Abstract
Background
While hyperkalemia is well described in adult chronic kidney disease (CKD), large studies evaluating potassium trends and risk factors for hyperkalemia in pediatric CKD are lacking. This study aimed to characterize hyperkalemia prevalence and risk factors in pediatric CKD.
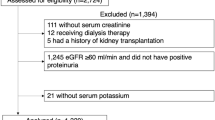
Methods
Cross-sectional analysis of Chronic Kidney Disease in Children (CKiD) study data evaluated median potassium levels and percentage of visits with hyperkalemia (K ≥5.5 mmoL/L) in relation to demographics, CKD stage, etiology, proteinuria, and acid–base status. Multiple logistic regression was used to identify risk factors for hyperkalemia.
Results
One thousand and fifty CKiD participants with 5183 visits were included (mean age 13.1 years, 62.7% male, 32.9% self-identifying as African American or Hispanic). A percentage of 76.6% had non-glomerular disease, 18.7% had CKD stage 4/5, 25.8% had low CO2, and 54.2% were receiving ACEi/ARB therapy. Unadjusted analysis identified a median serum potassium level of 4.5 mmol/L (IQR 4.1–5.0, p <0.001) and hyperkalemia in 6.6% of participants with CKD stage 4/5. Hyperkalemia was present in 14.3% of visits with CKD stage 4/5 and glomerular disease. Hyperkalemia was associated with low CO2 (OR 7.72, 95%CI 3.05–19.54), CKD stage 4/5 (OR 9.17, 95%CI 4.02–20.89), and use of ACEi/ARB therapy (OR 2.14, 95%CI 1.36–3.37). Those with non-glomerular disease were less frequently hyperkalemic (OR 0.52, 95%CI 0.34–0.80). Age, sex, and race/ethnicity were not associated with hyperkalemia.
Conclusions
Hyperkalemia was observed more frequently in children with advanced stage CKD, glomerular disease, low CO2, and ACEi/ARB use. These data can help clinicians identify high-risk patients who may benefit from earlier initiation of potassium-lowering therapies.
Graphical Abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Data Availability
Data in this manuscript were collected by the Chronic Kidney Disease in children prospective cohort study (CKiD) and can be requested via the CKiD website (https://statepi.jhsph.edu/ckid).
References
Valdivielso JM, Balafa O, Ekart R, Ferro C et al (2021) Hyperkalemia in chronic kidney disease in the new era of kidney protection therapies. Drugs 81:1467–1489. https://doi.org/10.1007/s40265-021-01555-5
Whittaker CF, Miklich MA, Patel RS, Fink JC (2018) Medication safety principles and practice in CKD. Clin J Am Soc Nephrol 13:1738–1746. https://doi.org/10.2215/CJN.00580118
Gilligan S, Raphael KL (2017) Hyperkalemia and hypokalemia in CKD: prevalence, risk factors, and clinical outcomes. Adv Chronic Kidney Dis 24:315–318. https://doi.org/10.1053/j.ackd.2017.06.004
Luo J, Brunelli SM, Jensen DE, Yang A (2016) Association between serum potassium and outcomes in patients with reduced kidney function. Clin J Am Soc Nephrol 11:90–100. https://doi.org/10.2215/CJN.01730215
Nakhoul GN, Huang H, Arrigain S, Jolly S et al (2015) Serum potassium, end-stage renal disease and mortality in chronic kidney disease. Am J Nephrol 41:456–463. https://doi.org/10.1159/000437151
DuBose TD (2017) Regulation of potassium homeostasis in CKD. Adv Chronic Kidney Dis 24:305–314. https://doi.org/10.1053/j.ackd.2017.06.002
Chan E, Ma A, Tullus K (2021) When should we start and stop ACEi/ARB in paediatric chronic kidney disease? Pediatr Nephrol 36:1751–1764. https://doi.org/10.1007/s00467-020-04788-w
van den Belt SM, Heerspink HJL, Kirchner M, Gracchi V et al (2020) Discontinuation of RAAS inhibition in children with advanced CKD. Clin J Am Soc Nephrol 15:625–632. https://doi.org/10.2215/CJN.09750819
Abraham AG, Betoko A, Fadrowski JJ, Pierce C et al (2017) Renin-angiotensin II-aldosterone system blockers and time to renal replacement therapy in children with CKD. Pediatr Nephrol 32:643–649. https://doi.org/10.1007/s00467-016-3512-4
Wong H, Mylrea K, Feber J, Drukker A, Filler G (2006) Prevalence of complications in children with chronic kidney disease according to KDOQI. Kidney Int 70:585–590. https://doi.org/10.1038/sj.ki.5001608
Furth SL, Cole SR, Moxey-Mims M, Kaskel F et al (2006) Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin J Am Soc Nephrol 1:1006–1015. https://doi.org/10.2215/CJN.01941205
