Abstract
This review provides updated knowledge on the long-term outcomes among children with antenatally diagnosed urinary tract dilatation (UTD), previously often referred to as antenatal hydronephrosis. Different definitions of UTD exist, which makes comparison between studies and generalized conclusions difficult. Roughly, one-third of antenatally diagnosed UTD, defined as a renal pelvis anterior posterior diameter (APD) of ≥ 4 mm in the second trimester and/or ≥ 7 mm in the third trimester, will resolve before birth, another third will resolve within the first years of life, and in the remaining cases, UTD will persist or a congenital abnormality (CAKUT) will be diagnosed postnatally. The risk of a postnatal CAKUT diagnosis increases with the degree of prenatal and postnatal dilatation, except for vesicoureteral reflux (VUR), which cannot be predicted from the degree of UTD. Urinary tract infections (UTIs) occur in 7–14% of children with UTD during the first years of life. The risk of UTI is higher in children with traditional risk factors for UTI, such as dilated VUR, hydroureteronephrosis, female gender, and intact foreskin. Continuous antibiotic prophylaxis may be considered in selected patients during the first years of life. In long-term follow-ups, permanent kidney damage is diagnosed in approximately 40% of children with moderate or severe UTD, but hypertension, proteinuria, and/or reduced eGFR are uncommon (0–5%). In children with mild UTD, the long-term outcome is excellent, and these children should not be subjected to unnecessary examinations and/or follow-up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Antenatal urinary tract dilatation (UTD) is one of the most common fetal anomalies detected in pregnancy [1,2,3,4,5]. Previously, this condition was referred to as congenital, antenatal, or prenatal hydronephrosis, but UTD is now the preferred term.
The introduction of routine fetal ultrasound screening in the 1990s generated a largely undefined group of patients. As the significance of UTD was unclear, individual centers had to invent their own recommendations, which resulted in numerous suggestions for the definition of significant UTD and many different recommendations for monitoring and management. Knowledge increased over time, and we now know that most dilatations will eventually resolve without intervention; we refer to this as physiological or transient dilatation. However, in some cases, UTD may be the first indication of an underlying urinary tract anomaly. It is therefore necessary to find ways of identifying cases of significant uropathy without exposing children with physiological dilatation to unnecessary investigation and follow-up and without creating unnecessary concern among parents. This is one of the most challenging tasks for the obstetricians, radiologists, and pediatricians involved in the care of these patients.
The aim of this review is to provide updated knowledge on the long-term outcomes and management among children with antenatally diagnosed UTD. The underlying uropathies and their management have been extensively reviewed previously [6,7,8] and will therefore not be addressed here.
Definition and grading of UTD
The aim of screening is to identify a specific condition and then initiate available treatment as early as possible, to avoid the risk of future morbidity. In UTD, this process includes identification of congenital anomalies of the kidney and urinary tract (CAKUT) and/or kidney damage. A prerequisite for successful screening is consensus over the definition of UTD, but it has not yet been possible to establish such a consensus, as cut-offs vary between studies and are often established arbitrarily. Some centers use the same cut-off values for both prenatal and postnatal evaluation, while others use increasing cut-offs for the different trimesters and for the postnatal evaluation.
The most common systems used for grading UTD are the APD system and the Society for Fetal Urology (SFU) system. However, other systems exist, such as the Onen system [9]. In the APD system, the anterior posterior diameter of the kidney pelvis is measured in millimeters. Different threshold values for abnormal dilatation have been used. For example, Dudley et al. proposed a cut-off of ≥ 5 mm throughout pregnancy [1], while Corteville et al. proposed ≥ 4 mm in the second trimester and ≥ 7 mm in the third trimester as definitions of significant pelvis dilation [10].
The SFU system uses a 5-point subjective grading which considers not only the appearance of the kidney pelvis but also the calyces and the kidney parenchyma [11]. However, the exact dimension of the kidney pelvis is not measured. An attempt to describe the SFU system with APD measures has been made by Swords and Peters [12].
A disadvantage of the grading systems mentioned above is that they do not provide information about the appearance of the ureters and bladder and the amount of amniotic fluid. Taking these measures into account is of utmost importance because a dilated bladder, a thickened bladder wall, dilated ureters, and oligohydramnios or anhydramnios may indicate lower urinary tract obstruction.
