Abstract
Background
Neonates with hypoxic ischemic encephalopathy (HIE) receiving therapeutic hypothermia are at high risk of acute kidney injury (AKI).
Methods
We performed a two-site prospective observational study from 2018 to 2019 to evaluate the utility of renal near-infrared spectroscopy (NIRS) in detecting AKI in 38 neonates with HIE receiving therapeutic hypothermia. AKI was defined by a delayed rate of serum creatinine decline (< 33% on day 3 of life, < 40% on day 5, and < 46% on day 7). Renal saturation (Rsat) and systemic oxygen saturation (SpO2) were continuously measured for the first 96 h of life (HOL). Renal fractional tissue oxygen extraction (RFTOE) was calculated as (SpO2 − Rsat)/(SpO2). Using renal NIRS, urine biomarkers, and perinatal factors, logistic regression was performed to develop a model that predicted AKI.
Results
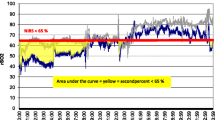
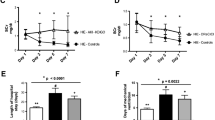
AKI occurred in 20 of 38 neonates (53%). During the first 96 HOL, Rsat was higher, and RFTOE was lower in the AKI group vs. the no AKI group (P < 0.001). Rsat > 70% had a fair predictive performance for AKI at 48–84 HOL (AUC 0.71–0.79). RFTOE ≤ 25 had a good predictive performance for AKI at 42–66 HOL (AUC 0.8–0.83). The final statistical model with the best fit to predict AKI (AUC = 0.88) included RFTOE at 48 HOL (P = 0.012) and pH of the infants’ first postnatal blood gas (P = 0.025).
Conclusions
Lower RFTOE on renal NIRS and pH on infant first blood gas may be early predictors for AKI in neonates with HIE receiving therapeutic hypothermia.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information


Similar content being viewed by others
Abbreviations
- AKI:
-
Acute kidney injury
- DOL:
-
Day of life
- HIE:
-
Hypoxic ischemic encephalopathy
- HOL:
-
Hour of life
- KDIGO:
-
Kidney Disease: Improving Global Outcomes
- MRI:
-
Magnetic resonance imaging
- NICU:
-
Neonatal intensive care units
- NIRS:
-
Near infrared spectroscopy
- R sat :
-
Renal saturation
- RFTOE:
-
Renal fractional tissue oxygen extraction
- SCr:
-
Serum creatinine
References
O’Dea M, Sweetman D, Bonifacio SL, El-Dib M, Austin T, Molloy EJ (2020) Management of multi organ dysfunction in neonatal encephalopathy. Front Pediatr 8:239. https://doi.org/10.3389/fped.2020.00239
Sarafidis K, Tsepkentzi E, Agakidou E, Diamanti E, Taparkou A, Soubasi V, Papachristou F, Drossou V (2012) Serum and urine acute kidney injury biomarkers in asphyxiated neonates. Pediatr Nephrol 27:1575–1582. https://doi.org/10.1007/s00467-012-2162-4
Rumpel J, Spray BJ, Chock VY, Kirkley MJ, Slagle CL, Frymoyer A, Cho SH, Gist KM, Blaszak R, Poindexter B, Courtney SE (2022) Urine biomarkers for the assessment of acute kidney injury in neonates with hypoxic ischemic encephalopathy receiving therapeutic hypothermia. J Pediatr 241:133-140.e3. https://doi.org/10.1016/j.jpeds.2021.08.090
Selewski DT, Jordan BK, Askenazi DJ, Dechert RE, Sarkar S (2013) Acute kidney injury in asphyxiated newborns treated with therapeutic hypothermia. J Pediatr 162:725-729.e1. https://doi.org/10.1016/j.jpeds.2012.10.002
Alaro D, Bashir A, Musoke R, Wanaiana L (2014) Prevalence and outcomes of acute kidney injury in term neonates with perinatal asphyxia. Afr Health Sci 14:682–688. https://www.ajol.info/index.php/ahs/article/view/107254
Oncel MY, Canpolat FE, Arayici S, Alyamac Dizdar E, Uras N, Oguz SS (2016) Urinary markers of acute kidney injury in newborns with perinatal asphyxia. Ren Fail 38:882–888. https://doi.org/10.3109/0886022X.2016.1165070
Sweetman DU, Onwuneme C, Watson WR, O’Neill A, Murphy JF, Molloy EJ (2016) Renal function and novel urinary biomarkers in infants with neonatal encephalopathy. Acta Paediatr 105:e513–e519. https://doi.org/10.1111/apa.13555
