Abstract
Background
Renal oligohydramnios (ROH) describes an abnormally low volume of amniotic fluid (AF) during pregnancy. ROH is mostly caused by congenital fetal kidney anomalies. The ROH diagnosis frequently implies an increased risk of peri- and postnatal fetal mortality and morbidity. The present study aimed to evaluate the impact of ROH on pre-and postnatal development in children with congenital kidney anomalies.
Methods
This retrospective study included 168 fetuses with anomalies in the kidney and urinary tract. Based on the amount of AF measured by ultrasound, patients were divided into three groups: normal amniotic fluid (NAF), amniotic fluid in the lower normal range (LAF), and ROH. These groups were compared with respect to prenatal sonographic parameters, perinatal outcomes, and postnatal outcomes.
Results
Among the 168 patients with congenital kidney anomalies, 26 (15%) had ROH, 132 (79%) had NAF, and 10 (6%) had LAF. Of the 26 families affected by ROH, 14 (54%) decided to terminate pregnancy. Of 10 live-born children in the ROH group, 6 (60%) survived the observation time; of these, 5/6 presented with chronic kidney disease, stages I–III, at their last examination. The main differences in postnatal development between the ROH group and the NAF and LAF groups were: restricted height and weight gain, respiratory issues, complicated feeding, and the presence of extrarenal malformations.
Conclusions
ROH is not a mandatory indicator of severe postnatal kidney function impairment. However, children with ROH have complicated peri-and postnatal periods, due to the presence of concomitant malformations, which must be considered in prenatal care.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An evaluation of amniotic fluid (AF) volume plays a major role in the assessment of fetal kidney function. Beginning in the 16th week of gestation, fetal diuresis is responsible for more than half of the amount of AF. Hence, a malfunction in fetal urine production rapidly leads to renal oligohydramnios (ROH) [1]. The most common pathologies associated with ROH are congenital anomalies of the kidney and urinary tract [2]. ROH can lead to the development of pulmonary hypoplasia. Children with ROH tend to have elevated risk of respiratory complications and impaired lung function in infancy [3].
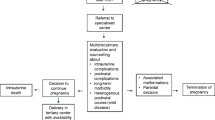
Most of the studies show serious consequences of this diagnosis when we include termination of pregnancy (TOP), survival rate and need for kidney replacement therapy [4,5,6]. Different practices in clinical centers and varying ethical beliefs influence the approach to managing this severe pathology; thus, no standardized management is currently available. Frequently, family counseling is solely carried out by obstetricians [7]. In some cases, multiprofessional teams of healthcare experts (e.g., a gynecologist, pediatric nephrologist, neonatologist, pediatric surgeon, and psychologist) have been employed to improve family counseling for affected families.
The present retrospective study aimed to evaluate ante-, peri-, and postnatal risk factors and the clinical outcome of 168 fetuses with prenatally diagnosed congenital kidney anomalies and different amniotic fluid levels, in a level I perinatal center. Our results will serve as a basis for improving the future counseling of affected families.
Materials and methods
Study population
This retrospective study included 168 pediatric patients who presented with congenital kidney anomalies from 2010–2019 at our level I perinatal center. On the basis of AF volume, the cohort was divided into three groups: normal amniotic fluid volume (NAF), low amniotic fluid volume (LAF), and ROH. ROH was sonographically defined as an amniotic fluid index (AFI) ≤ 5.1 cm and a single deepest amniotic fluid pocket (SDP) ≤ 2 cm. Previous studies have shown that these two measurement methods were valid for evaluating amniotic fluid in oligohydramnios [8, 9]. Patients with AFIs of 5.2 to 8 cm and an SDP of 2.1 to 4 cm were assigned to the LAF group. These three groups were evaluated for antenatal parameters and for perinatal and postnatal development with an elaborate case report form. Then, the three groups were compared with statistical analyses.
