Abstract
Background
The aetiology of idiopathic nephrotic syndrome (INS) remains partially unknown. Viral infections have been associated with INS onset. Since we observed fewer first onset INS cases during the Covid-19 pandemic, we hypothesised that lower INS incidence was the result of lockdown measures. Therefore, the aim of this study was to evaluate the incidence of childhood INS before and during the COVID-19 pandemic in two independent European INS cohorts.
Methods
Children with new INS in the Netherlands (2018–2021) and Paris area (2018–2021) were included. We estimated incidences using census data for each region. Incidences were compared using two proportion Z-tests.
Results
A total of 128 and 324 cases of first onset INS were reported in the Netherlands and Paris area, respectively, corresponding to an annual incidence of 1.21 and 2.58 per 100,000 children/year. Boys and young children (< 7 years) were more frequently affected. Incidence before and during the pandemic did not differ. When schools were closed, incidence was lower in both regions: 0.53 vs. 1.31 (p = 0.017) in the Netherlands and 0.94 vs. 2.63 (p = 0.049) in the Paris area. During peaks of hospital admissions for Covid-19, no cases were reported in the Netherlands or Paris area.
Conclusions
Incidence of INS before and during the Covid-19 pandemic was not different, but when schools were closed during lockdown, incidence was significantly lower. Interestingly, incidences of other respiratory viral infections were also reduced as was air pollution. Together, these results argue for a link between INS onset and viral infections and/or environmental factors.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic nephrotic syndrome (INS) is the most common glomerulopathy in paediatric nephrology, but is a rare disease in the general paediatric population. Its incidence is estimated to be between 1.2 and 16.9 per 100,000 children per year [1,2,3], varying widely between global regions and ethnicities [4]. In the Netherlands, between 2007 and 2009, the incidence of INS was estimated to be 1.52 per 100,000 children per year, which corresponds with ± 60 cases annually [5]. In the Paris area, a higher incidence of 3.35 per 100,000 children per year (± 75 cases annually) was found between December 2007 and May 2010 [6].
Patients with new onset INS present with profound oedema, heavy proteinuria (urinary protein-to-creatinine ratio (uPCR) > 200 mg /mmol), and hypoalbuminaemia (serum albumin < 25 g/L) [7]. The exact pathogenesis is still largely unknown, but different theories have been proposed. First, the immune system seems to play an important role in the aetiology of INS, which involves dysfunction or dysregulation of T and B cells. The T cell hypothesis was first proposed by Shalboub in 1974 [8]. Later, involvement of B cells became apparent following sustained remission of the disease in patients receiving rituximab [9] and the recent identification of autoantibodies (UCHL1, anti Nephrin) [10, 11]. Second, the presence of a circulating permeability factor plays a role, particularly in focal segmental glomerulosclerosis [12]. To date, this factor has yet to be identified. Third, in line with the T cell hypothesis, viral pathogens or allergens may trigger the onset of INS as a two-hit mechanism by inducing CD80 in the podocytes, which cannot be effectively cleared due to a dysfunctional T cell response [13, 14]. Direct evidence has never been shown, however, epidemiological data support the association between viral triggers (Epstein-Barr virus (EBV) and enterovirus) and INS onset [14, 15].
When the world was hit by the rapidly emerging and newly discovered coronavirus (SARS-CoV-2) causing a global pandemic [16], governments across the world implemented lockdown measures to contain the spread of the virus. Lockdown measures also impacted children and adolescents, but varied strongly in degree, timing, and duration between countries. Measures included the closing of schools, sports events, and non-essential shops, as well as group size restrictions, the obligation to wear a facemask, and travel restrictions (both locally and internationally).
During these periods of lockdown, study teams of the LEARNS (the Netherlands) and NEPHROVIR-3 (Paris area, France) trial noticed a decrease in the number of first onset INS, hypothesising that this may be due to less exposure to viral pathogens as a – desired – result of social distancing. This phenomenon has previously been suggested for relapse rate [17,18,19]. Therefore, the aim of this study is to compare the incidence of INS before (before March, 2020) and during (from March, 2020 to December, 2021) the Covid-19 pandemic in the Netherlands and the Paris area. Additionally, the impact of different lockdown measures on incidence of INS was studied. To do so, we used incidence data from the LEARNS study and NEPHROVIR-3 study.
