Abstract
Background
There is paucity of information on rituximab-associated hypogammaglobulinemia (HGG) and its potential infectious consequences in children treated for idiopathic nephrotic syndrome (INS).
Methods
A survey was distributed by the European Society Pediatric Nephrology to its members. It addressed the screening and management practices of pediatric nephrology units for recognizing and treating RTX-associated HGG and its morbidity and mortality. Eighty-four centers which had treated an overall 1328 INS children with RTX responded.
Results
The majority of centers administered several courses of RTX and continued concomitant immunosuppressive therapy. Sixty-five percent of centers routinely screened children for HGG prior to RTX infusion, 59% during, and 52% following RTX treatment. Forty-seven percent had observed HGG prior to RTX administration, 61% during and 47% >9 months following treatment in 121, 210, and 128 subjects respectively. Thirty-three severe infections were reported among the cohort of 1328 RTX-treated subjects, of whom 3 children died. HGG had been recognized in 30/33 (80%) of them.
Conclusions
HGG in steroid-dependent/frequently relapsing nephrotic syndrome (SDNS/FRNS) children is probably multifactorial and can be observed prior to RTX administration in children with SDNS/FRNS. Persistent HGG lasting >9 months from RTX infusion is not uncommon and may increase the risk of severe infections in this cohort. We advocate for the obligatory screening for HGG in children with SDNS/FRNS prior to, during, and following RTX treatment. Further research is necessary to identify risk factors for developing both HGG and severe infections before recommendations are made for its optimal management.
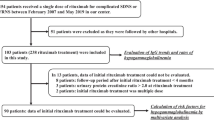
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rituximab (RTX) is a monoclonal antibody against CD20, an antigen expressed on the surface of all circulating B cells excluding plasma cells. Licensed for the treatment of malignancies, vasculitis, and rheumatoid arthritis, it is used off label for the treatment of different autoimmune disease and has been used increasingly for the management of idiopathic nephrotic syndrome (INS) mainly in children with poorly controlled steroid-dependent/frequently relapsing nephrotic syndrome (SDNS/FRNS) [1,2,3]. Recent randomized controlled trials have confirmed its efficacy for this indication, but paucity of data exist on its optimal dosage and short- and long-term safety [4,5,6,7,8,9,10]. Targeting B cells should be the rationale for using RTX in INS, nevertheless evidence exists that RTX can also impact T cells [11, 12]. Depletion of CD20-expressing B cells in the peripheral blood following RTX infusion is rapid and long lasting (several months). Though anti-CD20 antibodies were not expected to influence immunoglobulin levels, the association of RTX use and hypogammaglobulinemia (HGG) has been well established in adults, less so in the pediatric population [13, 14]. A number of risk factors including RTX dose, concomitant immunosuppressive (IMS) treatment, and pre-existing low immunoglobulin levels seem to play a role in its development [15,16,17,18,19]. The reported incidence in adults is relatively low, ranging from 14–20% in adults with malignancies to 3.5–4.2% in subjects with autoimmune diseases [18, 20,21,22]. The clinical significance of this acquired HGG is not fully known but recent publications have shown an increased risk of infections following its use in adults and children [18, 19, 23]. Due to the paucity of data on the incidence of HGG and its consequences in RTX-treated children with INS, a survey was undertaken by the Glomerulonephritis Working Group (WG) of the European Society Pediatric Nephrology (ESPN) addressing the screening and management practices in place in pediatric nephrology centers for the recognition and treatment of this complication and its potential association with severe infections.
Materials and methods
An online survey was distributed by the Glomerulonephritis WG to all ESPN members by email. The survey was web based and developed in the English language. It assessed three domains: center policy for administration of RTX (dose, number of courses, co-administrated drugs, CD19/20 monitoring), screening policy for HGG defined as serum levels below age-standardized reference ranges (prior, during and after 9 months after RTX infusion), its management with IgG replacement therapy (IGRT), and RTX-associated morbidity and mortality (center observations on the number of patients with severe infections requiring hospitalization, data on individual etiology and outcome). The survey consisted of 15 main questions and 25 subquestions of which 29 were close-ended and 11 open-ended. Respondents were able to review and change their answers. Question response types included 20 dichotomous, 8 single choice, 1 multiple choice, and 11 free text responses. The survey was developed by means of Google Documents Application. Participants were informed on the number of questions and time for survey completion. The survey was non-obligatory and no incentives were offered. Answers were stored automatically in a database.
Replies were obtained from 84 centers representing 14 EU countries (Belgium, Czech, Denmark, France, Germany, Greece, Italy, Malta, the Netherlands, Poland, Portugal, Spain, Sweden, and the UK), 2 non-EU countries (Russia and Turkey), and 3 non-European locations (Canada, Israel, and Iran). The response rate was 100% for 28 queries and between 91 and 98% for the remaining 13. Data analysis was performed using STATISTICA (Stat Soft. Inc). The survey results are presented in accordance with the CHERRIES reporting guidelines [24].