Data collection
The collection of ultrasonographic images was performed by specialists in obstetrics. Local guidelines were applied for antenatal ultrasound screening in Germany. They provided three ultrasound examinations, one for each trimester [10]. The lowest AF measurement at any time during the pregnancy determined the assignment to one of the three AF groups. Prenatal information about each mother and child included prenatal suspected diagnoses, gestational week of diagnosis, sex of the fetus, maternal age, extrarenal manifestations, prenatal intervention methods, and whether the parents had decided to undergo TOP. Perinatal parameters were retrieved from natal registries. For all live-born children, data were recorded on the gestational week at birth, birth mode, APGAR scores at 5 min and 10 min, percentile of birth weight (calculated for German neonates according to [11]) and the need for neonatal intensive care. To compare outcomes among the three groups, data on live-born children at last examination were collected until 2019. The postnatal data acquisition included: postnatal diagnosis, calculated percentiles of weight (pediatric calculation for German children according to [12]), and a recent glomerular filtration rate (GFR). The GFR in children aged one year or older was estimated according to the cystatin C formula [13] for children with normal cystatin C laboratory control. Otherwise, GFR was calculated with a creatinine-based bedside formula, according to Schwartz et al. [14]. Additional follow-up parameters were: the number of hospitalizations, dialysis treatment, kidney transplantation, respiratory adaptation, feeding adaption, and time of death, when deceased.
Statistical analysis
Initially, the parameters were analyzed with descriptive statistics. Categorial variables are expressed as the absolute and relative frequencies. Continuous, normally distributed data are expressed as the mean and standard deviation, and non-normally distributed data are expressed as the median and range. The relationship between two categorical variables was tested with the Chi-Square test. For continuous, non-normally distributed and ordinal variables, the Mann–Whitney U test was performed. The Kruskal–Wallis test was performed to compare the three groups: NAF, LAF, and ROH. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for pre-and postnatal parameters to estimate the influence of ROH compared to the two other AF states. P-values < 0.05 were considered statistically significant. All statistical analyses were performed with SPSS Statistics 28.0 software for Mac (SPSS, Chicago, IL, USA).
Results
Prenatal period
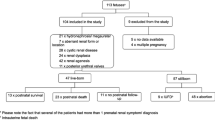
Among 168 fetuses with suspicious ultrasonographic diagnostic findings in the kidney and urinary tract, 26 (15.5%) displayed verified ROH, 132 (78.5%) displayed NAF, and 10 (6%) displayed LAF (Fig. 1). Based on ultrasonic examinations, 99 boys and 62 girls could be identified, but sex could not be determined in 7 children. The median follow-up for all patients was 636 days (range: 1–3148 days). In the ROH group, 14/26 (54%) of the parents chose a TOP, at a mean of 20 gestational weeks. Of the 14 TOPs performed, 10 had concomitant malformations. Among the children with ROH, the mother’s median age was 30 years (range: 19–38) (Table 1 and 2). ROH was diagnosed significantly earlier in the pregnancy (median gestational week 21) than either LAF (median gestational week 35) or NAF (median gestational week 32; p < 0.001). Three patients with ROH received a prenatal interventional treatment, either vesicoamniotic shunting (n = 1) or an amniotic fluid infusion (n = 2).
Outcomes in the three amniotic fluid groups. Patients with NAF and LAF showed significantly higher survival rates than children with ROH (p < 0.001). ROH: renal oligohydramnios; LAF: low amniotic fluid volume; NAF: normal amniotic fluid volume; IUFD: intrauterine fetal death; TOP: termination of pregnancy; CKD: chronic kidney disease
Among the prenatal sonographic patient diagnoses, cystic kidney malformations were predominant in the ROH group (30.8%). In contrast, the primary diagnoses in the NAF and LAF groups were vesicoureteral reflux (VUR) and hydronephrosis (NAF: 54.5%; LAF: 30%) as well as lower urinary tract obstruction for LAF 30% (Table 3). Sonographic measurements of anterior–posterior kidney pelvic diameters (APD) confirmed that antenatal hydronephrosis (ANH) was more common in NAF and LAF groups. Moreover, numerous factors were identified by ORs that influenced ROH development in children (Fig. 2). The parameters most highly associated with ROH development were extrarenal anomalies (OR: 11.6), a diagnosis prior to 20 weeks of gestation (OR: 12.1), and fetal growth disturbances (OR: 9.1). Extrarenal anomalies were defined as any additional genetic or structural anomaly present in other organs.