Methods
Study design
We conducted two separate, retrospective, cross-sectional, observational studies to estimate the incidence of INS in the Netherlands (January 2018 – December 2021) and the Paris area (January 2017 – December 2021). All new onset INS cases were prospectively registered as part of the ongoing clinical trials. In the Netherlands, an online survey was sent to all hospitals with a paediatric ward by email in order not to miss cases. After two and four weeks, a reminder was sent. An overview of all contacted hospitals can be found in the Online Resource 1. The survey was available online in Google Forms and consisted of 9 items divided over two parts: respondent and case details (see Online Resource 2). All hospitals participating in the NEPHROVIR-3 study were required to report any INS case during the recruitment phase, but since recruitment ended in February, 2020, all sites were contacted to report cases until December, 2021.
Study population
All children between 1 and 16 years of age who presented with a new onset INS in the Netherlands or Paris area were screened for eligibility for inclusion in either the LEARNS or the NEPHROVIR-3 study, respectively. INS was defined as the presence of oedema, proteinuria (uPCR > 200 mg/mmol), and hypoalbuminaemia (serum albumin < 25 g/L). Children with non-idiopathic nephrotic syndrome (secondary, genetic, or congenital) or children not living in either the Netherlands or Paris area were excluded. The population at risk consists of all children aged 1–16 years living in the Netherlands or Paris area.
Data collection
Date of first presentation, sex, and age were recorded on trial subject screening and enrolment logs. All data were screened for duplicates based on the case details. Census data (per January 1st) were extracted from the official statistic organs of the Netherlands (CBS: Centraal Bureau voor de Statistiek) and France (INSEE: Institut National de la Statistique et des Études Économiques).
To identify which and when lockdown measures were in effect, governmental and (national) news websites were used. Since testing policies changed over time in both countries, Covid-19-related hospitalisation, rather than confirmed cases of Covid-19, were used to illustrate the Covid-19 burden. Hospitalisation data were freely available from the website of the National Institute for Public Health and the Environment (Dutch: Rijksinstituut voor Volksgezondheid en Milieu (RIVM)) and Public Health France (French: Santé Publique France).
Outcome measures
The primary outcome was the difference in incidence of INS between before (before March 2020) and during (from March 2020) the Covid-19 pandemic in the Netherlands and Paris area. Incidence was expressed as the number of new cases per 100,000 children (≤ 16 years) at risk per year. Secondary outcomes included the effect of different lockdown measures on incidence in the two regions separately.
Statistical analysis
Descriptive continuous patient data are presented as the mean (standard deviation (SD)) or median (interquartile range (IQR)), depending on distribution. Discrete data are presented as frequencies and proportions (%).
To correct for missing cases, the true estimate was calculated. This estimate was based on the reported cases per month, adjusted for the total response rate for each survey. The response rate is the proportion of hospitals that completed the survey, independent of whether a case was reported. Assuming that missing reports were random and occurred independently from each other, the following equation was used:
To calculate the confidence intervals for the true number of cases, a Monte Carlo simulation was performed (n = 1000 simulations), where reported cases followed a Poisson distribution and response rate a binomial distribution.
The incidence of INS in both regions was calculated by dividing the true number of cases by the number of children between 1 and 16 years of age living in the Netherlands or Paris area (per January 1st of 2021) corrected for the total observation period:
Confidence intervals were obtained from the Monte Carlo simulation for the true number of cases estimate. Incidences (between Covid-period, sex, age group, lockdowns, and measures) were compared using a two-proportion Z-test. A p-value of < 0.05 was considered to be significantly different. All statistical tests were performed using R studio version 3.6.1 [20].
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Amsterdam University Medical Centers, location University of Amsterdam on March 8th, 2018 (2017_310). All subjects and/or their parents (if applicable) signed for informed consent. The LEARNS study is registered (www.trialregister.nl; NL6826). Further, the Ethics Committee concluded that the additional survey did not fall under scope of the Dutch Medical Research involving Humans Act (Dutch: Wet Medisch-Wetenschappelijk Onderzoek met mensen (WMO)) and a waiver of informed consent was obtained. The NEPHROVIR-3 study was approved by the Ethics Committee (French: Comité de Protection des Personnes) of Ile-De-France IV on January 26th, 2017 and registered (www.clinicaltrials.org, NCT02818738). For both studies, all subjects and/or their parents (if applicable) signed for informed consent. All survey data were collected anonymously.
