Abstract
Background
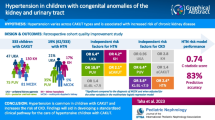
Congenital anomalies of the kidney and urinary tract (CAKUT) are the most frequent causes of childhood chronic kidney disease (CKD). Using a large CAKUT cohort, we sought to identify the predictors of CKD and to develop a prediction model that informs a risk-stratified clinical pathway.
Methods
This was a retrospective cohort study including cases with multicystic dysplastic kidneys (MCDK), unilateral kidney agenesis (UKA), kidney hypoplasia (KH), and posterior urethral valves (PUV). We identified risk factors for CKD (estimated glomerular filtration rate [eGFR] <60 ml/min/1.73 m2) and tested their performance in an adjusted multivariate binary regression model. Prediction probability scores for CKD were used to separate cases likely to develop complications from those not needing specialist follow-up.
Results
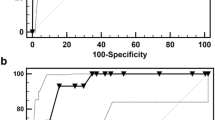
We identified 452 eligible cases of CAKUT with 22% developing CKD. Strongest associations with CKD included primary diagnosis (OR 3.5, 95% CI 2.6–4.6), preterm delivery (OR 2.3, 95% CI 1.2–4.4), non-kidney anomalies (OR 1.8, 95% CI 1.1–3), first eGFR<90 (OR 8.9, 95% CI 4.4–18.1), small kidney size (OR 9, 95% CI 4.9–16.6), and additional kidney anomalies (OR 1.6, 95% CI 1.2–2.8). PUV (OR 4.7, 95% CI 1.5–15.3), first eGFR <90 (OR 4.4, 95% CI 2–9.7), and kidney length to body length ratio <7.9 (OR 4.2, 95% CI 1.9–9.2) were independent predictors of CKD. The regression model had a prediction accuracy of 80% and a prediction probability c-statistic of 0.81.
Conclusion
Using a large combined CAKUT cohort we identified risk factors for CKD. Our prediction model provides the first steps towards a risk-stratified clinical pathway.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information



Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and patient confidentiality. Anonymized and de-identified data are available from the corresponding author upon reasonable request.
References
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ (2012) Epidemiology of chronic kidney disease in children. Pediatr Nephrol 27:363–373
Kerecuk L, Schreuder MF, Woolf AS (2008) Renal tract malformations: perspectives for nephrologists. Nat Clin Pract Nephrol 4:312–325
Charlton JR, Springsteen CH, Carmody JB (2014) Nephron number and its determinants in early life: a primer. Pediatr Nephrol 29:2299–2308
Brenner BM, Mackenzie HS (1997) Nephron mass as a risk factor for progression of renal disease. Kidney Int Suppl 63:S124-127
Cortinovis M, Perico N, Ruggenenti P, Remuzzi A, Remuzzi G (2022) Glomerular hyperfiltration. Nat Rev Nephrol 18:435–451
Bennett KM, Baldelomar EJ, Charlton JR (2022) Delivering on the potential of measuring nephron number in the clinic. Nat Rev Nephrol 18:271–272
Matsell DG, Bao C, White TP, Chan E, Matsell E, Cojocaru D, Bajno L, Catapang M (2023) Kidney length standardized to body length predicts outcome in infants with a solitary functioning kidney. Pediatr Nephrol 38:173–180
Obrycki L, Sarnecki J, Lichosik M, Sopinska M, Placzynska M, Stanczyk M, Mirecka J, Wasilewska A, Michalski M, Lewandowska W, Derezinski T, Pac M, Szwarc N, Annusewicz K, Rekuta V, Azukaitis K, Cekuolis A, Wierzbicka-Rucinska A, Jankauskiene A, Kalicki B, Jobs K, Tkaczyk M, Feber J, Litwin M (2022) Kidney length normative values in children aged 0–19 years - a multicenter study. Pediatr Nephrol 37:1075–1085
Gilad N, Weissmann-Brenner A, Gilboa Y, Dekel B, Achiron R, Perlman S (2021) Multicystic Dysplastic Kidney: Prenatal Compensatory Renal Growth Pattern. J Ultrasound Med 40:2165–2171
Restrepo JM, Torres-Canchala L, Viafara LM, Agredo MA, Quintero AM, Filler G (2021) Renal length z-score for the detection of dysfunction in children with solitary functioning kidney. Acta Paediatr 110:652–658
Poggiali IV, Simoes ESAC, Vasconcelos MA, Dias CS, Gomes IR, Carvalho RA, Oliveira MCL, Pinheiro SV, Mak RH, Oliveira EA (2019) A clinical predictive model of renal injury in children with congenital solitary functioning kidney. Pediatr Nephrol 34:465–474
Marzuillo P, Guarino S, Grandone A, Di Somma A, Diplomatico M, Rambaldi PF, Decimo F, Miraglia Del Giudice E, La Manna A, Polito C (2019) Congenital solitary kidney size at birth could predict reduced eGFR levels later in life. J Perinatol 39:129–134