Pierce CB, Muñoz A, Ng DK, Warady BA, Furth SL, Schwartz GJ (2021) Age- and sex-dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int 99:948–956. https://doi.org/10.1016/j.kint.2020.10.047
National Kidney Foundation (2002) K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 39(2 Suppl 1):S1-266
Harambat J, Kunzmann K, Azukaitis K, Bayazit A et al (2017) Metabolic acidosis is common and associates with disease progression in children with chronic kidney disease. Kidney Int 92:1507–1514. https://doi.org/10.1016/j.kint.2017.05.006
Brown DD, Roem J, Ng DK, Reidy K et al (2020) Low serum bicarbonate and CKD progression in children. Clin J Am Soc Nephrol 15:755–765. https://doi.org/10.2215/CJN.07060619
Brown DD, Carroll M, Ng DK, Levy R et al (2022) Longitudinal associations between low serum bicarbonate and linear growth in children with CKD. Kidney360 3:666–676. https://doi.org/10.34067/KID.0005402021
Kim T, Rhee CM, Streja E, Soohoo M et al (2017) Racial and ethnic differences in mortality associated with serum potassium in a large hemodialysis cohort. Am J Nephrol 45:509–521. https://doi.org/10.1159/000475997
Eriguchi R, Obi Y, Soohoo M, Rhee C et al (2019) Racial and ethnic differences in mortality associated with serum potassium in incident peritoneal dialysis patients. Am J Nephrol 50:361–369. https://doi.org/10.1159/000502998
Leon SJ, Whitlock R, Rigatto C, Komenda P et al (2022) Hyperkalemia-related discontinuation of renin-angiotensin-aldosterone system inhibitors and clinical outcomes in CKD: a population-based cohort study. Am J Kidney Dis 80:164-173.e1. https://doi.org/10.1053/j.ajkd.2022.01.002
Palmer BF, Clegg DJ (2022) Managing hyperkalemia to enable guideline-recommended dosing of renin-angiotensin-aldosterone system inhibitors. Am J Kidney Dis 80:158–160. https://doi.org/10.1053/j.ajkd.2022.02.012
National Kidney Foundation (2009) KDOQI clinical practice guideline for nutrition in children with CKD: 2008 update. Am J Kidney Dis 53:S11–S104. https://doi.org/10.1053/j.ajkd.2008.11.017
Desloovere A, Renken-Terhaerdt J, Tuokkola J, Shaw V et al (2021) The dietary management of potassium in children with CKD stages 2–5 and on dialysis-clinical practice recommendations from the Pediatric Renal Nutrition Taskforce. Pediatr Nephrol 36:1331–1346. https://doi.org/10.1007/s00467-021-04923-1
Acknowledgements
Data in this manuscript were collected by the Chronic Kidney Disease in children prospective cohort study (CKiD) with clinical coordinating centers (Principal Investigators) at Children’s Mercy Hospital and the University of Missouri—Kansas City (Bradley Warady, MD) and Children’s Hospital of Philadelphia (Susan Furth, MD, PhD), Central Biochemistry Laboratory (George Schwartz, MD) at the University of Rochester Medical Center, and data coordinating center (Alvaro Muñoz, PhD and Derek Ng, PhD) at the Johns Hopkins Bloomberg School of Public Health.
Funding
The CKiD Study is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, with additional funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Heart, Lung, and Blood Institute (U01 DK066143, U01 DK066174, U24 DK082194, U24 DK066116). The CKiD website is located at https://statepi.jhsph.edu/ckid and a list of CKiD collaborators can be found at https://statepi.jhsph.edu/ckid/site-investigators/ and in the Supplemental Material.
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Katherine Kurzinski, Yunwen Xu, Derek Ng, and Bradley Warady. The first draft of the manuscript was written by Katherine Kurzinski and Bradley Warady, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics/IRB approval
CKiD protocols and sites were approved by local site Institutional Review Boards (IRBs) and informed consent and assent were provided by all parents and appropriately-aged participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kurzinski, K.L., Xu, Y., Ng, D.K. et al. Hyperkalemia in pediatric chronic kidney disease. Pediatr Nephrol 38, 3083–3090 (2023). https://doi.org/10.1007/s00467-023-05912-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05912-2