Results
A total of 118 and 324 unique cases were reported during the observation periods of the studies in the Netherlands (2018–2021) and the Paris area (2017–2021), respectively. The Dutch survey yielded an additional of 10 cases that were initially missed. Thus, 128 and 324 cases were included in the analysis (Table 1).
Following the first cases and rapid spread of the virus, both countries implemented restrictive measures of varying degree. An overview and timeline of the measures can be found in Table 2. Fundamental hygiene rules applied for both countries during the pandemic: keep 1.5-m distance, wash your hands, stay at home and test yourself in case of symptoms, and ventilate rooms.
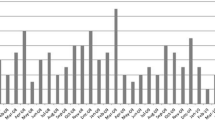
Incidence of INS in the Netherlands
Figure 1a shows the monthly new cases of INS between 2018 and 2021. Overall incidence of INS in children in the Netherlands was 1.21 (95% CI 1.00–1.43) per 100,000 children per year (Table 3a). During the Covid-19 pandemic, incidence was lower (1.14, 95% CI 0.88–1.43) than before the pandemic (1.25, 95% CI 0.97–1.56), but this was not significant (p = 0.61). Overall incidence was higher in boys (p = 0.011) and in children under the age of 7 or under 12 (p < 0.001). When the schools were closed, incidence was significantly lower (0.53, 95% CI 0.15–0.96 vs. 1.31, 95% CI 1.07–1.56, p = 0.017). Other lockdown measures had no effect on incidence (Table 3a). When looking at absolute numbers, no cases occurred during the peak of the first (March, 2020) and second (January, 2021) wave, whereas there was an increase in cases when schools reopened after the summer holidays (September, 2020) and after the second lockdown (March, 2021) (Fig. 2a).
Close-up of the Covid-19 period 2020–2021 with the number of new cases (left axis) and indication of lockdown measures (grey blocks and coloured line below X-axis) and Covid-19-related hospitalisations (30-day average; right axis) in a. the Netherlands and b. Paris area. Grey blocks = Full school closures; Light grey blocks = Partial school closures. Light blue line = fundamental hygiene rules; Green line = “Intelligent” lockdown (Bars and restaurants closed, schools and sports events closed, non-essential shops opened, group size restrictions); Blue line = Partial lockdown (Bars and restaurants closed, non-essential shops opened, group size restrictions); Red line = Complete lockdown (Non-essential shops closed); Black line = Curfew
Incidence of INS in the Paris area
Figure 1b shows the monthly new cases of INS between 2017 and 2021. Overall incidence of INS in children in the Paris area was 2.58 (95% CI 2.30–2.85) per 100,000 children per year (Table 3b). Similar to the Netherlands, incidence in boys (p < 0.001) and young children (p < 0.001) was higher. During the Covid-19 pandemic, the incidence of INS in children was 2.64 (95% CI 2.04–2.90), which was comparable to before the pandemic (2.44, 95% CI 2.30–3.00, p = 0.54). When the schools were closed, incidence was significantly lower (0.94, 95% CI 0.24–1.91 vs. 2.63 95% CI 2.35–2.93, p = 0.049). Subsequent lockdown measures – when schools stayed open – had no effect on incidence (Table 3b). There was an increase in cases when schools reopened in June 2020, while during peaks of hospital admissions for COVID-19 (April 2020), no case of INS was reported in the Paris area (Fig. 2b).
Discussion
The results of this observational study in the Netherlands and the Paris area in France show that incidence of INS was lower when schools were closed and lockdown measures were at their maximum. There was no difference between the period before and during the Covid-19 pandemic in both countries.
It has been assumed that incidence of INS has been stable over the decades [4]. A recent epidemiological study in a multi-ethnic population of Atlanta, United States of America, showed comparable incidence rates over three different 5-year periods [21]. However, during the Covid-19 pandemic, the investigators of the LEARNS and NEPHROVIR-3 study noticed a drop in new onset INS. Based on the theory that viral infections precede or trigger INS onset [14, 15], we hypothesised that the Covid-19 pandemic could impact INS incidence. Since the start of the Covid-19 pandemic, case reports of new onset of INS during SARS-CoV-2 infection have been published both in adults and children [22,23,24], but also reports that viral infections were significantly reduced [25,26,27,28,29,30]. Therefore, we conducted two independent, retrospective population-based studies in two different European regions. Surprisingly, we did not find a difference in incidence between the before and during pandemic INS cohorts in either region. This is in line with findings from Southern California where the number of new cases the year before the pandemic was similar to that of the first year of the pandemic [17]. No higher incidence during the repeated peaks or waves of Covid-19 related hospitalisations – and thus, SARS-CoV-2 burden – was observed. On the contrary, new cases were absent. This may suggest that SARS-CoV-2 is not a specific trigger for INS onset, which was also observed in a recent Italian retrospective study [31] and systematic review of literature [32]. However, it must be noted that the Covid-19 burden in children was low, especially before the emergence of the Omicron variant.