Essajee F, Were F, Admani B (2015) Urine neutrophil gelatinase-associated lipocalin in asphyxiated neonates: a prospective cohort study. Pediatr Nephrol 30:1189–1196. https://doi.org/10.1007/s00467-014-3035-9
Altit G, Bhombal S, Tacy TA, Chock VY (2018) End-organ saturation differences in early neonatal transition for left- versus right-sided congenital heart disease. Neonatology 114:53–61. https://doi.org/10.1159/000487472
Sood BG, McLaughlin K, Cortez J (2015) Near-infrared spectroscopy: applications in neonates. Semin Fetal Neonatal Med 20:164–172. https://doi.org/10.1016/j.siny.2015.03.008
Harer MW, Adegboro CO, Richard LJ, McAdams RM (2021) Non-invasive continuous renal tissue oxygenation monitoring to identify preterm neonates at risk for acute kidney injury. Pediatr Nephrol 36:1617–1625. https://doi.org/10.1007/s00467-020-04855-2
Bonsante F, Ramful D, Binquet C, Samperiz S, Daniel S, Gouyon JB, Iacobelli S (2019) Low renal oxygen saturation at near-infrared spectroscopy on the first day of life is associated with developing acute kidney injury in very preterm infants. Neonatology 115:198–204. https://doi.org/10.1159/000494462
Dorum BA, Ozkan H, Cetinkaya M, Koksal N (2021) Regional oxygen saturation and acute kidney injury in premature infants. Pediatr Int 63:290–294. https://doi.org/10.1111/ped.14377
Ruf B, Bonelli V, Balling G, Hörer J, Nagdyman N, Braun SL, Ewert P, Reiter K (2015) Intraoperative renal near-infrared spectroscopy indicates developing acute kidney injury in infants undergoing cardiac surgery with cardiopulmonary bypass: a case-control study. Crit Care 19:27. https://doi.org/10.1186/s13054-015-0760-9
Zhang D, Ouyang C, Zhao X, Cui B, Dai F, Meng L, Ma J (2021) Renal tissue desaturation and acute kidney injury in infant cardiac surgery: a prospective propensity score-matched cohort study. Br J Anaesth 127:620–628. https://doi.org/10.1016/j.bja.2021.06.045
Chock VY, Frymoyer A, Yeh CG, Van Meurs KP (2018) Renal saturation and acute kidney injury in neonates with hypoxic ischemic encephalopathy undergoing therapeutic hypothermia. J Pediatr 200:232-239.e1. https://doi.org/10.1016/j.jpeds.2018.04.076
Sarnat HB, Sarnat MS (1976) Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch Neurol 33:696–705. https://doi.org/10.1001/archneur.1976.00500100030012
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, Fanaroff AA, Poole WK, Wright LL, Higgins RD, Finer NN, Carlo WA, Duara S, Oh W, Cotten CM, Stevenson DK, Stoll BJ, Lemons JA, Guillet R, Jobe AH; National Institute of Child Health and Human Development Neonatal Research Network (2005) Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med 353:1574–1584. https://doi.org/10.1056/NEJMcps050929
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Gupta C, Massaro AN, Ray PE (2016) A new approach to define acute kidney injury in term newborns with hypoxic ischemic encephalopathy. Pediatr Nephrol 31:1167–1178. https://doi.org/10.1007/s00467-016-3317-5
Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, Chishti AS, Woroniecki R, Mammen C, Swanson JR, Sridhar S, Wong CS, Kupferman JC, Griffin RL, Askenazi DJ; Neonatal Kidney Collaborative (NKC) (2017) Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health 1:184–194. https://doi.org/10.1016/S2352-4642(17)30069-X
Zappitelli M, Ambalavanan N, Askenazi DJ, Moxey-Mims MM, Kimmel PL, Star RA, Abitbol CL, Brophy PD, Hidalgo G, Hanna M, Morgan CM, Raju TNK, Ray P, Reyes-Bou Z, Roushdi A, Goldstein SL (2017) Developing a neonatal acute kidney injury research definition: a report from the NIDDK neonatal AKI workshop. Pediatr Res 82:569–573. https://doi.org/10.1038/pr.2017.136