La Scola C, Ammenti A, Puccio G, Lega MV, De Mutiis C, Guiducci C, De Petris L, Perretta R, Venturoli V, Vergine G, Zucchini A, Montini G (2016) Congenital Solitary Kidney in Children: Size Matters. J Urol 196:1250–1256
Matsell DG, Bao C, Po White T, Chan E, Matsell E, Cojocaru D, Catapang M; Pediatric Nephrology Clinical Pathway Development Team (2021) Outcomes of solitary functioning kidneys-renal agenesis is different than multicystic dysplastic kidney disease. Pediatr Nephrol 36:3673–3680
Matsell DG, Cojocaru D, Matsell EW, Eddy AA (2015) The impact of small kidneys. Pediatr Nephrol 30:1501–1509
Matsell DG, Yu S, Morrison SJ (2016) Antenatal Determinants of Long-Term Kidney Outcome in Boys with Posterior Urethral Valves. Fetal Diagn Ther 39:214–221
Dinkel E, Ertel M, Dittrich M, Peters H, Berres M, Schulte-Wissermann H (1985) Kidney size in childhood. Sonographical growth charts for kidney length and volume. Pediatr Radiol 15:38–43
Vasconcelos MA, Silva AS, Gomes IR, Carvalho RA, Pinheiro SV, Colosimo EA, Yorgin P, Mak RH, Oliveira EA (2019) A clinical predictive model of chronic kidney disease in children with posterior urethral valves. Pediatr Nephrol 34:283–294
Schwartz GJ, Feld LG, Langford DJ (1984) A simple estimate of glomerular filtration rate in full-term infants during the first year of life. J Pediatr 104:849–854
Brion LP, Fleischman AR, McCarton C, Schwartz GJ (1986) A simple estimate of glomerular filtration rate in low birth weight infants during the first year of life: noninvasive assessment of body composition and growth. J Pediatr 109:698–707
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Groen S, Roeleveld N, Westland R, Renkema KY, Steffens MG, Gracchi V, Lilien MR, van Wijk JAE, Feitz WFJ, Schreuder MF, van der Zanden LFM, Solitary Functioning Kidney: Aetiology and Prognosis (SOFIA) study group (2023) Uncovering risk factors for kidney injury in children with a solitary functioning kidney. Kidney Int 103:156–165
Nelson CP, Lee RS, Trout AT, Servaes S, Kraft KH, Barnewolt CE, Logvinenko T, Chow JS (2019) The association of postnatal urinary tract dilation risk score with clinical outcomes. J Pediatr Urol 15(341):e341–e346
McLeod DJ, Sebastiao YV, Ching CB, Greenberg JH, Furth SL, Becknell B (2020) Longitudinal kidney injury biomarker trajectories in children with obstructive uropathy. Pediatr Nephrol 35:1907–1914
McLeod DJ, Ching CB, Sebastiao YV, Greenberg JH, Furth SL, McHugh KM, Becknell B (2019) Common clinical markers predict end-stage renal disease in children with obstructive uropathy. Pediatr Nephrol 34:443–448
Wu CQ, Blum ES, Patil D, Shin HS, Smith EA (2022) Predicting childhood chronic kidney disease severity in infants with posterior urethral valve: a critical analysis of creatinine values in the first year of life. Pediatr Nephrol 37:1339–1345
Klaus R, Lange-Sperandio B (2022) Chronic Kidney Disease in Boys with Posterior Urethral Valves-Pathogenesis. Prog Manag Biomed 10:1894. https://doi.org/10.3390/biomedicines10081894
Westland R, Schreuder MF, Bokenkamp A, Spreeuwenberg MD, van Wijk JA (2011) Renal injury in children with a solitary functioning kidney–the KIMONO study. Nephrol Dial Transplant 26:1533–1541
Trnka P, Hiatt MJ, Tarantal AF, Matsell DG (2012) Congenital urinary tract obstruction: defining markers of developmental kidney injury. Pediatr Res 72:446–454
Perl AJ, Schuh MP, Kopan R (2022) Regulation of nephron progenitor cell lifespan and nephron endowment. Nat Rev Nephrol 18:683–695
Aslam M, Watson AR, Trent Anglia MSG (2006) Unilateral multicystic dysplastic kidney: long term outcomes. Arch Dis Child 91:820–823
Walawender L, Becknell B, Matsell DG (2023) Congenital anomalies of the kidney and urinary tract: defining risk factors of disease progression and determinants of outcomes. Pediatr Nephrol. https://doi.org/10.1007/s00467-023-05899-w
Funding
B.B. is supported by 5R01DK125469 (U.S. National Institutes of Health, NIDDK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors have no conflicts of interest to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Matsell, D.G., Catapang, M. & Becknell, B. Predicting outcomes in children with congenital anomalies of the kidney and urinary tract. Pediatr Nephrol 38, 3407–3415 (2023). https://doi.org/10.1007/s00467-023-05992-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05992-0