes in deceased donor kidney transplantation one year after KAS implementation. Am J Transplant 16:1834–1847. https://doi.org/10.1111/ajt.13770
Shelton BA, Sawinski D, Ray C et al (2018) Decreasing deceased donor transplant rates among children (≤6 years) under the new kidney allocation system. Am J Transplant 18:1690–1698. https://doi.org/10.1111/AJT.14663
Oni L, Wright RD, Marks S et al (2021) Kidney outcomes for children with lupus nephritis. Pediatric Nephrology 36:1377–1385. https://doi.org/10.1007/S00467-020-04686-1
Mai K, Singer P, Fahmy AE et al (2022) Kidney transplant outcomes in children and adolescents with systemic lupus erythematosus. Pediatr Transplant 26:e14178. https://doi.org/10.1111/PETR.14178
Wong T, Goral S (2019) Lupus Nephritis and Kidney Transplantation: Where Are We Today? Adv Chronic Kidney Dis 26:313–322. https://doi.org/10.1053/J.ACKD.2019.08.007
Plantinga LC, Patzer RE, Drenkard C et al (2015) Association of Time to Kidney Transplantation With Graft Failure Among US Patients With End-Stage Renal Disease Due to Lupus Nephritis. Arthritis Care Res (Hoboken) 67:571–581. https://doi.org/10.1002/ACR.22482
Acknowledgements
Thank you to Nicholas Peoples (Baylor College of Medicine) and Connor Rollings (The University of Texas Health Science Center at Houston) for your support, both personal and professional.
Author information
Authors and Affiliations
Contributions
Study concept and design: Rana. Acquisition of data: Rana. Analysis and interpretation of data: Alvarez. Drafting of manuscript: Alvarez. Critical revision: Alvarez, Montgomery, Galvan, Brewer, Rana.
Corresponding author
Ethics declarations
Declarations
The authors have nothing to disclose. Due to using de-identified patient information, IRB approval was not needed and therefore waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Within this study, the authors constructed a pediatric waitlist risk index and stratified this index into quartiles. However, in the original manuscript, they did not include the range of values that each quartile spans. This has been added to the caption of fig. 1.
Supplementary information
Below is the link to the electronic supplementary material.
Graphical abstract
(PPTX 297 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alvarez, A., Montgomery, A., Galván, N.T.N. et al. Predicting wait time for pediatric kidney transplant: a novel index. Pediatr Nephrol 39, 2483–2493 (2024). https://doi.org/10.1007/s00467-023-06232-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06232-1