To address these shortcomings, a consensus conference was organized with the aim of improving the grading of UTD and harmonizing prenatal and postnatal UTD follow-up. Based on accumulated research, a new grading system and follow-up program was proposed [13]. The new system extracted important parts of the different pre-existing grading systems, adjusted limits for significant dilatation, and proposed a reduction in the number of follow-up investigations. Furthermore, it was suggested that the concept of hydronephrosis, which focuses only on the kidney, should be replaced by the concept of UTD, which emphasizes the importance of the entire urinary tract system. UTD is defined as mild, moderate, and severe based on APD measurements and other urinary tract findings (Table 1).
Extensive postnatal investigation was proposed to be limited to those with moderate or severe dilatation. The UTD classification has been evaluated in several studies and has shown an accurate precision in detecting postnatal CAKUT, the need for surgery [14,15,16], and chronic kidney disease [17, 18]. Updated recommendations were published in 2022 [19].
Postnatal evaluation
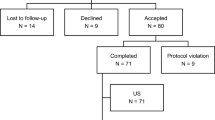
Most protocols recommend that prenatal findings should be confirmed postnatally with two consecutive kidney ultrasounds [20]. Further management is based on the results of these investigations. The first ultrasound examination should, if possible, be postponed to at least 48 h after birth, because of the risk of a false-negative result due to low urine production during the first days of life. The second examination should take place a few weeks or months later, depending on the severity of the antenatal dilatation. A flowchart for both prenatal and postnatal care has been proposed by Nguyen et al. [13]. A similar flowchart used at the Karolinska University Hospital in Stockholm is presented in Fig. 1.
Postnatal investigation with invasive studies such as VCUG and MAG3 scintigraphy is usually reserved for children with postnatal APD ≥ 15 mm and/or abnormal kidney parenchyma, severe calyx dilatation, ureteral dilatation, or bladder pathology [13]. Children with APD 10 to < 15 mm and no other urinary tract abnormalities are usually monitored with repeated ultrasound examinations for some time to rule out progress of the dilatation. However, it has not yet been possible to define either the optimal period between the investigations or the proper time for discontinuation.
What is the risk of a postnatal diagnosis of CAKUT?
Depending on the definition of UTD, CAKUT is diagnosed postnatally in approximately 25–50% of affected children [4, 21,22,23]. The risk increases with increasing degree of the antenatal dilatation [24] for all CAKUT conditions except vesicoureteral reflux (VUR), which is diagnosed in approximately 7–24% of all cases regardless of the degree of antenatal dilatation [4, 21, 22, 24,25,26]. A meta-analysis published in 2006 found that 12% of infants with mild dilatation, 45% with moderate dilatation, and 88% with severe fetal dilatation were postnatally diagnosed with CAKUT [24].
The most common CAKUT conditions diagnosed postnatally are VUR and ureteropelvic junction obstruction (UPJO), both diagnosed in approximately 10–12% of cases, followed by megaureter in 7% and different forms of kidney “plasias” (dysplasia, hypoplasia, and aplasia) in 6% [4, 22]. Conditions such as posterior urethral valve (PUV), prune belly syndrome, neurogenic bladder, ureterocele, and urethral aplasia are less frequently diagnosed. Although rare, it is particularly important to identify cases with possible lower urinary tract obstruction, for instance PUV, as the urinary tract may need decompression soon after birth to prevent further damage to the kidneys.
What is the chance of spontaneous resolution of UTD?
The chance of spontaneous resolution depends on both the definition of UTD and whether all prenatally detected UTD is included or only UTD that persists into the postnatal period. It is important to separate data based on prenatal data from data based on postnatal data, as this knowledge is used to guide health care providers in the optimal surveillance of fetuses and infants with UTD and to provide information to the parents-to-be about what to expect in the future. Resolution in this context is used as a proxy for non-significant UTD, that is, a healthy child.