Despite the low burden of SARS-CoV-2 infection in children [33], they were severely affected by the implementation of lockdown measures. The effect of lockdown was largest in the Paris area and when schools were closed. Differences in the severity of the lockdown measures between the countries may explain the difference in the magnitude of the effect of lockdown on the INS incidence. Right when the pandemic hit, social distancing and fundamental hygiene measures were implemented by the governments of both countries. However, considerable differences in the measures existed between countries, but also between subsequent lockdowns. During the first lockdown in France, the measures were stricter than those that followed in the second and third waves of the pandemic. Schools were closed from March 17th until May 11th, 2020, which led to an immediate drop in incidence in March/April 2020. When schools reopened, children of 6 years and older had to wear face masks. Also, strict travel restrictions and time outside the house as well as closing of all non-essential businesses were implemented during first lockdown. This is in contrast to the Netherlands, where schools were closed from March to June, 2020, but businesses were still open, albeit with hygiene measures. Moreover, although discouraged, people were free to travel throughout the country and spend their time outside. On the other hand, schools in the Netherlands were repeatedly closed for longer periods of time. When comparing the three successive lockdowns, there was an increase in the number of new cases, which may reflect the gradual release in the strictness of each lockdown.
Our findings, combined with data on viral infections from the literature, support our hypothesis that the onset of INS is potentially driven by a (viral) infection. This is based on several observations. First, incidence in both regions was lower when schools were closed. The closing of schools seriously impacted the number of peer interactions and/or encounters between children, while working from home, travel restriction and curfew reduced contacts among adults. This did not only contain the spread of SARS-CoV-2, but also resulted in a rapid decrease in incidence of other virus-transmitted infections within weeks [34,35,36]. This is thought to be the result of social distancing (physical distance, fewer encounters, school closings), increasing barriers (face masks), and increased awareness for hygiene (washing hands, the use of disinfectants). Our results indicate that wearing face masks had little to no impact on INS incidence, which is probably explained by the fact that in both regions only children of 12 years or older were obliged to wear a mask in public spaces, including schools (in Paris, the measure was later extended to include all children of 6 years and older). Since INS is a disease that primarily manifests itself in young children with a significantly higher incidence in children < 7 years of age, the children who were impacted are only a small proportion of INS patients and thus had little influence on overall incidence. But even within the age groups that had to wear facemasks, no difference was found.
Second, the impact of reduced viral transmission by minimising social encounters on INS incidence is further underscored by our observation that when the latest school restrictions were lifted in in the Netherlands, this led to a marked increase in new onset INS in the three months following. Almost simultaneously, a peak in respiratory syncytial virus (RSV) occurred in the Netherlands and France [37]. Literature shows that with the phased reduction of the lockdown, different viruses showed different tendencies of re-emerging. There was a steep increase in respiratory viruses after the reopening of schools and public places [38] and after the obligation to wear a facemask was released [39]. In our study, however, there was no effect of wearing facemasks.
Multiple studies have shown that the rate of infection-related hospitalisations in children significantly decreased in the weeks following the first lockdown measures [25,26,27,28, 30]. Although an altered pattern in healthcare-seeking behaviour may have played a role, hospitalisation rates for epilepsy, urinary tract infections or other, more serious health conditions did not change. As INS does not resolve spontaneously, it is unlikely that avoidance of medical care out of fear of contracting Covid-19 is of influence here.
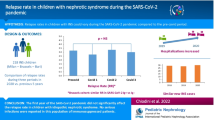
Two studies showed trends towards lower relapse rates of INS during the Covid-19 pandemic [18, 19], while one did find a significant lower relapse rate [17]. We did not include relapse rate in our study, since a substantial proportion of children was included in one of the RCTs (either LEARNS or NEPHROVIR-3) which could have biased the results. Although the association between relapses and triggering infections has been more clearly established for the occurrence of relapses than first onset INS [40,41,42], earlier studies have shown that children with first onset INS had a higher geno- and seroprevalence of EBV than controls [14]. Another study highlighted an association between enterovirus infection and childhood INS onset [15]. This again emphasises the potential role that viruses may play in triggering nephrotic syndrome. Whether this effect is direct or indirect (“second hit”) through a malfunctioning immune response, remains to be elucidated [13].