Results
Eighty-forty centers reported treating a total number of 1328 children with RTX for steroid-sensitive INS. RTX was given to children with SDNS/FRNS who were poorly controlled with standard steroid and IMS therapy.
Center policies for rituximab administration
The majority (22/84) of centers prescribed RTX independently of age, 23 limited RTX use to children > 5 years and 8 to subjects > 10 years age. RTX was given as a single infusion (375 mg/m2) by 51/84 (60%) centers and as two consecutive infusions by 28/84. Twenty-three units prescribed RTX as a single course of treatment, 44 gave 1–5 courses, and 17 centers had given > 5 RTX courses. The majority (46/61; 75%) routinely assessed CD19/20 counts during treatment, adapting further RTX infusions according to CD19/CD20 reconstitution. Steroids were continued by 47/84 (56%) centers and IMS drugs by 59/84 (70%). Only 15 units discontinued all concomitant treatment with the introduction of anti-CD20 therapy (Table 1).
Recognition of hypogammaglobulinemia
Prior to initial RTX infusion 78/84 centers checked serum IgG levels, 55 routinely (65%). Following RTX administration 81/84 centers checked serum IgG, 50 routinely (59%). Late screening of IgG levels was performed by 79/84 centers, 44 routinely (52%) (Fig. 1).
Nearly half (47%) of the actively screening units (37/78) reported observing HGG in patients prior to RTX administration in a cumulative number of 121 children. Sixty-one percent of actively screening units (49/78) observed HGG in children during RTX treatment, reporting a total number of 210 children with this complication. Forty-seven percent of units (36/76) declared they had observed persistent HGG (> 9 months after RTX infusion) in a total number of 128 children (Fig. 2).
Anti-CD20 antibodies were administered by 28/37 (75%) centers despite preexisting HGG, 19 of them routinely prescribing prophylactic IGRT. During RTX treatment, 30/49 centers (62%) prescribed prophylactic IgG to some of their patients, 19 never used them. When persistent HGG was recognized 10/35 centers routinely administered prophylactic IgG, the majority 17/35 (49%) supplementing IgG to individual patients and 8 centers left HGG untreated. In spite of persistent HGG, 81% (29/36) centers continued IMS or steroid therapy.
Morbidity and mortality associated with RTX in children with INS
Twenty out of eighty-four centers (23%) observed severe infections in children associated with the use of RTX (Fig. 3). Thirty-three severe infections requiring hospitalization were reported among the overall 1328 RTX-treated subjects. The most frequently noted were upper respiratory tract infections and pneumonias of pneumococcal, pneumocystis, and viral etiology (12), followed by sepsis (4) and a variety of viral (myocarditis, herpes infections, meningoencephalitis, measles) and bacterial infections (skin, mastoiditis, pertussis, neuroborreliosis, urinary tract). The majority of children (30/33) demonstrated low serum IgG levels (80%). Three deaths were reported, two due to respiratory tract infections (streptococcus pneumonia, RSV pneumonia) and one due to pneumonia and sepsis of unknown etiology (Table 2).
Number of centers reporting severe infections (morbidity) and death from severe infections (mortality) in children with SDNS/FRNS treated with RTX. Severe infections reported by 20/84 centers in 33/over 1300 children treated with RTX; deaths reported by 3/82 centers in 3/ over 1300 children treated with RTX
Discussion
The ESPN survey on the presence of HGG in RTX-treated children with INS collected information from 84 pediatric nephrology centers treating an overall number of 1328 children, the largest cohort of children subjected to this off-label therapy reported to date. The presented results include the majority of European centers using anti-CD20 antibodies for the treatment of childhood INS, as access to this type of therapy is not universal [25]. The presented results are therefore representative of the contemporary attitudes of mainly European pediatric nephrologists for screening and recognizing HGG in RTX-treated nephrotic subjects.
The reported center policies for RTX administration were surprisingly uniform in spite of lacking consensus guidelines and limited published clinical trials on its use in children for this indication. Only 9% of centers used it solely for older children, the remaining administrating it without age restriction or in children >5 years of age. Concern in prescribing anti-CD20 antibodies to very young children is justified due to the lack of data on its direct and possible long-term effect on their immunological system. Younger age at RTX administration has been reported to be associated with the occurrence of HGG and poorer response to treatment [26, 27]. The protocol most frequently used by centers was cautious with 60% administering a single dose of 375 mg/m2. The majority of units administered more than one course of treatment, reflecting the practice of offering anti-CD20 therapy to children with poorly controlled SDNS/FRNS who demonstrate relapses following previous IMS therapy and also relapsed following RTX use [28]. The frequently observed (82% centers) use of concomitant IMS therapy and/or steroids with RTX increased the children’s risk of developing acquired immunodeficiency.