Perinatal period
From the perinatal period and later, only live-born children (n = 10/26 ROH, n = 124/132 NAF, n = 9/10 LAF) were included in the analyses (Table 2). Birth complications that led to an emergency cesarian section occurred significantly more frequently among children with ROH (n = 2/10), compared to those with LAF (n = 0/9) or NAF (n = 6/124; p < 0.001). Moreover, children with ROH had significantly lower APGAR scores at 5 and 10 min (APGAR 5 min: 8, range: 0–9, p < 0.001; APGAR 10 min: 9, range: 0–10, p = 0.008). Finally, significantly more children with ROH required intensive neonatal care (p < 0.001) and intubation (p < 0.001). However, children in NAF and LAF groups also required intensive care in a considerable number of cases (LAF 44.4%, NAF 26.6%). The three groups received mask ventilation at similar frequencies: LAF: 1/9 (11.1%), NAF: 13/124 (10.5%), and ROH: 1/10 (10%). Comparing the pre-and postnatal diagnoses of the ROH group, the leading diagnosis changed from polycystic kidney disease (prenatal) to complex multiorgan disease (postnatal). In the NAF and LAF groups, the postnatal evaluation of the patient’s leading diagnosis did not differ from the prenatal sonographic evaluation.
Mortality
An outcome analysis of the entire study cohort is shown in Fig. 1. In the ROH group, 10/26 children were born alive. Of these, 6/10 (60%) children survived the observation time. Four ROH patients died in the neonatal period, and of these, two children died due to a syndromic disease and two children died due to pulmonary hypoplasia (both with autosomal recessive kidney disease). In the NAF group, 1/124 children died due to VACTERL syndrome (i.e., vertebral defects, anal atresia, cardiac defects, tracheo-esophageal fistula, kidney anomalies, and limb abnormalities), with cystic kidney malformations and hydronephrosis (Table 4). Among the three groups, survival rates of children with NAF (n = 123/124) and LAF (n = 9/9) were significantly higher than that of children with ROH (n = 6/10; p < 0.001).
In the ROH group, three out of 26 children received therapeutic prenatal interventions. Of these children, one received a vesicoamniotic shunt placement and survived the observation time. Two children received AF infusions; of these, one died intrauterine and the other died in the neonatal period.
Long-term outcome
We next evaluated the three groups (ROH, NAF, LAF) to investigate the relation of ROH on the postnatal development of a child diagnosed with a congenital kidney anomaly. We evaluated the weight percentiles for each of the 168 children at the time of the perinatal counseling conference, at birth, and at the last documented follow-up examination. The ROH group showed a significant drop in the median weight percentile from the prenatal period (48th percentile, range 3–97), through the perinatal period (19th percentile, range 3–97), and the postnatal period (3rd percentile, range 3–75). In the two other groups, the weight percentiles remained relatively constant over the three time periods.
At the last examination, children with ROH presented significantly higher chronic kidney disease (CKD) stages than children in the two other groups (p = 0.044). The GFR was significantly lower in children with ROH (GFR: 65 ml/min) than in children with NAF (GFR: 106 ml/min) or LAF (GFR: 119 ml/min; p < 0.001). However, it should be emphasized that 5/6 children with ROH presented with CKD stages I–III at the last examination. One patient in the ROH group had CKD stage V and received consecutive peritoneal dialysis and a kidney transplantation. In comparison, none of the children in the NAF or LAF groups required kidney replacement therapy. Interestingly, the surviving children in the ROH group did not have significantly longer hospital stays or more surgeries than children with congenital kidney anomalies and either NAF or LAF (NAF: p = 0.131, LAF: p = 0.451). The most relevant differences in postnatal development between children with ROH compared to children with NAF or LAF were the risks of restricted growth and weight gain, respiratory issues, and feeding complications (Fig. 3).