In addition, a previous dynamic epidemiological study has demonstrated time and space clustering of childhood INS cases in the Paris area [6], arguing for the role of one (or more) environmental triggering factor(s), yet to be identified. Besides the virus hypothesis, environmental pollution may also be a triggering factor. Air pollution has been associated with an increased risk of INS in children in Taiwan [43]. During the spring 2020 lockdown, measures to limit the spread of Covid-19 sharply reduced activities. A major decrease in air pollution levels was observed in metropolitan France and led to a reduction in NO2 and PM concentrations [44]. Again, whether air exposure may have a direct or indirect effect on disease triggering is currently unknown, but the role of other (unknown) environmental factors might have also been modified with lockdowns.
This study has some limitations. Although new cases were prospectively reported to the Dutch study team, the additional survey identified ten more first onset INS patients. The response rate was high, still it was not 100%. New onset INS cases could have been missed, which may have underestimated the incidence. We tried to overcome this by estimating the true number of cases using a Monte Carlo simulation, but it is unknown in which month cases were missed. On the other side, there was a 100% response rate in Paris and this study found a similar change in pattern. Yet, these two independent cohort studies were able to confirm the results of one another. Another limitation was that we could only use descriptive analyses due to the limited amount of data. The low number of cases prevented us from doing extensive analyses to identify an association between the effect of lockdown, lag time (time between implementation of a lockdown measure and its effect) or holidays on INS incidence. Furthermore, the retrospective design prevented us from obtaining samples for antigenic or serological assays to detect concomitant viral infections. Also, because of a high prevalence of asymptomatic forms of SARS-CoV-2 infection in children and a dramatic heterogeneity of testing policies over time, in the vast majority of patients there was no information on whether they had been recently infected with SARS-CoV-2 in the days or weeks preceding INS onset in the electronic patient file. Therefore, we cannot conclude that SARS-CoV-2 does not trigger INS with 100% certainty.
In conclusion, our results suggest a link between INS onset and viral infections in children, although COVID-19 does not appear to be a specific trigger. A significant decrease in incidence was observed in periods when child-to-child interaction was minimised by closing schools and thereby reducing viral transmission in two independent European cohorts. This enabled us to confirm our findings. Since incidence before and during the pandemic was not significantly different, we suggest that a more or less similar number of children are at risk for developing INS over large periods of time, but that in the absence of a (viral) trigger, the disease does not manifest itself. When the trigger remerges, the incidence peaks afterwards. This has been shown in a large epidemiological study in the Paris area (lower incidence in summer) [6] and in a small Japanese study (significantly higher number of new cases in autumn) [45]. Viruses as triggers for INS onset deserve our attention for future studies. With the help of multinational, prospective registry studies of new onset INS, valuable information about trends in incidence and associated factors could be added to the field of paediatric nephrology – especially since INS is a rare disease. Gaining insight into the pathogenesis of INS could provide researchers and clinicians new directions for future research, prevention of the disease, and targeted therapy.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Franke I, Aydin M, Llamas Lopez CE, Kurylowicz L, Ganschow R, Lentze M, Born M (2018) The incidence of the nephrotic syndrome in childhood in Germany. Clin Exper Nephrol 22:126–132
