Abstract
Background
Coexisting genetic variants in patients with anti-factor H (FH)-associated atypical hemolytic uremic syndrome (aHUS) have implications for therapy. We estimated the prevalence of complement genetic variants in children with anti-FH aHUS from a prospective nationwide cohort and determined if significant genetic variants impact long-term kidney outcomes.
Methods
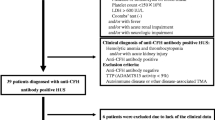
Of 436 patients in the database, 77 consecutive patients, 21 with a relapse and 9 with kidney failure and/or death were included. Targeted sequencing, using a 27-gene panel including CFH, CFI, CFB, C3, CD46, PLG, DGKE, and THBD and multiplex ligation-dependent probe amplification of CFH-CFHR region, was performed. The adverse outcome was eGFR < 30 ml/min/1.73 m2 or death.
Results
Patients had high anti-FH titers 5670 (2177–13,545) AU/ml, relapsing course (42.1%), and adverse outcomes (19.6%). Variants, chiefly of unknown significance, were found in 7 (6.5%; 95% CI 3.1–13.2%); a pathogenic variant was found in one patient. Homozygous deletion of CFHR1 was present in 91.6% compared to 9.8% in 184 healthy controls. Plasma exchanges and immunosuppression showed a trend of improving outcomes, independent of genetic defects (HR 0.32; P = 0.070). Meta-analysis of 18 studies (384 patients) showed that the pooled prevalence of pathogenic and likely pathogenic variants was 3% (95% CI 0–8%). Of 37 total variants in the meta-analysis, 7 (18.9%) each were pathogenic and likely pathogenic; others were variants of unknown significance.
Conclusions
Significant variants in complement regulatory genes are rare in patients with anti-FH-associated aHUS. Irrespective of genetic defects, plasma exchanges and immunosuppression showed a statistical trend to improved outcomes.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
References
Fakhouri F, Zuber J, Fremeaux-Bacchi V, Loirat C (2017) Haemolytic uraemic syndrome. Lancet 390:681–696
Fakhouri F, Fremeaux-Bacchi V (2021) Thrombotic microangiopathy in aHUS and beyond: clinical clues from complement genetics. Nat Rev Nephrol 17:543–553
Vieira-Martins P, El Sissy C, Bordereau P, Gruber A, Rosain J, Fremeaux-Bacchi V (2016) Defining the genetics of thrombotic microangiopathies. Transfus Apher Sci 54:212–219
Schaefer F, Ardissino G, Ariceta G, Fakhouri F, Scully M, Isbel N, Lommele A, Kupelian V, Gasteyger C, Greenbaum LA, Johnson S, Ogawa M, Licht C, Vande Walle J, Fremeaux-Bacchi V, Global aHUS Registry (2018) Clinical and genetic predictors of atypical hemolytic uremic syndrome phenotype and outcome. Kidney Int 94:408–418
Bu F, Zhang Y, Wang K, Borsa NG, Jones MB, Taylor AO, Takanami E, Meyer NC, Frees K, Thomas CP, Nester C, Smith RJH (2018) Genetic analysis of 400 patients refines understanding and implicates a new gene in atypical hemolytic uremic syndrome. J Am Soc Nephrol 29:2809–2819
Challis RC, Ring T, Xu Y, Wong EK, Flossmann O, Roberts IS, Ahmed S, Wetherall M, Salkus G, Brocklebank V, Fester J, Strain L, Wilson V, Wood KM, Marchbank KJ, Santibanez-Koref M, Goodship TH, Kavanagh D (2017) Thrombotic microangiopathy in inverted formin 2-mediated renal disease. J Am Soc Nephrol 28:1084–1091
Osborne AJ, Breno M, Borsa NG, Bu F, Fremeaux-Bacchi V, Gale DP, van den Heuvel LP, Kavanagh D, Noris M, Pinto S, Rallapalli PM, Remuzzi G, Rodriguez de Cordoba S, Ruiz A, Smith RJH, Vieira-Martins P, Volokhina E, Wilson V, Goodship THJ, Perkins SJ (2018) Statistical validation of rare complement variants provides insights into the molecular basis of atypical hemolytic uremic syndrome and C3 glomerulopathy. J Immunol 200:2464–2478
Hofer J, Janecke AR, Zimmerhackl LB, Riedl M, Rosales A, Giner T, Cortina G, Haindl CJ, Petzelberger B, Pawlik M, Jeller V, Vester U, Gadner B, van Husen M, Moritz ML, Wurzner R, Jungraithmayr T; German-Austrian HUS Study Group (2013) Complement factor H-related protein 1 deficiency and factor H antibodies in pediatric patients with atypical hemolytic uremic syndrome. Clin J Am Soc Nephrol 8:407–415
Jozsi M, Licht C, Strobel S, Zipfel SL, Richter H, Heinen S, Zipfel PF, Skerka C (2008) Factor H autoantibodies in atypical hemolytic uremic syndrome correlate with CFHR1/CFHR3 deficiency. Blood 111:1512–1514
Dragon-Durey MA, Sethi SK, Bagga A, Blanc C, Blouin J, Ranchin B, Andre JL, Takagi N, Cheong HI, Hari P, Le Quintrec M, Niaudet P, Loirat C, Fridman WH, Fremeaux-Bacchi V (2010) Clinical features of anti-factor H autoantibody-associated hemolytic uremic syndrome. J Am Soc Nephrol 21:2180–2187
Puraswani M, Khandelwal P, Saini H, Saini S, Gurjar BS, Sinha A, Shende RP, Maiti TK, Singh AK, Kanga U, Ali U, Agarwal I, Anand K, Prasad N, Rajendran P, Sinha R, Vasudevan A, Saxena A, Agarwal S, Hari P, Sahu A, Rath S, Bagga A (2019) Clinical and immunological profile of anti-factor H antibody associated atypical hemolytic uremic syndrome: a nationwide database. Front Immunol 10:1282