Knowledge based on prenatal data
Most studies have used prenatal data and analyzed the chance of spontaneous resolution according to whether UTD is mild, moderate, or severe. Unfortunately, as mentioned above, definitions of mild, moderate, and severe UTD vary between studies. For example, Sairam et al. grouped their cohort of 268 fetuses with UTD according to findings in the second trimester; mild if APD was ≥ 4 mm and moderate/severe if APD was ≥ 7 mm or if there was calyceal dilatation. They reported a resolution rate of 82% for mild cases and 44% for moderate and severe cases [3]. Coelho et al. grouped their cohort of 192 fetuses with APD ≥ 5 mm, normal ureters and bladder, and normal amniotic fluid at gestational week 28 or later into mild (5 to < 10 mm), moderate (10 to < 15 mm), and severe (> 15 mm) and reported a resolution rate of 60% for mild UTD, 44% for moderate UTD, and 36% for severe UTD [23]. Barbosa et al. used a definition similar to Coelho et al. and reported a resolution rate of approximately 90% in mild UTD, 74% in moderate UTD, and 27% in severe UTD [25]. In the latter study, the addition of calyx dilatation to mild pelvis dilatation increased the risk of surgery from 9 to 14%; however, the authors did not state the indications for surgery.
Other research groups have concentrated on the subgroup of fetuses with dilated pelvis and/or calyces but normal kidney parenchyma, ureters, urinary bladder, and amount of amniotic fluid, often referred to as “isolated antenatal hydronephrosis.” For example, Tombesi et al. reported that resolution occurred in 73% of cases with isolated antenatal hydronephrosis before or after birth, and only 1% were subjected to surgery postnatally [27].
Mild prenatal UTD, mostly defined as an APD of ≤ 10 mm in the third trimester, often overlaps with the definition of isolated antenatal hydronephrosis. In some cases, however, APD may exceed this threshold without the co-existence of other urinary tract abnormalities, particularly in cases of UPJO. Nevertheless, regardless of the exact definition and grading of UTD, most studies show that a large proportion of antenatally detected UTD will resolve before birth [25,26,27] and a certain proportion more after birth and that the chance of resolution is higher in mild than in severe UTD [25].
Knowledge based on postnatal data
Slightly more than 50% of cases that persist into the postnatal period will eventually resolve, and another 40–45% will improve or stabilize during the first 3 years of life [28,29,30]. Two studies with follow-up of at least 10 years found that resolution had occurred in 73–99% of cases with SFU grade I–II dilatation, 30–89% of cases with SFU III dilatation, and 0–31% of cases with SFU IV dilatation at the end of follow-up [31, 32]. Interestingly, Matsui et al. reported that the UTD reappeared in a small number of patients (1%) after being absent for several years [31].
Even though the chance of resolution in mild and moderate UTD is substantial, there is still a non-negligible risk of surgery in this group. Generally, the need for surgery is low, often reported to be between 0 and 2% [3, 21, 23, 33]. The indication for surgery is mainly VUR with recurrent urinary tract infections (UTIs) or UPJO with increasing dilatation and/or decreasing split function. Higher rates of surgery, such as the 10% reported by Barbosa et al. [25], possibly reflect a different policy for surgery.
What is the risk of urinary tract infections?
Children with antenatally diagnosed UTD have an increased risk of UTI compared to the age-matched normal population. Most studies report a cumulative incidence of approximately 7–14% during the first 3 years of life [21, 23, 27, 28, 33,34,35,36,37,38], but inclusion criteria vary between studies, which makes comparisons difficult. For example, Szymanski et al., Zareba et al., Zee et al., and Visuri et al. excluded children with anatomical abnormalities other than VUR [34,35,36,37]; Tombesi and Alconcher, Madden-Fuentes et al., and Alconcher and Tombesi excluded children with anatomical abnormalities as well as those with VUR [27, 28, 33]; Coelho et al. excluded children with abnormal amniotic fluid and/or bladder or ureter dilatation in utero [23]; and de Kort and Lidefelt did not exclude any cases [21, 38]. Single studies have reported a lower UTI frequency than the abovementioned [39], while for example Braga et al., who unlike most others included patients and collected data prospectively, reported a UTI frequency of 19% [40]. The prospective design may have contributed to the higher cumulative incidence in this study.