Banh THM, Hussain-Shamsy N, Patel V, Vasilevska-Ristovska J, Borges K, Sibbald C, Lipszyc D, Brooke J, Geary D, Langlois V, Reddon M, Pearl R, Levin L, Piekut M, Licht CPB, Radhakrishnan S, Aitken-Menezes K, Harvey E, Hebert D, Piscione TD, Parekh RS (2016) Ethnic differences in incidence and outcomes of childhood nephrotic syndrome. Clin J Am Soc Nephrol 11:1760–1768
Sharples PM, Poulton J, White RHR (1985) Steroid responsive nephrotic syndrome is more common in Asians. Arch Dis Child 60:1014–1017
Veltkamp F, Rensma LR, Bouts AHM (2021) Incidence and relapse of idiopathic nephrotic syndrome: Meta-analysis. Pediatrics 148:e202002924
El Bakkali L, Pereira RR, Kuik DJ, Ket JCF, Van Wijk JAE (2011) Nephrotic syndrome in The Netherlands: A population-based cohort study and a review of the literature. Pediatr Nephrol 26:1241–1246
Dossier C, Lapidus N, Bayer F, Sellier-Leclerc AL, Boyer O, de Pontual L, May A, Nathanson S, Orzechowski C, Simon T, Carrat F, Deschênes G (2016) Epidemiology of idiopathic nephrotic syndrome in children: endemic or epidemic? Pediatr Nephrol 31:2299–2308
Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, Chan TM, Cook HT, Fervenza FC, Gibson KL, Glassock RJ, Jayne DRW, Jha V, Liew A, Liu ZH, Mejía-Vilet JM, Nester CM, Radhakrishnan J, Rave EM, Reich HN, Ronco P, Sanders JSF, Sethi S, Suzuki Y, Tang SCW, Tesar V, Vivarelli M, Wetzels JFM, Floege J (2021) KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int 100:S1–S276
Shalhoub RJ (1974) Pathogenesis of Lipoid Nephrosis: a Disorder of T-Cell Function. Lancet 304:556–560
Colucci M, Carsetti R, Cascioli S, Casiraghi F, Perna A, Rava L, Ruggiero B, Emma F, Vivarelli M (2016) B Cell Reconstitution after Rituximab Treatment in Idiopathic Nephrotic Syndrome. J Am Soc Nephrol 27:1811–1822
Watts AJB, Keller KH, Lerner G, Rosales I, Collins AB, Sekulic M, Waikar SS, Chandraker A, Riella LV, Alexander MP, Troost JP, Chen J, Fermin D, Yee JL, Sampson MG, Beck LH Jr, Henderson JM, Greka A, Rennke HG, Weins A (2022) Discovery of Autoantibodies Targeting Nephrin in Minimal Change Disease Supports a Novel Autoimmune Etiology. J Am Soc Nephrol 33:238–252
Jamin A, Berthelot L, Couderc A, Chemouny JM, Boedec E, Dehoux L, Abbad L, Dossier C, Daugas E, Monteiro RC, Deschênes G (2018) Autoantibodies against podocytic UCHL1 are associated with idiopathic nephrotic syndrome relapses and induce proteinuria in mice. J Autoimmun 89:149–161
McCarthy ET, Sharma M, Savin VJ (2010) Circulating permeability factors in idiopathic nephrotic syndrome and focal segmental glomerulosclerosis. Clin J Am Soc Nephrol 5:2115–2121
Shimada M, Araya C, Rivard C, Ishimoto T, Johnson RJ, Garin EH (2011) Minimal change disease: A “two-hit” podocyte immune disorder? Pediatr Nephrol 26:645–649
Dossier C, Jamin A, Deschênes G (2017) Idiopathic nephrotic syndrome: The EBV hypothesis. Pediatr Res 81:233–239
Lin JN, Lin CL, Yang CH, Lin MC, Lai CH, Lin HH, Kao CH (2016) Risk of Nephrotic Syndrome following Enteroviral Infection in Children: A Nationwide Retrospective Cohort Study. PLoS One 11:e0161004
World Health Organization (2020) Coronavirus disease 2019 (COVID-19): Situation Report - 51. WHO, Geneva
Crane C, Bakhoum C, Ingulli E (2022) Rates of idiopathic childhood nephrotic syndrome relapse are lower during the COVID-19 pandemic. Pediatr Nephrol 37:2679–2685
Chiodini B, Bellotti AS, Morello W, Bulgaro C, Farella I, Giordano M, Montini G, Ismaili K, Wissing KM (2023) Relapse rate in children with nephrotic syndrome during the SARS-CoV-2 pandemic. Pediatr Nephrol 38:1139–1146
Harambat J, Allard L, Godron-Dubrasquet A (2021) Relapse rate of nephrotic syndrome in the time of COVID-19. Pediatr Nephrol 36:211–212
R Core Team (2020) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria
Londeree J, McCracken CE, Greenbaum LA, Anderson EJ, Plantinga LC, Gillespie SE, Wang C-S (2021) Estimation of childhood nephrotic syndrome incidence: data from the atlanta metropolitan statistical area and meta-analysis of worldwide cases. J Nephrol 35:575–583