Routine assessment of immunoglobulins prior to RTX administration was frequent but not a universal practice (2/3 of centers). The center-based design of our survey did not enable an exact calculation of the incidence of HGG in RTX-treated children with SDNS/FRNS. Nevertheless, 47% of pediatric nephrology units had observed pre-RTX low IgG levels in a total number of 121 patients. Data from a large cohort of adults treated for malignancies or autoimmune diseases suggests it may be relatively common as it was noted in nearly half of the screened 655 subjects [18]. The causes of pretreatment HGG have been related to previous IMS/steroid treatment, a previously undiagnosed primary common variable immunodeficiency or urinary loss of immunoglobulins [15, 16, 18]. Both primary and secondary causes of HGG have been recognized as risk factors for the severity of RTX-associated HGG and its related infectious complications [16, 17, 19, 22, 23, 29]. The increased rate of infectious complications in RTX-treated adults with rheumatoid arthritis led to the publication of a consensus statement for the pretreatment assessment of Ig in this disease population [30, 31]. Similarly, we advocate for the routine assessment of immunoglobulin levels prior to initiation of anti-CD20 therapy in INS children. Although 50% of centers reported a policy of prophylactic IGRT, there is currently no consensus regarding its use. The decision may be personalized depending on the age of the patient, vaccine competency, previous history of infections, and possibly severity of HGG.
Transient HGG following RTX infusion is a recognized phenomenon though its incidence is not well described [14, 32]. In most patients, RTX does not reduce immunoglobulin levels significantly as it does not target the antigen specific IgG-producing plasma cells. Between 24 and 34% of adults treated with RTX develop HGG [33, 34]. The survey results and recently published data from a Japanese study suggest that it may have a similar or even higher incidence in children [35]. The management of this complication was not uniform as there is little information to guide clinicians on the optimal method of infection prophylaxis during B cell depletion and HGG. Though antibiotic prophylaxis and IgG replacement therapy have been reported to be effective, only 28% of centers used it routinely, 48% administering them in individual subjects [13, 18, 36]. This attitude seems to be rational, as serious infections requiring hospitalization were reported in less than 2.5% of the total number of RTX-treated children. In a long-term safety study of RTX in 2578 adults with rheumatoid arthritis, serious infections were reported in 7% [34]. Repeated courses of RTX, malignancies, concomitant steroid/IMS treatment, and pretreatment low IgG levels have been implicated as risk factors for significant HGG and severe infections [14, 15, 17, 18, 22, 29]. In a recent single-center Japanese study, the severity of HGG was not significantly associated with the risk of infection in nephrotic children [23].
Persistent HGG was recognized by a similar proportion of centers (47%) and in a similar overall number of children (128) as for pretreatment HGG. This suggests that, at least in some of the children, HGG may have already been present before RTX infusion and confirms the rationale for routine pretreatment evaluation of immunoglobulin levels. The prophylactic use of IGRT varied between units and only 1/3 units gave IGRT routinely for persistent HGG. Due to the survey design, it was not possible to assess the efficacy of IGRT. According to published recommendations for the management of HGG in children treated with B cell targeting therapy for rheumatic diseases, not all patients with HGG require supplementation [37]. Initiation of IGRT may be necessary in the presence of serious, persistent, unusual, or recurrent infections.
The number of 33 reported severe infections associated with the use of RTX in a total cohort of 1328 children with INS was comparatively low, confirming the relative safety of this biologic therapy for children with SDNS/FRNS.
Furthermore, the causal relationship of severe infections and RTX use is probably complex and additional factors may play a role including, but not limited to, previous or concomitant IMS drugs, pre-existing low IgG levels, or RTX dosage. The high frequency of HGG in subjects with severe infections (80%) is highly suggestive that low serum IgG contributes to the development of severe infections in a subset of nephrotic children, though most children with HGG seem to fare well [19, 23].
Though infrequent, serious infections in nephrotic subjects are an important issue and children with this complication require monitoring and rapid management as 3 deaths were recorded among the 33 children reported with severe infections.