Gist KM, Goldstein SL, Wrona J, Alten JA, Basu RK, Cooper DS, Soranno DE, Duplantis J, Altmann C, Gao Z, Faubel S (2017) Kinetics of the cell cycle arrest biomarkers (TIMP-2*IGFBP-7) for prediction of acute kidney injury in infants after cardiac surgery. Pediatr Nephrol 32:1611–1619. https://doi.org/10.1007/s00467-017-3655-y
Al-Wassia H, Alshaikh B, Sauve R (2013) Prophylactic theophylline for the prevention of severe renal dysfunction in term and post-term neonates with perinatal asphyxia: a systematic review and meta-analysis of randomized controlled trials. J Perinatol 33:271–277. https://doi.org/10.1038/jp.2012.97
Bakr AF (2005) Prophylactic theophylline to prevent renal dysfunction in newborns exposed to perinatal asphyxia–a study in a developing country. Pediatr Nephrol 20:1249–1252. https://doi.org/10.1007/s00467-005-1980-z
Bhatt GC, Gogia P, Bitzan M, Das RR (2019) Theophylline and aminophylline for prevention of acute kidney injury in neonates and children: a systematic review. Arch Dis Child 104:670–679. https://doi.org/10.1136/archdischild-2018-315805
Bhat MA, Shah ZA, Makhdoomi MS, Mufti MH (2006) Theophylline for renal function in term neonates with perinatal asphyxia: a randomized, placebo-controlled trial. J Pediatr 149:180–184. https://doi.org/10.1016/j.jpeds.2006.03.053
Jenik AG, Ceriani Cernadas JM, Gorenstein A, Ramirez JA, Vain N, Armadans M, Ferraris JR (2000) A randomized, double-blind, placebo-controlled trial of the effects of prophylactic theophylline on renal function in term neonates with perinatal asphyxia. Pediatrics 105:E45. https://doi.org/10.1542/peds.105.4.e45
Chock VY, Cho SH, Frymoyer A (2021) Aminophylline for renal protection in neonatal hypoxic-ischemic encephalopathy in the era of therapeutic hypothermia. Pediatr Res 89:974–980. https://doi.org/10.1038/s41390-020-0999-y
Emma F, Montini G, Parikh SM, Salviati L (2016) Mitochondrial dysfunction in inherited renal disease and acute kidney injury. Nat Rev Nephrol 12:267–280. https://doi.org/10.1038/nrneph.2015.214
Massaro AN, Bouyssi-Kobar M, Chang T, Vezina LG, du Plessis AJ, Limperopoulos C (2013) Brain perfusion in encephalopathic newborns after therapeutic hypothermia. AJNR Am J Neuroradiol 34:1649–1655. https://doi.org/10.3174/ajnr.A3422
Perazzo S, Revenis M, Massaro A, Short BL, Ray PE (2020) A new approach to recognize neonatal impaired kidney function. Kidney Int Rep 5:2301–2312. https://doi.org/10.1016/j.ekir.2020.09.043
Cavallin F, Rubin G, Vidal E, Cainelli E, Bonadies L, Suppiej A, Trevisanuto D (2020) Prognostic role of acute kidney injury on long-term outcome in infants with hypoxic-ischemic encephalopathy. Pediatr Nephrol 35:477–483. https://doi.org/10.1007/s00467-019-04406-4
Sarkar S, Askenazi DJ, Jordan BK, Bhagat I, Bapuraj JR, Dechert RE, Selewski DT (2014) Relationship between acute kidney injury and brain MRI findings in asphyxiated newborns after therapeutic hypothermia. Pediatr Res 75:431–435. https://doi.org/10.1038/pr.2013.230
Yan ES, Chock VY, Bonifacio SL, Dahlen A, Guimaraes CV, Altit G, Bhombal S, Van Meurs K (2022) Association between multi-organ dysfunction and adverse outcome in infants with hypoxic ischemic encephalopathy. J Perinatol 42:907–913. https://doi.org/10.1038/s41372-022-01413-6
Kirkley MJ, Boohaker L, Griffin R, Soranno DE, Gien J, Askenazi D, Gist KM; Neonatal Kidney Collaborative (NKC) (2019) Acute kidney injury in neonatal encephalopathy: an evaluation of the AWAKEN database. Pediatr Nephrol 34:169–176. https://doi.org/10.1007/s00467-018-4068-2
Ustun N, Ovali F (2021) Risk factors and outcomes of acute kidney injury in neonates with persistent pulmonary hypertension of the newborn. Medeni Med J 36:193–200. https://doi.org/10.5222/MMJ.2021.22687