Discussion
Medical and technical progress has enabled accurate diagnostics in prenatal medicine. With the help of ultrasonographic fine diagnostics and fetal MRI, anomalies of the kidney and urinary tract can be well detected, but a detailed consultation is required for families about a child’s diagnosis and prognosis. The present study is one of the few to compare clinical data from the date of prenatal counseling through a postnatal follow-up among children with congenital kidney anomalies and different AF statuses. Other studies such as Mehler et al. and Zilberman et al. also compare different amniotic fluid levels but do not focus on a complete follow-up of all children [6, 15].
Parental decision for TOP
In our ROH cohort, 54% of the parents chose a TOP, which limited the significance of our follow-up results. Other studies have shown lower termination rates, such as the 37% reported by Mehler et al. [6]. It must be emphasized that additional extrarenal malformations were observed in 93% of our TOP cohort, compared to only 53% (20/38) in the TOP cohort of Mehler et al. [6]. High TOP rates among patients with ROH also influenced the results of the PLUTO study (Percutaneous shunting in Lower Urinary Tract Obstruction); their high TOP rate eventually led to early study closure, due to lack of statistical power [16]. Families that were counseled by a local gynecologist and were later included in our study often had a pre-existing opinion about TOP. Independent of the diagnosis severity and ethical beliefs, we recommend effective communication between families, doctors, and professional multidisciplinary support personnel, and access to further testing and appointments [17].
Survival
Survival rates of live-born children differed significantly among the AF groups. As shown in many previous studies, the lack of AF represented a poor prognostic factor for infant survival in the neonatal period [18,19,20,21]. In the present study, four children in the ROH group died in the neonatal period due to respiratory failure or syndromal disease. The survival rates of newborns with NAF and LAF were significantly higher than that of newborns with ROH. Like Krispin et al., we assumed that the survival and outcome of patients with intermediate oligohydramnios, represented by the LAF group, was similar to that observed among children with euhydramnios [22]. Both our NAF and LAF groups predominantly represented urinary flow disorders and LUTO – diagnoses with a good prognosis, when treated early. In contrast, newborns with ROH presented with a remarkable number of extrarenal anomalies, which were associated with multiorgan developmental complications.
We assumed that, once a patient with ROH surpassed the neonatal period, the mortality risk would be very low. This assumption was supported by the fact that 5/6 survivors had only mild to moderate CKD in infancy. Our study confirmed results shown in other studies [6, 20, 21] which showed that ROH was associated with a high neonatal mortality and morbidity. Nevertheless, the postnatal prognosis was favorable for children with ROH.
Prognostic factors
Most pregnant women receive routine surveillance imaging during pregnancy. Consequently, kidney and urinary malformations may be discovered more frequently than before. As a result, caregivers must develop a comprehensive plan before birth [2]. In our study, we emphasized that multidisciplinary counseling must accompany the families, both in the antenatal setting and after birth, to develop a detailed follow-up program. The present study underlined the following facts associated with the development of ROH. In particular, patients who show antenatal malformations in the kidneys and urinary tract, paired with extrarenal anomalies, hypotrophic fetal growth, or a diagnosis of a kidney/urinary tract anomaly ≤ 20 gestational weeks, must draw the doctor’s attention to a possible underlying ROH. Our findings also emphasized that intrauterine growth retardation, detected with ultrasound, in association with ROH represents a poor prognosis, as shown previously by other research groups [23]. Moreover, our results supported the notion that, in particular, infants small for their gestational age that are born with ROH are at increased risk of death, compared to children with NAF [24]. In addition, extrarenal anomalies and an early diagnosis before 20 weeks of gestation are negative predictive factors for patients with ROH [6, 9, 25, 26].