In conclusion, we advocate for the routine screening for HGG prior to and post RTX treatment in children with FRNS/SDNS. The survey has demonstrated that if screened for, HGG is a widely recognized complication observed by nearly half of European pediatric nephrology centers using this off-label therapy. The main limitation of the performed survey is the lack of data on the exact incidence of HGG in children treated for INS and the influence of RTX and other IMS drugs on its incidence and duration. Furthermore, the design of the study did not enable a risk analysis for the development of HGG nor the risk of acquiring severe infections in its presence. Further studies are required before recommendations can be issued on the clinical significance and optimal management of HGG in children with idiopathic nephrotic syndrome who have received or will receive RTX.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Payandeh Z, Bahrami AA, Hoseinpoor R, Mortazavi Y, Rajabibazl M, Rahimpour A et al (2019) The applications of anti-CD20 antibodies to treat various B cells disorders. Biomed Pharmacother 109:2415–2426. https://doi.org/10.1016/j.biopha.2018.11.121
Kronbichler A, Windpessl M, Pieringer H, Jayne DRW (2017) Rituximab for immunologic renal disease: what the nephrologist needs to know. Autoimmun Rev 16:633–643. https://doi.org/10.1016/j.autrev.2017.04.007
Ravani P, Bonanni A, Rossi R, Caridi G, Ghiggeri GM (2016) Anti-CD20 antibodies for idiopathic nephrotic syndrome in children. Clin J Am Soc Nephrol 11:710–720. https://doi.org/10.2215/CJN.08500815
Iijima K, Sako M, Nozu K, Mori R, Tuchida N, Kamei K et al (2014) Rituximab for Childhood-onset Refractory Nephrotic Syndrome (RCRNS) Study Group. Rituximab for childhood-onset, complicated, frequently relapsing nephrotic syndrome or steroid-dependent nephrotic syndrome: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet 384:1273–1281. https://doi.org/10.1016/S0140-6736(14)60541-9
Ravani P, Rossi R, Bonanni A, Quinn RR, Sica F, Bodria M et al (2015) Rituximab in children with steroid-dependent nephrotic syndrome: a multicenter, open-label, noninferiority, randomized controlled trial. J Am Soc Nephrol 26:2259–2266. https://doi.org/10.1681/ASN.2014080799
Kallash M, Smoyer WE, Mahan JD (2019) Rituximab use in the management of childhood nephrotic syndrome. Front Pediatr 7:178. https://doi.org/10.3389/fped.2019.00178
Ravani P, Magnasco A, Edefonti A, Murer L, Rossi R, Ghio L et al (2011) Short-term effects of rituximab in children with steroid- and calcineurin-dependent nephrotic syndrome: a randomized controlled trial. Clin J Am Soc Nephrol 6:1308–1315. https://doi.org/10.2215/CJN.09421010
Basu B, Sander A, Roy B, Preussler S, Barua S, Mahapatra TKS et al (2018) Efficacy of rituximab vs tacrolimus in pediatric corticosteroid-dependent nephrotic syndrome: a randomized clinical trial. JAMA Pediatr 172:757–764. https://doi.org/10.1001/jamapediatrics.2018.1323
TaŞdemİr M, Canpolat N, Yildiz N, ÖzÇelİk G, Benzer M, Saygili SK et al (2021) Rituximab treatment for difficult-to-treat nephrotic syndrome in children: a multicenter, retrospective study. Turk J Med Sci. https://doi.org/10.3906/sag-2012-297
Topaloğlu R, Gülhan B, Çelegen K, İnözü M, Hayran M, Düzova A, Ozaltin F (2019) Front Pediatr 7:313. https://doi.org/10.3389/fped.2019.00313
Bhatia D, Sinha A, Hari P, Sopory S, Saini S, Puraswani M et al (2018) Rituximab modulates T- and B-lymphocyte subsets and urinary CD80 excretion in patients with steroid-dependent nephrotic syndrome. Pediatr Res 84:520–526. https://doi.org/10.1038/s41390-018-0088-7
Madanchi N, Bitzan M, Takano T (2017) Rituximab in minimal change disease: mechanisms of action and hypotheses for future studies. Can J Kidney Health Dis 4:2054358117698667. https://doi.org/10.1177/2054358117698667
Marzuillo P, Guarino S, Esposito T, Di Sessa A, Orsini SI, Capalbo D et al (2019) Rituximab-induced IgG hypogammaglobulinemia in children with nephrotic syndrome and normal pre-treatment IgG values. World J Clin Cases 7:1021–1027. https://doi.org/10.12998/wjcc.v7.i9.1021
Parmentier C, Delbet JD, Decramer S, Boyer O, Hogan J, Ulinski T (2020) Immunoglobulin serum levels in rituximab-treated patients with steroid-dependent nephrotic syndrome. Pediatr Nephrol 35:455–462. https://doi.org/10.1007/s00467-019-04398-1
Christou EAA, Giardino G, Worth A, Ladomenou F (2017) Risk factors predisposing to the development of hypogammaglobulinemia and infections post-Rituximab. Int Rev Immunol 36:352–359. https://doi.org/10.1080/08830185.2017.1346092
Khojah AM, Miller ML, Klein-Gitelman MS, Curran ML, Hans V, Pachman LM, Fuleihan RL (2019) Rituximab-associated hypogammaglobulinemia in pediatric patients with autoimmune diseases. Pediatr Rheumatol Online J 17:61. https://doi.org/10.1186/s12969-019-0365-y