Several studies have attempted to define risk factors for UTI within the UTD population. Coelho et al. confirmed that underlying uropathy was an independent risk factor for febrile UTI [41], and in the study by Visuri et al., VUR seemed to be the most important risk factor among the uropathies [37]. Braga et al. concluded that hydroureteronephrosis, female gender, an intact foreskin, and no antibiotic prophylaxis were risk factors for UTI [40]. However, Lidefelt et al. showed that the risk of UTI in children with mild UTD was similar to the age-matched population and therefore did not recommend antibiotic prophylaxis for this group [38]. Moderate/severe UTD (SFU grade III–IV) as opposed to mild UTD (SFU grade I–II) seems to be an independent risk factor only in boys [36].
What is the risk of permanent kidney damage?
Perhaps the most important question in the long term is who will end up with chronic kidney damage later in life and who will not. Children who already exhibit kidney damage at birth, such as those with congenital kidney dysplasia or hypoplasia, naturally belong to this group. However, in an unselected group of children with antenatally detected UTD, it is challenging to predict who else will end up with permanent kidney damage. This question has been addressed by only a few research groups.
The Oliveira group from Brazil is one of these [42]. They analyzed a cohort of 447 children with isolated antenatal APD ≥ 5 mm in the third trimester and showed that 5% of the children had experienced a composite event of hypertension, proteinuria, and/or reduced eGFR at a median follow-up of 6.4 years (IQR: 2.8–12.5 years). All children who experienced this composite event were defined as SFU III–IV, and so, no child with mild UTD developed chronic kidney damage during the study period [42].
Herthelius et al. studied a smaller group of children diagnosed with UTD at a single center in Stockholm between 2003 and 2005 [43]. Approximately two-thirds of the original cohort (71/103, 69%) agreed to a follow-up at an average age of 13.6 years (range: 12–15 years). None of the participants in this study exhibited proteinuria or reduced eGFR at follow-up. However, among children with postnatal APD > 7 mm and/or kidney, calyceal, ureteral, or bladder pathology in the neonatal period, 15% had persistent UTD and 39% had signs of permanent kidney damage (according to either ultrasound or DMSA findings) at the 12–15-year follow-up. Among children without these findings, only one boy (5%) had signs of chronic kidney damage. Among children with chronic kidney damage at the 12–15-year follow-up, all but one (7%) had moderate or severe antenatal UTD (UTD A2–3).
At what time point can follow-up safely be stopped in a child who has dilatation postnatally that is neither a basis for further investigation nor small enough to be ignored?
At the present time we have no definite answer to this question. What we do know is that with today’s recommendations, we will miss sporadic cases with minor urinary tract abnormalities and/or minor kidney damage, for instance VUR. This is unavoidable without exposing a large number of healthy children to unnecessary investigations.
The follow-up of children diagnosed with CAKUT should be individualized and based on recommendations from a pediatric nephrologist, a pediatric urologist, or both. Children older than 1 year and with an APD less than 15 mm and no other abnormal findings on repeated measurements are unlikely to be diagnosed with CAKUT later in life and can be discharged after informing the parents to seek medical advice in case of recurrent UTIs or recurrent or persistent abdominal pain [6, 44].
Summary and conclusions
Roughly speaking, one-third of prenatally detected UTD will resolve before birth, another third will persist into the neonatal period but resolve spontaneously within the first 2 to 3 years of life, and the remaining third will end up with a CAKUT diagnosis in the early neonatal period or with persistent UTD.
In children with CAKUT, chronic kidney damage may be present at birth or may develop later. This group of children should be monitored for kidney damage during childhood.
In children with no CAKUT diagnosis but with persistent moderate or severe UTD (UTD P2–P3, SFU III–IV), there is a small but non-negligible risk of future kidney damage. This group could include cases with undiagnosed CAKUT, mostly VUR or low-grade UPJO, and the optimal follow-up is unclear. It may therefore be wise to infrequently monitor these children during childhood and to carefully instruct the parents to seek medical advice in case of recurrent UTIs or recurrent or persistent abdominal pain.