We also showed that the emergency cesarean section and intubation rates in the ROH group were significantly higher than in the two other AF groups. At this point it should be added that children in the NAF and LAF groups are also prone to neonatal complications with subsequent need for intensive care (as shown in Table 2). Therefore, we suggest that delivery should be conducted in a center that provides a neonatal intensive care unit.
One of our most important results was that impaired growth and weight gain and nutritional uptake challenges were significantly higher in the ROH group compared to the NAF and LAF groups. All 168 patients in our cohort had prenatally diagnosed kidney and urinary tract anomalies, which can be associated with growth and weight issues. ROH and intrauterine growth retardation are two conditions that occur together, as many studies have already shown [27,28,29,30]. Our results underlined the notion that a lack of AF contributed even more to growth and weight gain issues. Due to these challenges, medical professionals should adjust treatment and postnatal care for fetuses with ROH as described by Zurowska et al. and Karlberg et al., for children with kidney failure and normal AF volumes [28, 31]. A paragraph of the Karlberg study makes the following statement about children with congenital kidney anomalies and growth impairment: “We speculate that the growth failure during fetal life and the first postnatal months reflects metabolic and/or nutritional influences and the impaired growth at 0.75–1.5 years of age is related to a partial insensitivity to growth hormone”. Based on our data we can state that growth and weight gain are associated with oligohydramnios. Our results also supported the conclusion that children with ROH had a higher long-term risk of respiratory complications, compared to children with NAF or LAF [3]. It is debatable whether restricted growth and weight gain, respiratory issues and feeding complications are independent or a sequence of events, since there were children in the ROH group without respiratory issues who still had feeding and growth complications.
These potential neonatal complications must be taken into consideration by doctors and families in prenatal care. The well-established guidelines in our center emphasized delivery and follow-up requisites for children with ROH. These requisites included the obligatory attendance of obstetricians, neonatologists, pediatric nephrologists, urologists, pulmonologists, and pediatric surgeons; the availability of the latest respiratory support system; and an intensive care unit.
Study limitations
This study had some important limitations. First, the postnatal outcome data included only the patients who survived the neonatal period, which was a rather small patient cohort for the ROH group. Second, the three ROH children who received antenatal therapeutic interventions were not analyzed individually; hence, no firm conclusion could be drawn about the influence of antenatal interventions. Third, although we could draw a conclusion about the health issues associated with the presence of ROH, we did not analyze the quality of life of patients or their families. To achieve even better counseling for families affected by ROH, larger, multicenter prospective studies must be performed.
Conclusion
In summary, this is one of the few studies to compare patients with anomalies of the kidney and urinary tract on the basis of AF volume with long-term follow-up. We identified several risk factors associated with the presence of ROH that should be focused on for appropriate family counseling. Our findings showed that a prenatal diagnosis of ROH was associated with elevated neonatal mortality compared to the mortality of children with normal or mildly reduced amounts of AF. Patients with ROH who survived the neonatal period had acceptable renal function without kidney replacement therapy. Not only the ROH group, but also the NAF and LAF groups have a significant number of pre-and postnatal complications.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Beall MH, van den Wijngaard JPHM, van Gemert MJC, Ross MG (2007) Amniotic fluid water dynamics. Placenta 28:816–823