Roberts DM, Jones RB, Smith RM, Alberici F, Kumaratne DS, Burns S et al (2015) Rituximab-associated hypogammaglobulinemia: incidence, predictors and outcomes in patients with multi-system autoimmune disease. J Autoimmun 57:60–65. https://doi.org/10.1016/j.jaut.2014.11.009
Barmettler S, Ong MS, Farmer JR, Choi H, Walter J (2018) Association of immunoglobulin levels, infectious risk, and mortality with rituximab and hypogammaglobulinemia. JAMA Netw Open 1:e184169. https://doi.org/10.1001/jamanetworkopen.2018.4169
Takao H, Nishi K, Funaki T, Inoki Y, Osaka K, Nada T, Yokota S, Sato M, Ogura M, Ishikura K, Ishiguro A, Kamei K (2022) Changes in patterns of infection associated with pediatric idiopathic nephrotic syndrome: a single-center experience in Japan. J Pediatr. https://doi.org/10.1016/j.jpeds.2022.10.005
McLaughlin P, Grillo-López AJ, Link BK, Levy R, Czuczman MS, Williams ME et al (1998) Rituximab chimeric anti-CD20 monoclonal antibody therapy for relapsed indolent lymphoma: half of patients respond to a four-dose treatment program. J Clin Oncol 16:2825–2833. https://doi.org/10.1200/JCO.1998.16.8.2825
Cabanillas F, Liboy I, Pavia O, Rivera E (2006) High incidence of non-neutropenic infections induced by rituximab plus fludarabine and associated with hypogammaglobulinemia: a frequently unrecognized and easily treatable complication. Ann Oncol 17:1424–1427. https://doi.org/10.1093/annonc/mdl141
van Vollenhoven RF, Emery P, Bingham CO 3rd, Keystone EC, Fleischmann R, Furst DE et al (2010) Longterm safety of patients receiving rituximab in rheumatoid arthritis clinical trials. J Rheumatol 37:558–567. https://doi.org/10.3899/jrheum.090856
Inoki Y, Nishi K, Sato M, Ogura M, Kamei K (2022) The association between hypogammaglobulinemia severity and infection risk in rituximab-treated patients with childhood-onset idiopathic nephrotic syndrome. Pediatr Nephrol. https://doi.org/10.1007/s00467-022-05652-9
Eysenbach G (2004) Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res 6:e34. https://doi.org/10.2196/jmir.6.3.e34
Prikhodina L, Ehrich J, Shroff R, Topaloglu R, Levtchenko E, European Society for Paediatric Nephrology (2020) The European Society for Paediatric Nephrology study of pediatric renal care in Europe: comparative analysis 1998-2017. Pediatr Nephrol 35:103–111. https://doi.org/10.1007/s00467-019-04378-5
Colucci M, Carsetti R, Serafinelli J, Rocca S, Massella L, Gargiulo A et al (2019) Prolonged impairment of immunological memory after anti-CD20 treatment in pediatric idiopathic nephrotic syndrome. Front Immunol 10:1653. https://doi.org/10.3389/fimmu.2019.01653
Chan EY, Webb H, Yu E, Ghiggeri GM, Kemper MJ, Ma AL et al (2020) Both the rituximab dose and maintenance immunosuppression in steroid-dependent/frequently-relapsing nephrotic syndrome have important effects on outcomes. Kidney Int 97:393–401. https://doi.org/10.1016/j.kint.2019.09.033
Cattran DC, Feehally J, Cook T, Liu ZH et al (2012) Kidney disease: improving global outcomes (KDIGO) glomerulonephritis work group. kdigo clinical practice guideline for glomerulonephritis. Kidney Int Suppl 2:139–274. https://doi.org/10.1038/kisup.2012.9
Trivin C, Tran A, Moulin B, Choukroun G, Gatault P, Courivaud C et al (2017) Infectious complications of a rituximab-based immunosuppressive regimen in patients with glomerular disease. Clin Kidney J 10:461–469. https://doi.org/10.1093/ckj/sfw101
Kado R, Sanders G, McCune WJ (2016) Suppression of normal immune responses after treatment with rituximab. Curr Opin Rheumatol 28:251–258. https://doi.org/10.1097/BOR.0000000000000272
Buch MH, Smolen JS, Betteridge N, Breedveld FC, Burmester G, Dörner T et al (2011) Rituximab Consensus Expert Committee. Updated consensus statement on the use of rituximab in patients with rheumatoid arthritis. Ann Rheum Dis 70:909–920. https://doi.org/10.1136/ard.2010.144998
Delbe-Bertin L, Aoun B, Tudorache E, Lapillone H, Ulinski T (2013) Does rituximab induce hypogammaglobulinemia in patients with pediatric idiopathic nephrotic syndrome? Pediatr Nephrol 28:447–451. https://doi.org/10.1007/s00467-012-2361-z
Marco H, Smith RM, Jones RB, Guerry MJ, Catapano F, Burns S et al (2014) The effect of rituximab therapy on immunoglobulin levels in patients with multisystem autoimmune disease. BMC Musculoskelet Disord 15:178. https://doi.org/10.1186/1471-2474-15-178
van Vollenhoven RF, Fleischmann RM, Furst DE, Lacey S, Lehane PB (2015) Longterm safety of rituximab: final report of the rheumatoid arthritis global clinical trial program over 11 years. J Rheumatol 42:1761–1766. https://doi.org/10.3899/jrheum.150051