References
Dudley JA, Haworth JM, McGraw ME, Frank JD, Tizard EJ (1997) Clinical relevance and implications of antenatal hydronephrosis. Arch Dis Child Fetal Neonatal Ed 76:F31–F34. https://doi.org/10.1136/fn.76.1.f31
Feldman DM, DeCambre M, Kong E, Borgida A, Jamil M, McKenna P, Egan JF (2001) Evaluation and follow-up of fetal hydronephrosis. J Ultrasound Med 20:1065–1069. https://doi.org/10.7863/jum.2001.20.10.1065
Sairam S, Al-Habib A, Sasson S, Thilaganathan B (2001) Natural history of fetal hydronephrosis diagnosed on mid-trimester ultrasound. Ultrasound Obstet Gynecol 17:191–196. https://doi.org/10.1046/j.1469-0705.2001.00333.x
Ismaili K, Hall M, Donner C, Thomas D, Vermeylen D, Avni FE, Brussels Free University Perinatal Nephrology study group (2003) Results of systematic screening for minor degrees of fetal renal pelvis dilatation in an unselected population. Am J Obstet Gynecol 188:242–246. https://doi.org/10.1067/mob.2003.81
Lidefelt KJ, Ek S, Mihocsa L (2006) Is screening for vesicoureteral reflux mandatory in infants with antenatal renal pelvis dilatation? Acta Paediatr 95:1653–1656. https://doi.org/10.1080/08035250600764826
Balthazar A, Herndon CDA (2018) Prenatal urinary tract dilatation. Urol Clin North Am 45:641–657. https://doi.org/10.1016/j.ucl.2018.06.011
Becker AM (2009) Postnatal evaluation of infants with an abnormal antenatal renal sonogram. Curr Opin Pediatr 21:207–213. https://doi.org/10.1097/mop.0b013e32832772a8
Chiodini B, Ghassemi M, Khelif K, Ismaili K (2019) Clinical outcome of children with antenatally diagnosed hydronephrosis. Front Pediatr 7:103. https://doi.org/10.3389/fped.2019.00103
Onen A (2007) An alternative grading system to refine the criteria for severity of hydronephrosis and optimal treatment guidelines in neonates with primary UPJ-type hydronephrosis. J Pediatr Urol 3:200–205. https://doi.org/10.1016/j.jpurol.2006.08.002
Corteville JE, Gray DL, Crane JP (1991) Congenital hydronephrosis: correlation of fetal ultrasonographic findings with infant outcome. Am J Obstet Gynecol 165:384–388. https://doi.org/10.1016/0002-9378(91)90099-d
Fernbach SK, Maizels M, Conway JJ (1993) Ultrasound grading of hydronephrosis: introduction to the system used by the Society for Fetal Urology. Pediatr Radiol 23:478–480. https://doi.org/10.1007/BF02012459
Swords KA, Peters CA (2015) Neonatal and early infancy management of prenatally detected hydronephrosis. Arch Dis Child Fetal Neonatal Ed 100:F460–F464. https://doi.org/10.1136/archdischild-2014-306050
Nguyen HT, Benson CB, Bromley B, Campbell JB, Chow J, Coleman B, Cooper C, Crino J, Darge K, Herndon CD, Odibo AO, Somers MJ, Stein DR (2014) Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol 10:982–998. https://doi.org/10.1016/j.jpurol.2014.10.002
Green CA, Adams JC, Goodnight WH, Odibo AO, Bromley B, Jelovsek JE, Stamilio DM, Venkatesh KK (2022) Frequency and prediction of persistent urinary tract dilation in third trimester and postnatal urinary tract dilation in infants following diagnosis in second trimester. Ultrasound Obstet Gynecol 59:522–531. https://doi.org/10.1002/uog.23758
Kaspar CDW, Lo M, Bunchman TE, Xiao N (2017) The antenatal urinary tract dilation classification system accurately predicts severity of kidney and urinary tract abnormalities. J Pediatr Urol 13:485.e1-485.e7. https://doi.org/10.1016/j.jpurol.2017.03.020
Zhang H, Zhang L, Guo N (2020) Validation of “urinary tract dilation” classification system: correlation between fetal hydronephrosis and postnatal urological abnormalities. Medicine (Baltimore) 99:e18707. https://doi.org/10.1097/MD.0000000000018707