Moxey-Mims M, Raju TNK (2018) Anhydramnios in the setting of renal malformations: The National Institutes of Health Workshop summary. Obstet Gynecol 131:1069–1079
Chien LN, Chiou HY, Wang CW, Yeh TF, Chen CM (2014) Oligohydramnios increases the risk of respiratory hospitalization in childhood: a population-based study. Pediatr Res 75:576–581
Grijseels EWM (2011) Outcome of pregnancies complicated by oligohydramnios or anhydramnios of renal origin. Prenat Diagn 31:1039–1045
Klaassen I, Neuhaus TJ, Mueller-Wiefel DE, Kemper MJ (2007) Antenatal oligohydramnios of renal origin: long-term outcome. Nephrol Dial Transplant 22:432–439
Mehler K, Gottschalk I, Burgmaier K, Volland R, Buscher AK, Feldkotter M, Keller T, Weber LT, Kribs A, Habbig S (2018) Prenatal parental decision-making and postnatal outcome in renal oligohydramnios. Pediatr Nephrol 33:651–659
Aulbert W, Kemper MJ (2016) Severe antenatally diagnosed renal disorders: background, prognosis and practical approach. Pediatr Nephrol 31:563–574
Madendag Y, Madendag IC, Sahin E, Aydin E, Sahin ME, Acmaz G (2019) How well do the popular ultrasonic techniques estimate amniotic fluid volume and diagnose oligohydramnios, in fact? Ultrasound Q 35:35–38
Hughes DS, Magann EF, Whittington JR, Wendel MP, Sandlin AT, Ounpraseuth ST (2020) Accuracy of the ultrasound estimate of the amniotic fluid volume (Amniotic Fluid Index and Single Deepest Pocket) to identify actual low, normal, and high amniotic fluid volumes as determined by quantile regression. J Ultrasound Med 39:373–378
Schiessl B (2009) Pregnancy screening in Germany. Gynakol Geburtshilfliche Rundsch 49:287–291
Voigt M, Rochow N, Schneider K, Hagenah HP, Scholz R, Hesse V, Wittwer-Backofen U, Straube S, Olbertz D (2014) New percentile values for the anthropometric dimensions of twin neonates: analysis of perinatal survey data of 2007–2011 from all 16 States of Germany. Z Geburtshilfe Neonatol 218:210–217
Hesse V, Schnabel O, Judis E, Cammann H, Hinkel J, Weissenborn J (2016) Längsschnittstudie des aktuellen Wachstums 0- bis 6-jähriger deutscher Kinder: Teil 1. Monatsschrift Kinderheilkunde 164:478–496
Mian AN, Schwartz GJ (2017) Measurement and estimation of glomerular filtration rate in children. Adv Chron Kidney Dis 24:348–356
Schwartz GJ, Muñoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Zilberman Sharon N, Pekar-Zlotin M, Kugler N, Accart Z, Nimrodi M, Melcer Y, Cuckle H, Maymon R (2022) Oligohydramnios: how severe is severe? J Matern Fetal Neonatal Med 35:5754–5760
Morris RK, Malin GL, Quinlan-Jones E, Middleton LJ, Diwakar L, Hemming K, Burke D, Daniels J, Denny E, Barton P, Roberts TE, Khan KS, Deeks JJ, Kilby MD (2013) The Percutaneous shunting in Lower Urinary Tract Obstruction (PLUTO) study and randomised controlled trial: evaluation of the effectiveness, cost-effectiveness and acceptability of percutaneous vesicoamniotic shunting for lower urinary tract obstruction. Health Technol Assess 17:1–232
Hodgson J, Pitt P, Metcalfe S, Halliday J, Menezes M, Fisher J, Hickerton C, Petersen K, McClaren B (2016) Experiences of prenatal diagnosis and decision-making about termination of pregnancy: A qualitative study. Aust N Z J Obstet Gynaecol 56:605–613
Spiro JE, Konrad M, Rieger-Fackeldey E, Masjosthusmann K, Amler S, Klockenbusch W, Schmitz R (2015) Renal oligo- and anhydramnios: cause, course and outcome–a single-center study. Arch Gynecol Obstet 292:327–336