Inoki Y, Kamei K, Nishi K, Sato M, Ogura M, Ishiguro A (2022) Incidence and risk factors of rituximab-associated hypogammaglobulinemia in patients with complicated nephrotic syndrome. Pediatr Nephrol 37:1057–1066. https://doi.org/10.1007/s00467-021-05304-4
Roberts DM, Jones RB, Smith RM, Alberici F, Kumaratne DS, Burns S et al (2015) Immunoglobulin G replacement for the treatment of infective complications of rituximab-associated hypogammaglobulinemia in autoimmune disease: a case series. J Autoimmun 57:24–29. https://doi.org/10.1016/j.jaut.2014.11.004
Wijetilleka S, Jayne DR, Mukhtyar C, Ala A, Bright PD, Chinoy H, Harper L, Kazmi MA, Kiani-Alikhan S, Li CK, Misbah SA, Oni L, Price-Kuehne FE, Salama AD, Workman S, Wrench D, Karim MY (2019) Recommendations for the management of secondary hypogammaglobulinaemia due to B cell targeted therapies in autoimmune rheumatic diseases. Rheumatology (Oxford) 58:889–896. https://doi.org/10.1093/rheumatology/key394
Acknowledgements
Endén K.: Department of Paediatrics, Tampere University Hospital, Tampere, Finland; Oh J.: University Medical Center Hamburg-Eppendorf, Hamburg, Germany; Tsygin A.: Federal State Budgetary Institution “Scientific Centre of Children Health” under the Russian Academy of Medical Sciences, Moscow, Russia; Grenda R.: The Children’s Memorial Health Institute, Warsaw, Poland; Raes A.: Department of Pediatric Nephrology, Ghent University Hospital, 9000 Ghent, Belgium; Van Hoeck Koen J.M.: Department of Pediatrics, Antwerp University Hospital, Edegem, Belgium; Adams B.: Hôpital Universitaire des Enfants Reine Fabiola HUDERF·Department of Nephrology-dialysis; Aksenova M.: Scientific Clinical Institution of Pediatrics of Russian Medical University, Moscow·nephrology; Ranchin B.: Pediatric Nephrology Unit, Hôpital Femme Mere Enfant, Hospices Civils de Lyon, Lyon, France; Hooman N.: Aliasghar Clinical Research Development Center, Alkiasghar Children Hospital, University of Medical Sciences (IUMS) Tehera, Iran; Ogarek I.: Department of Pediatric Nephrology and Hypertension CMUJ in Cracow, Poland; Seeman T.: Department of Pediatrics and Biomedical Center, 2nd Faculty of Medicine and Faculty of Medicine in Pilsen, Charles University in Prague, Czech Republic; Fila M.: Centre Hospitalier Universitaire de Montpellier , Department de pediatrie; Oni L.: Department of Paediatric Nephrology, Liverpool Health Partners, Alder Hey Children’s NHS Foundation Trust Hospital, Liverpool, UK; Mir S.: Department of Pediatrics, Pediatric Nephrology Units, Faculty of Medicine, Ege University, Izmir, Turkey; Novo R.: Pediatric Nephrology Unit, Hôpital Jeanne de Flandre, Centre Hospitalier Universitaire de Lille, Lille, France; Stabouli S.: 1st Department of Pediatrics, School of Medicine, Faculty of Health Sciences, Aristotle University Thessaloniki, Hippokratio Hospital; Vara-Martín J.: Pediatric Nephrology, Pediatrics, University Hospital 12 Octubre, Madrid, Spain; van Wijk J.A.E.: Department of Pediatric Nephrology, VU University Medical Center, Amsterdam; Ehren R.: Children’s and Adolescents’ Hospital, Pediatric Nephrology, University of Cologne, Germany; Bekassy Z.: Department of Pediatrics, Clinical Sciences Lund, Lund University, Lund, Sweden; Herthelius M.: Astrid Lindgren Children’s Hospital, Karolinska University Hospital, Stockholm, Sweden; Becherucci F.: Nephrology and Dialysis Unit, Meyer Children’s University Hospital, Florence, Italy; Shasha-Lavsky H.: Pediatric Nephrology Unit, Galilee Medical Center, Nahariya, Israel; Santos F.: Hospital Universitario Central de Asturias (HUCA), University of Oviedo, Oviedo, Spain; Feldkötter M.: Department of Pediatrics, Division of Pediatric Nephrology, University Children’s Hospital Zurich, Zurich, Switzerland; Pańczyk-Tomaszewska M.: Medical University of Warsaw, Poland: Department of Pediatrics and Nephrology; Harambat J.: Department of Pediatric Nephrology, Centre Hospitalier Universitaire de Bordeaux Groupe hospitalier Pellegrin, Bordeaux, France; Grima D.: Cornerstone Research Group, Burlington, Ontario, Canada; Gökçe I.: Department of Pediatric Nephrology, Marmara University School of Medicine, Istanbul, Turkey; Teixeira A.: Centro Materno-Infantil do Norte, Centro Hospitalar do Porto, Porto, Portugal; Licht C.: Department of Pediatric Nephrology, The Hospital for Sick Children, Toronto, Canada; Schmidt I.M.: Department of Paediatrics and Adolescent Medicine, Juliane Marie Centre, Rigshospitalet University Hospital, Copenhagen, Denmark; Brandström P.: Pediatric UroNephrology Center, The Queen Silvia Children’s Hospital, The Sahlgrenska Academy at the University of Gothenburg, Sweden; Dinçel N.: Department of Pediatric Nephrology, University of Health Sciences Dr. Behc¸et Uz Child Disease and Pediatric Surgery Training and Research Hospital, İzmir, Turkey.