Alvarado A, Franceschi G, Resplandor E, Sumba J, Orta N (2021) COVID-19 associated with onset nephrotic syndrome in a pediatric patient: coincidence or related conditions? Pediatr Nephrol 36:205–207
Shah SA, Carter HP (2020) New-Onset Nephrotic Syndrome in a Child Associated With COVID-19 Infection. Front Pediatr 8:471
Cancarevic I, Nassar M, Medina L, Sanchez A, Parikh A, Hosna A, Devanabanda B, Vest M, Ayotunde F, Ghallab M, Omran I (2022) Nephrotic Syndrome in Adult Patients With COVID-19 Infection or Post COVID-19 Vaccine: A Systematic Review. Cureus 14:e29613
Polcwiartek LB, Polcwiartek C, Andersen MP, Østergaard L, Broccia MD, Gislason GH, Køber L, Torp-Pedersen C, Schou M, Fosbøl E, Kragholm K, Hagstrøm S (2021) Consequences of coronavirus disease-2019 (COVID-19) lockdown on infection-related hospitalizations among the pediatric population in Denmark. Eur J Pediatr 180:1955–1963
Van Brusselen D, De Troeyer K, Ter Haar E, Vander Auwera A, Poschet K, Van Nuijs S, Bael A, Stobbelaar K, Verhulst S, Van Herendael B, Willems P, Vermeulen M, De Man J, Bossuyt N, Vanden Driessche K (2021) Bronchiolitis in COVID-19 times: a nearly absent disease? Eur J Pediatr 180:1969–1973
Nagakumar P, Chadwick CL, Bush A, Gupta A (2021) Collateral impact of COVID-19: why should children continue to suffer? Eur J Pediatr 180:1975–1979
Angoulvant F, Ouldali N, Yang DD, Filser M, Gajdos V, Rybak A, Guedj R, Soussan-Banini V, Basmaci R, Lefevre-Utile A, Brun-Ney D, Beaujouan L, Skurnik D (2021) Coronavirus Disease 2019 Pandemic: Impact Caused by School Closure and National Lockdown on Pediatric Visits and Admissions for Viral and Nonviral Infections-a Time Series Analysis. Clin Infect Dis 72:319–322
Dawei Y, Naïm O, Alexis R, Vincent G, Romain G, Valérie S-B, Romain B, Alain L-U, Cécile S, Loganayagi V, Julie T, David S, François A (2021) Baisse des infections virales et viro-induites pédiatriques pendant les confinements en 2020. Médecine thérapeutique / Pédiatrie 23:41–45
Rotulo GA, Percivale B, Molteni M, Naim A, Brisca G, Piccotti E, Castagnola E (2021) The impact of COVID-19 lockdown on infectious diseases epidemiology: The experience of a tertiary Italian Pediatric Emergency Department. Am J Emerg Med 43:115–117
Morello W, Vianello FA, Bulgaro C, Montini G (2022) Epidemiology, severity, and risk of SARS-CoV-2-related relapse in children and young adults affected by idiopathic nephrotic syndrome: a retrospective observational cohort study. Pediatr Nephrol 38:1159–1166
Morello W, Vianello FA, Proverbio E, Peruzzi L, Pasini A, Montini G (2022) COVID-19 and idiopathic nephrotic syndrome in children: systematic review of the literature and recommendations from a highly affected area. Pediatr Nephrol 37:757–764
Naeimi R, Sepidarkish M, Mollalo A, Parsa H, Mahjour S, Safarpour F, Almukhtar M, Mechaal A, Chemaitelly H, Sartip B, Marhoommirzabak E, Ardekani A, Hotez PJ, Gasser RB, Rostami A (2023) SARS-CoV-2 seroprevalence in children worldwide: A systematic review and meta-analysis. EClinicalMedicine 56:101786
Reukers D, van Asten L, Brandsema P, Dijkstra F, Hendriksen J, Hooiveld M, de Lange M, Lanooij S, Niessen F, Teirlinck A, Verstraten C, Meijer A, van Gageldonk-Lafeber A (2021) Annual report Surveillance of COVID-19, influenza and other respiratory infections in the Netherlands: winter 2020/2021. Surveillance van COVID-19, griep en andere luchtweginfecties: winter 2020/2021. Rijksinstituut voor Volksgezondheid en Milieu RIVM
Oh DY, Buda S, Biere B, Reiche J, Schlosser F, Duwe S, Wedde M, von Kleist M, Mielke M, Wolff T, Durrwald R (2021) Trends in respiratory virus circulation following COVID-19-targeted nonpharmaceutical interventions in Germany, January - September 2020: Analysis of national surveillance data. Lancet Reg Health Eur 6:100112