Goto T, Sugiura T, Awaya R, Ueda H, Mizutani E, Ito K, Nagasaki R, Kato T, Saitoh S (2016) Survival of fetuses with severe oligohydramnios. Clin Exper Obstet Gynecol 43:341–344
Loos S, Kemper MJ (2018) Causes of renal oligohydramnios: impact on prenatal counseling and postnatal outcome. Pediatr Nephrol 33:541–545
Klein J, Buffin-Meyer B, Boizard F, Moussaoui N, Lescat O, Breuil B, Fedou C, Feuillet G, Casemayou A, Neau E, Hindryckx A, Decatte L, Levtchenko E, Raaijmakers A, Vayssière C, Goua V, Lucas C, Perrotin F, Cloarec S, Benachi A, Manca-Pellissier MC, Delmas HL, Bessenay L, Le Vaillant C, Allain-Launay E, Gondry J, Boudailliez B, Simon E, Prieur F, Lavocat MP, Saliou AH, De Parscau L, Bidat L, Noel C, Floch C, Bourdat-Michel G, Favre R, Weingertner AS, Oury JF, Baudouin V, Bory JP, Pietrement C, Fiorenza M, Massardier J, Kessler S, Lounis N, Auriol FC, Marcorelles P, Collardeau-Frachon S, Zürbig P, Mischak H, Magalhães P, Batut J, Blader P, Saulnier Blache JS, Bascands JL, Schaefer F, Decramer S, Schanstra JP (2021) Amniotic fluid peptides predict postnatal kidney survival in developmental kidney disease. Kidney Int 99:737–749
Krispin E, Netser T, Wertheimer A, Salman L, Chen R, Wiznitzer A, Hadar E (2019) Induction of labor methods in isolated term oligohydramnios. Arch Gynecol Obstet 299:765–771
Portmann C (2005) P10.21: The outcome of IUGR with oligohydramnios identified at routine morphology ultrasound. Ultrasound Obstet Gynecol 26:444–444
Sasahara J, Ishii K, Umehara N, Oba M, Kiyoshi K, Murakoshi T, Tanemoto T, Ishikawa H, Ichizuka K, Yoshida A, Tanaka K, Ozawa K, Sago H (2016) Significance of oligohydramnios in preterm small-for-gestational-age infants for outcome at 18 months of age. J Obstet Gynaecol Res 42:1451–1456
Ring E, Fotter R (2008) Renal failure and renal transplantation. In: Fotter, R. (eds) Pediatric Uroradiology. Medical Radiology. Springer, Berlin, Heidelberg pp 401–413
Isert S, Müller D, Thumfart J (2020) Factors associated with the development of chronic kidney disease in children with congenital anomalies of the kidney and urinary tract. Front Pediatr 8:298–298
Magann EF, Haas DM, Hill JB, Chauhan SP, Watson EM, Learman LA (2011) Oligohydramnios, small for gestational age and pregnancy outcomes: an analysis using precise measures. Gynecol Obstet Invest 72:239–244
Zurowska AM, Fischbach M, Watson AR, Edefonti A, Stefanidis CJ (2013) Clinical practice recommendations for the care of infants with stage 5 chronic kidney disease (CKD5). Pediatr Nephrol 28:1739–1748
Chauhan SP, Taylor M, Shields D, Parker D, Scardo JA, Magann EF (2007) Intrauterine growth restriction and oligohydramnios among high-risk patients. Am J Perinatol 24:215–221
Lin CC, Sheikh Z, Lopata R (1990) The association between oligohydramnios and intrauterine growth retardation. Obstet Gynecol 76:1100–1104
Karlberg J, Schaefer F, Hennicke M, Wingen AM, Rigden S, Mehls O (1996) Early age-dependent growth impairment in chronic renal failure. European Study Group for Nutritional Treatment of Chronic Renal Failure in Childhood. Pediatr Nephrol 10:283–287
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
This observational study was approved by the local ethics committee and the institutional review board of the University Hospital Jena, Germany (No. 2019–1577).
Competing interests
No funding was received to assist with the preparation of this manuscript.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schulz, A.M., Lauten, A., Lehmann, T. et al. Amniotic fluid content in children with kidney and urinary tract anomalies determines pre- and postnatal development. Pediatr Nephrol 38, 3635–3643 (2023). https://doi.org/10.1007/s00467-023-05988-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05988-w