Collaborators: Members of ESPN Glomerulonephritis Working Group:
Alpay H. – Marmara University, Istanbul, Turkey
Andersen R. - Aarhus University Hospital, Denmark.
Ariceta G. - Hospital MaternoInfantil de la Vall d’Hebron, Barcelona, Spain
Atmış B. - Cukurova University Faculty of Medicine, Adana, Turkey.
Bayrakçı U.S. - Ankara Yıldırım Beyazıt Unıversity Faculty of Medicine, Ankara, Turkey
Esrea B. - Baskent University Hospital, Ankara, Turkey
Baudouin V. - Robert Debré Hospital, APHP, Paris, France.
Bervina N. - Orenburg Regional Children's Hospital , Nephrology Department
Benetti E. - AOP-University of Padova, Italy
Berard E. - Hôpitaux pédiatriques universitaires de Nice, Nice, France,
Bjerre A. - Oslo University Hospital, Rikshospitalet, Oslo, Norway.
Bouts A. - Amsterdam University, The Netherlands.
Christian M. - Nottingham Children's Hospital at the QMC, UK
Couderc A. - APHP, Hôpital Robert-Debré, Paris, France
Dehoorne J. - Ghent University, Gent, Belgium.
Deschenes G. - Paris University Hospital Robert Debré, Paris, France.
Dossier C. - APHP, Hôpital Robert-Debré, Paris, France.
Düşünsel R. - Erciyes University Faculty of Medicine, Kayseri, Turkey
Ekinci Z. - Kocaeli Academy for Solidarity, Kocaeli, Turkey.
Emma F. - Bambino Gesù Children's Hospital, IRCCS, Rome, Italy;
Espinoza L. - Servicio de Nefrología Pediátrica, Hospital La Paz, Madrid, España
Gianviti A. - Children's Hospital Bambino Gesù, IRCCS, Rome, Italy.
Herrero Goñi M. - Hospital de Cruces, Baracaldo, Spain.
Guido G. - Ospedale S. Eugenio, Roma, Italia.
Ghio L. - Fondazione Ca’ Granda, IRCCS Ospedale Maggiore, Policlinico Milano, Italy
Groothoff J. - Emma Children's Hospital, Amsterdam UMC, University of Amsterdam, The Netherlands.
Hacıhamdioğlu D.Ö. - MedicalPark Goztepe Hospital, Istanbul, Turkey.
Espino Hernández M. - Pediatrics, University Hospital 12 Octubre, Madrid, Spain.
Jankauskiene A. - Pediatric Center, Vilnius University, Vilnius, Lithuania
Kagan M. - Orenburg Regional Children’s Hospital, Orenburg, Russia;
Kemper M. - University Hospital Hamburg-Eppendorf, Hamburg, Germany;
Kovacevic M. - Institute for Child and Youth Health Care in Novi Sad, Serbia
Kohl S. - University of Cologne, Faculty of Medicine and University Hospital Cologne, Cologne, Germany.
Kramar R.T. - Karolinska Institutet, Sweden
López-González M. - University Hospital Vall d'Hebron, Barcelona, Spain
Aris A.M. - Madrid Hospital Vall d’Hebron, Barcelona, Spain
Maringhini S. - Ospedale dei Bambini “G. Di Cristina” A.R.N.A.S. Palermo, Italy
Marlais M. - Great Ormond Street Hospital for Children NHS Foundation Trust, London, UK
Melgosa M. - La Paz University Hospital, Madrid, Spain.
Mitsioni A. - P. & A. Kyriakou Children’s Hospital, Athens, Greece
Montini G. - University of Milan, Ospedale Maggiore Policlinico, Milano, Italy
Moczulska A. - Jagiellonian University Medical College, Cracow, Poland
Murer L. - AOP-University of Padova, Italy
Obukhova V. - Research Institute of Pediatrics and Children Surgery, Moscow, Russia
Oh J. - University Medical Center Hamburg-Eppendorf, Hamburg, Germany
Ortega P. - Hospital Universitari La Fe, Valencia, Spain
Özçakar Z.B. - Ankara University School of Medicine, Ankara, Turkey.