Park KY, Seo S, Han J, Park JY (2021) Respiratory virus surveillance in Canada during the COVID-19 pandemic: An epidemiological analysis of the effectiveness of pandemic-related public health measures in reducing seasonal respiratory viruses test positivity. PLoS One 16:e0253451
van Summeren J, Meijer A, Aspelund G, Casalegno JS, Erna G, Hoang U, Lina B, Vsgi L, de Lusignan S, Teirlinck AC, Thors V, Paget J (2021) Low levels of respiratory syncytial virus activity in Europe during the 2020/21 season: what can we expect in the coming summer and autumn/winter? Eurosurveillance 26:2100639
Poole S, Brendish NJ, Tanner AR, Clark TW (2020) Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir Med 8:e92–e93
Esposito S, Principi N (2020) To mask or not to mask children to overcome COVID-19. Eur J Pediatr 179:1267–1270
Yap H-K, Han EJS, Heng C-K, Gong W-K (2001) Risk factors for steroid dependency in children with idiopathic nephrotic syndrome. Pediatr Nephrol 16:1049–1052
MacDonald NE, Wolfish N, McLaine P, Phipps P, Rossier E (1986) Role respiratory viruses in exacerbations of primary nephrotic syndrome. J Pediatr 108:378–382
Takahashi S, Wada N, Murakami H, Funaki S, Inagaki T, Harada K, Nagata M (2007) Triggers of relapse in steroid-dependent and frequently relapsing nephrotic syndrome. Pediatr Nephrol 22:232–236
Wang C, Tsai JD, Wan L, Lin CL, Wei CC (2022) Association between gaseous air pollutants and idiopathic nephrotic syndrome in children: a 12-year population-based cohort study. Ital J Pediatr 48:70
Adélaïde L, Medina S, Wagner V, de Crouy-Chanel P, Real E, Colette A, Couvidat F, Bessagnet B, Alter M, Durou A, Host S, Hulin M, Corso M, Pascal M (2021) Covid-19 Lockdown in Spring 2020 in France Provided Unexpected Opportunity to Assess Health Impacts of Falls in Air Pollution. Front Sustain Cities 3:643821
Odaka J, Kanai T, Uehara R, Kusano E, Yamagata T (2015) Seasonal variation in first episode of childhood idiopathic steroid-sensitive nephrotic syndrome and adult minimal change nephrotic syndrome. Clin Exper Nephrol 19:146–147
Acknowledgements
The authors would like to thank all participating hospitals and associated local investigators involved in the LEARNS consortium and NEPHROVIR network. A complete list of all participating local investigators in both countries can be found in the Supplementary Material.
Funding
The LEARNS study is funded with a consortium grant from the Dutch Kidney Foundation (CP16.03).
Author information
Authors and Affiliations
Consortia
Contributions
In alphabetical order: Conceptualization: Antonia Bouts, Claire Dossier, Sandrine Florquin, Floor Veltkamp; Methodology: Jesper Kers, Hessel Peters-Sengers, Floor Veltkamp; Formal analysis and investigation: Victoire Thenot, Floor Veltkamp; Writing—original draft preparation: Bas van Lieshout, Carlijn Mussies, Floor Veltkamp, Victoire Thenot; Writing—review and editing: Antonia Bouts, Claire Dossier, Djera Khan, Julien Hogan, Jesper Kers, Hessel Peters-Sengers; Funding acquisition: Antonia Bouts, Claire Dossier; Resources: Bas van Lieshout, Carlijn Mussies, Victoire Thenot, Floor Veltkamp; Supervision: Antonia Bouts, Claire Dossier.
Corresponding author
Ethics declarations
Ethics approval
The LEARNS study was approved by the Ethics Committee of Amsterdam University Medical Centers, location University of Amsterdam, the Netherlands (2017_310). The NEPHROVIR-3 study was approved by the Ethics Committee (Comité de Protection des Personnes) of Ile-De-France IV.
Consent to participate
Written informed consent has been obtained from the parents and/or patients (if applicable).
Consent for publication
Written informed consent has been obtained from the parents and/or patients (if applicable).
Competing interests
None to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Veltkamp, F., Thenot, V., Mussies, C. et al. Incidence of idiopathic nephrotic syndrome during the Covid-19 pandemic in the Paris area (France) and in the Netherlands. Pediatr Nephrol 38, 3681–3692 (2023). https://doi.org/10.1007/s00467-023-06006-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-06006-9