Yum SK, Seo YM, Youn YA, Sung IK (2019) Preoperative metabolic acidosis and acute kidney injury after open laparotomy in the neonatal intensive care unit. Pediatr Int 61:994–1000. https://doi.org/10.1111/ped.13929
Charlton JR, Boohaker L, Askenazi D, Brophy PD, D’Angio C, Fuloria M, Gien J, Griffin R, Hingorani S, Ingraham S, Mian A, Ohls RK, Rastogi S, Rhee CJ, Revenis M, Sarkar S, Smith A, Starr M, Kent AL; Neonatal Kidney Collaborative (2019) Incidence and risk factors of early onset neonatal AKI. Clin J Am Soc Nephrol 14:184–195. https://doi.org/10.2215/CJN.03670318
Robertsson Grossmann K, Bárány P, Blennow M, Chromek M (2022) Acute kidney injury in infants with hypothermia-treated hypoxic-ischaemic encephalopathy: an observational population-based study. Acta Paediatr 111:86–92. https://doi.org/10.1111/apa.16078
Meersch M, Schmidt C, Hoffmeier A, Van Aken H, Wempe C, Gerss J, Zarbock A (2017) Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med 43:1551–1561. https://doi.org/10.1007/s00134-016-4670-3
Mintzer JP, Parvez B, Chelala M, Alpan G, LaGamma EF (2014) Quiescent variability of cerebral, renal, and splanchnic regional tissue oxygenation in very low birth weight neonates. J Neonatal Perinatal Med 7:199–206. https://doi.org/10.3233/NPM-14814035
Acknowledgements
The authors would like to thank Donnal Walters, MD, NIRS data analysis, University of Arkansas for Medical Sciences, Little Rock, AR.
Funding
This work was supported by the Arkansas Children’s Research Institute and Arkansas Biosciences Institute. The study sponsors did not have any role in the (1) study design; (2) the collection, analysis, and interpretation of data; (3) the writing of the report; and (4) the decision to submit the manuscript for publication. No form of payment was given to anyone to produce the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Jennifer Rumpel, Beverly J. Spray, Adam Frymoyer, Sydney Rogers, Seo-Ho Cho, Richard Blaszak, Sherry E. Courtney, and Valerie Y. Chock. The first draft of the manuscript was written by Jennifer Rumpel, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The other authors do not have any conflicts of interest to declare for this study. AF is a scientific advisor and holds a financial interest in Halo Biosciences, which is unrelated to the submitted work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
NIRS data from this study were presented in a virtual podium presentation at the Pediatric Academic Society (PAS) meeting in 2021. Urine biomarker data from this cohort were published in the Journal of Pediatrics in a manuscript entitled “Urine Biomarkers for the Assessment of Acute Kidney Injury in Neonates with Hypoxic Ischemic Encephalopathy Receiving Therapeutic Hypothermia” (Rumpel et al. 2022).
Supplementary Information
Below is the link to the electronic supplementary material.
467_2023_5892_MOESM2_ESM.pptx
Supplemental Fig. S1a Receiver operating curve for NIRS renal saturation for prediction of AKI using a delayed rate of SCr decline at 24, 48, and 72 hours of life. 1b. Receiver operating curve for NIRS RFTOE for prediction of AKI using a delayed rate of SCr decline at 24, 48, and 72 hours of life. (PPTX 228 KB)
467_2023_5892_MOESM3_ESM.docx
Supplemental Fig. S2 Receiver operating curve for NIRS RFTOE and infant first blood gas pH for prediction of AKI using a delayed rate of SCr decline at 24, 48, and 72 hours of life. (DOCX 99 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rumpel, J.A., Spray, B.J., Frymoyer, A. et al. Renal oximetry for early acute kidney injury detection in neonates with hypoxic ischemic encephalopathy receiving therapeutic hypothermia. Pediatr Nephrol 38, 2839–2849 (2023). https://doi.org/10.1007/s00467-023-05892-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-023-05892-3