Melo FF, Mak RH, Simões E, Silva AC, Vasconcelos MA, Dias CS, Rosa LC, Shiomatsu GY, Storch C, Oliveira MCL, Oliveira EA (2021) Evaluation of urinary tract dilation classification system for prediction of long-term outcomes in isolated antenatal hydronephrosis: a cohort study. J Urol 206:1022–1030. https://doi.org/10.1097/JU.0000000000001899
Melo FF, Vasconcelos MA, Mak RH, Silva ACSE, Dias CS, Colosimo EA, Silva LR, Oliveira MCL, Oliveira EA (2022) Postnatal urinary tract dilatation classification: improvement of the accuracy in predicting kidney injury. Pediatr Nephrol 37:613–623. https://doi.org/10.1007/s00467-021-05254-x
Nguyen HT, Phelps A, Coley B, Darge K, Rhee A, Chow JS (2022) 2021 update on the urinary tract dilation (UTD) classification system: clarifications, review of the literature, and practical suggestions. Pediatr Radiol 52:740–751. https://doi.org/10.1007/s00247-021-05263-w
Aksu N, Yavaşcan O, Kangin M, Kara OD, Aydin Y, Erdoğan H, Tuncel TC, Cetinkaya E, Ozbay E, Sandikçioğlu TG (2005) Postnatal management of infants with antenatally detected hydronephrosis. Pediatr Nephrol 20:1253–1259. https://doi.org/10.1007/s00467-005-1989-3
de Kort EH, Bambang Oetomo S, Zegers SH (2008) The long-term outcome of antenatal hydronephrosis up to 15 millimetres justifies a noninvasive postnatal follow-up. Acta Paediatr 97:708–713. https://doi.org/10.1111/j.1651-2227.2008.00749.x
Mallik M, Watson AR (2008) Antenatally detected urinary tract abnormalities: more detection but less action. Pediatr Nephrol 23:897–904. https://doi.org/10.1007/s00467-008-0746-9
Coelho GM, Bouzada MC, Pereira AK, Figueiredo BF, Leite MR, Oliveira DS, Oliveira EA (2007) Outcome of isolated antenatal hydronephrosis: a prospective cohort study. Pediatr Nephrol 22:1727–1734. https://doi.org/10.1007/s00467-007-0539-6
Lee RS, Cendron M, Kinnamon DD, Nguyen HT (2006) Antenatal hydronephrosis as a predictor of postnatal outcome: a meta-analysis. Pediatrics 118:586–593. https://doi.org/10.1542/peds.2006-0120
Barbosa JA, Chow JS, Benson CB, Yorioka MA, Bull AS, Retik AB, Nguyen HT (2012) Postnatal longitudinal evaluation of children diagnosed with prenatal hydronephrosis: insights in natural history and referral pattern. Prenat Diagn 32:1242–1249. https://doi.org/10.1002/pd.3989
Scarborough PL, Ferrara E, Storm DW (2015) Should prenatal hydronephrosis that resolves before birth be followed postnatally? Analysis and comparison to persistent prenatal hydronephrosis. Pediatr Nephrol 30:1485–1491. https://doi.org/10.1007/s00467-015-3080-z
Tombesi MM, Alconcher LF (2012) Short-term outcome of mild isolated antenatal hydronephrosis conservatively managed. J Pediatr Urol 8:129–133. https://doi.org/10.1016/j.jpurol.2011.06.009
Madden-Fuentes RJ, McNamara ER, Nseyo U, Wiener JS, Routh JC, Ross SS (2014) Resolution rate of isolated low-grade hydronephrosis diagnosed within the first year of life. J Pediatr Urol 10:639–644. https://doi.org/10.1016/j.jpurol.2014.07.004
Sarhan OM, Helaly AE, Al Otay A, Ghanbar MA, Nakshabandi Z (2018) Isolated low grade prenatally detected unilateral hydronephrosis: do we need long term follow-up? Int Braz J Urol 44:812–818. https://doi.org/10.1590/S1677-5538.IBJU.2017.0474
Zee RS, Herndon CDA, Cooper CS, Kim C, McKenna PH, Khoury A, Herbst KW (2017) Time to resolution: a prospective evaluation from the Society for Fetal Urology hydronephrosis registry. J Pediatr Urol 13:316.e1-316.e5. https://doi.org/10.1016/j.jpurol.2016.12.012