Ulinski T. - Armand-Trousseau Hospital, Paris, France
Pasini A. - Azienda Ospedaliero Universitaria, Policlinico Sant’Orsola-Malpighi, Bologna, Italy.
Papalia T. - Azienda Ospedaliera, Italy, Cosenza
Paunova S. - Pirogov Russian National Research Medical University, Moscow, Russia
Pena A. - Hospital Infantil La Paz, Madrid, Spain.
Pecoraro C. - Children Hospital Santobono-Pausilipon, Naples Italy
Petrosyan E. - Russian National Research Medical University, Moscow, Russia
Peruzzi L. - Regina Margherita Children’s Hospital, Città della Salute e della Scienza di Torino, Turin, Italy
Printza N. - Hippokration General Hospital, Aristotle University, Thessaloniki, Greece.
Prikhodina L. - Pirogov Russian National Research Medical University, Moscow, Russia
Pietrement C. - Centre Hospitalier Universitaire de Reims, France
Rittig S. - Aarhus University Hospital, Aarhus, Denmark
Rodrigo D. - University Institute of Health Sciences Research (IUNICS-IdISPa), University of Balearic Islands, Palma de Mallorca, Spain;
Savenkova N. - Saint-Petersburg State Pediatric Medical University, St Petersburg, Russia
Saraga M. - School of Medicine, University of Split, Split, Croatia
Sever F.L. - İstanbul University Cerrahpaşa Faculty of Medicine, İstanbul, Turkey
Schreuder M. - Radboud University Medical Center, Radboud Institute for Molecular Life Sciences, Amalia Children’s Hospital, Nijmegen, The Netherlands.
Szczepanska M. – Faculty of Medical Sciences in Zabrze, SUM in Katowice, Poland
Tasic V. - University Children’s Hospital, Skopje, North Macedonia.
Tonshoff B. - University Children’s Hospital Heidelberg, Heidelberg, Germany.
Tullus K. - Great Ormond Street NHS Foundation Trust Hospital, London, UK.
Vara J. - Martin Hospital Universitario 12 de Octubre, Madrid, Spain
Vande Walle J. - Safepedrug, University Hospital Gent, Gent, Belgium
Volokhina E. - Amalia Children’s Hospital Radboud University Medical Center Nijmegen, The Netherlands.
Zieg J. - Second Medical Faculty, Motol University Hospital, Charles University, Prague, Czech Republic.
Waters A. - Great North Children’s Hospital, Newcastle Upon Tyne, UK.
Weber L.T. - University Hospital of Cologne, Cologne, Germany
Webbe N. - University of Manchester, Manchester Academic Health Science Centre, Royal Manchester Children’s Hospital, Manchester, UK
Wasiak M. - Department of Pediatrics and Nephrology, Medical University of Warsaw, Warsaw, Poland.
Funding
This study was supported by ESPN—European Society Pediatric Nephrology. No other funding was received.
Role of funder/sponsor (if any)Dissemination of survey through membership emails, technical support in data collection.
Author information
Authors and Affiliations
Consortia
Contributions
Aleksandra Zurowska MD, PhD conceptualized and designed the study, designed the data collection instruments, collected data, coordinated and supervised data collection, drafted the initial manuscript, and reviewed and revised the manuscript. Magdalena Drozynska-Duklas conceptualized and designed the study, designed the data collection instruments, collected data, carried out the initial analyses, drafted the initial manuscript, and reviewed and revised the manuscript. Rezan Topaloglu collected data, critically reviewed the manuscript for important intellectual content. Antonia Bouts collected data, critically reviewed the manuscript for important intellectual content. Olivia Boyer collected data, critically reviewed the manuscript for important intellectual content. Mohan Shenoy collected data, critically reviewed the manuscript for important intellectual content. Marina Vivarelli collected data, critically reviewed the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
1. Marina Vivarelli declared potential conflict of interests:
- Grants – Alexion
- Sponsored clinical trials – Chinook, Novartis, Bayer, Rche, Apellis, Travere, Alexion, Chemocentrix
- Lectures – Travere, Alexion, WebMD
- Consultancy fees – Novartis, Biocryst, Roche
- Advisory board – Novartis
2. Aleksandra Zurowska declared potential conflict of interests: lectures for Swixx BioPharma
3. Mohan Shenoy declared potential conflict of interests: advisory board – Novartis
4. Olivia Boyer declared potential conflict of interests: consultancy fees – Rocher
5. Magdalena Drozynska-Duklas – no conflict of interests to disclose
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A complete list of ESPN Glomerulonephritis WG appears below.
Supplementary Information
Graphical Abstract
(PPTX 151 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zurowska, A., Drozynska-Duklas, M., Topaloglu, R. et al. Rituximab-associated hypogammaglobulinemia in children with idiopathic nephrotic syndrome: results of an ESPN survey. Pediatr Nephrol 38, 3035–3042 (2023). https://doi.org/10.1007/s00467-023-05913-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05913-1