Matsui F, Shimada K, Matsumoto F, Takano S (2008) Late recurrence of symptomatic hydronephrosis in patients with prenatally detected hydronephrosis and spontaneous improvement. J Urol 180:322–325. https://doi.org/10.1016/j.juro.2008.03.065
Yang Y, Hou Y, Niu ZB, Wang CL (2010) Long-term follow-up and management of prenatally detected, isolated hydronephrosis. J Pediatr Surg 45:1701–1706. https://doi.org/10.1016/j.jpedsurg.2010.03.030
Alconcher LF, Tombesi MM (2012) Natural history of bilateral mild isolated antenatal hydronephrosis conservatively managed. Pediatr Nephrol 27:1119–1123. https://doi.org/10.1007/s00467-012-2113-0
Szymanski KM, Al-Said AN, Pippi Salle JL, Capolicchio JP (2012) Do infants with mild prenatal hydronephrosis benefit from screening for vesicoureteral reflux? J Urol 188:576–581. https://doi.org/10.1016/j.juro.2012.04.017
Zareba P, Lorenzo AJ, Braga LH (2014) Risk factors for febrile urinary tract infection in infants with prenatal hydronephrosis: comprehensive single center analysis. J Urol 191(5 Suppl):1614–1618. https://doi.org/10.1016/j.juro.2013.10.035
Zee RS, Herbst KW, Kim C, McKenna PH, Bentley T, Cooper CS, Herndon CD (2016) Urinary tract infections in children with prenatal hydronephrosis: a risk assessment from the Society for Fetal Urology hydronephrosis registry. J Pediatr Urol 12:261.e1-261.e2617. https://doi.org/10.1016/j.jpurol.2016.04.024
Visuri S, Jahnukainen T, Taskinen S (2017) Incidence of urinary tract infections in infants with antenatally diagnosed hydronephrosis-a retrospective single center study. J Pediatr Surg 52:1503–1506. https://doi.org/10.1016/j.jpedsurg.2016.11.038
Lidefelt KJ, Herthelius M (2008) Antenatal hydronephrosis: infants with minor postnatal dilatation do not need prophylaxis. Pediatr Nephrol 23:2021–2024. https://doi.org/10.1007/s00467-008-0893-z
Sencan A, Carvas F, Hekimoglu IC, Caf N, Sencan A, Chow J, Nguyen HT (2014) Urinary tract infection and vesicoureteral reflux in children with mild antenatal hydronephrosis. J Pediatr Urol 10:1008–1013. https://doi.org/10.1016/j.jpurol.2014.04.001
Braga LH, Farrokhyar F, D’Cruz J, Pemberton J, Lorenzo AJ (2015) Risk factors for febrile urinary tract infection in children with prenatal hydronephrosis: a prospective study. J Urol 193(5 Suppl):1766–1771. https://doi.org/10.1016/j.juro.2014.10.091
Coelho GM, Bouzada MC, Lemos GS, Pereira AK, Lima BP, Oliveira EA (2008) Risk factors for urinary tract infection in children with prenatal renal pelvic dilatation. J Urol 179:284–289. https://doi.org/10.1016/j.juro.2007.08.159
Costa FP, Simões E, Silva AC, Mak RH, Ix JH, Vasconcelos MA, Dias CS, Fonseca CC, Oliveira MCL, Oliveira EA (2019) A clinical predictive model of renal injury in children with isolated antenatal hydronephrosis. Clin Kidney J 13:834–841. https://doi.org/10.1093/ckj/sfz102
Herthelius M, Axelsson R, Lidefelt KJ (2020) Antenatally detected urinary tract dilatation: a 12–15-year follow-up. Pediatr Nephrol 35:2129–2135. https://doi.org/10.1007/s00467-020-04659-4
Nguyen HT, Herndon CD, Cooper C, Gatti J, Kirsch A, Kokorowski P, Lee R, Perez-Brayfield M, Metcalfe P, Yerkes E, Cendron M, Campbell JB (2010) The Society for Fetal Urology consensus statement on the evaluation and management of antenatal hydronephrosis. J Pediatr Urol 6:212–231. https://doi.org/10.1016/j.jpurol.2010.02.205
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Herthelius, M. Antenatally detected urinary tract dilatation: long-term outcome. Pediatr Nephrol 38, 3221–3227 (2023). https://doi.org/10.1007/s00467-023-05907-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05907-z