Sinha A, Gulati A, Saini S, Blanc C, Gupta A, Gurjar BS, Saini H, Kotresh ST, Ali U, Bhatia D, Ohri A, Kumar M, Agarwal I, Gulati S, Anand K, Vijayakumar M, Sinha R, Sethi S, Salmona M, George A, Bal V, Singh G, Dinda AK, Hari P, Rath S, Dragon-Durey MA, Bagga A; Indian HUS Registry (2014) Prompt plasma exchanges and immunosuppressive treatment improves the outcomes of anti-factor H autoantibody-associated hemolytic uremic syndrome in children. Kidney Int 85:1151–1160
Bhattacharjee A, Reuter S, Trojnar E, Kolodziejczyk R, Seeberger H, Hyvarinen S, Uzonyi B, Szilagyi A, Prohaszka Z, Goldman A, Jozsi M, Jokiranta TS (2015) The major autoantibody epitope on factor H in atypical hemolytic uremic syndrome is structurally different from its homologous site in factor H-related protein 1, supporting a novel model for induction of autoimmunity in this disease. J Biol Chem 290:9500–9510
Zhang Y, Ghiringhelli Borsa N, Shao D, Dopler A, Jones MB, Meyer NC, Pitcher GR, Taylor AO, Nester CM, Schmidt CQ, Smith RJH (2020) Factor H autoantibodies and complement-mediated diseases. Front Immunol 11:607211
Noris M, Caprioli J, Bresin E, Mossali C, Pianetti G, Gamba S, Daina E, Fenili C, Castelletti F, Sorosina A, Piras R, Donadelli R, Maranta R, van der Meer I, Conway EM, Zipfel PF, Goodship TH, Remuzzi G (2010) Relative role of genetic complement abnormalities in sporadic and familial aHUS and their impact on clinical phenotype. Clin J Am Soc Nephrol 5:1844–1859
Valoti E, Alberti M, Iatropoulos P, Piras R, Mele C, Breno M, Cremaschi A, Bresin E, Donadelli R, Alizzi S, Amoroso A, Benigni A, Remuzzi G, Noris M (2019) Rare functional variants in complement genes and anti-FH autoantibodies-associated aHUS. Front Immunol 10:853
Moore I, Strain L, Pappworth I, Kavanagh D, Barlow PN, Herbert AP, Schmidt CQ, Staniforth SJ, Holmes LV, Ward R, Morgan L, Goodship TH, Marchbank KJ (2010) Association of factor H autoantibodies with deletions of CFHR1, CFHR3, CFHR4, and with mutations in CFH, CFI, CD46, and C3 in patients with atypical hemolytic uremic syndrome. Blood 115:379–387
Brocklebank V, Johnson S, Sheerin TP, Marks SD, Gilbert RD, Tyerman K, Kinoshita M, Awan A, Kaur A, Webb N, Hegde S, Finlay E, Fitzpatrick M, Walsh PR, Wong EKS, Booth C, Kerecuk L, Salama AD, Almond M, Inward C, Goodship TH, Sheerin NS, Marchbank KJ, Kavanagh D (2017) Factor H autoantibody is associated with atypical hemolytic uremic syndrome in children in the United Kingdom and Ireland. Kidney Int 92:1261–1271
Kidney Disease Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group (2012) KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Loirat C, Fakhouri F, Ariceta G, Besbas N, Bitzan M, Bjerre A, Coppo R, Emma F, Johnson S, Karpman D, Landau D, Langman CB, Lapeyraque AL, Licht C, Nester C, Pecoraro C, Riedl M, van de Kar NC, Van de Walle J, Vivarelli M, Fremeaux-Bacchi V; HUS International (2016) An international consensus approach to the management of atypical hemolytic uremic syndrome in children. Pediatr Nephrol 31:15–39
Bagga A, Khandelwal P, Mishra K, Thergaonkar R, Vasudevan A, Sharma J, Patnaik SK, Sinha A, Sethi S, Hari P, Dragon-Durey MA on behalf of the Indian Society of Pediatric Nephrology (2019) Hemolytic uremic syndrome in a developing country: consensus guideline. Pediatr Nephrol 34:1465–1482
Krumm N, Turner TN, Baker C, Vives L, Mohajeri K, Witherspoon K, Raja A, Coe BP, Stessman HA, He ZX, Leal SM, Bernier R, Eichler EE (2015) Excess of rare, inherited truncating mutations in autism. Nat Genet 47:582–588
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, Grody WW, Hegde M, Lyon E, Spector E, Voelkerding K, Rehm HL, ACMG Laboratory Quality Assurance Committee (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17:405–424
de Cordoba SR, de Jorge EG (2008) Translational mini-review series on complement factor H: genetics and disease associations of human complement factor H. Clin Exp Immunol 151:1–13
Esparza-Gordillo J, Goicoechea de Jorge E, Buil A, Carreras Berges L, Lopez-Trascasa M, Sanchez-Corral P, Rodriguez de Cordoba S (2005) Predisposition to atypical hemolytic uremic syndrome involves the concurrence of different susceptibility alleles in the regulators of complement activation gene cluster in 1q32. Hum Mol Genet 14:703–712
de Jong S, de Breuk A, Bakker B, Katti S, Hoyng CB, Nilsson SC, Blom AM, van den Heuvel LP, den Hollander AI, Volokhina EB (2021) Functional analysis of variants in complement factor I identified in age-related macular degeneration and atypical hemolytic uremic syndrome. Front Immunol 12:789897
Bienaime F, Dragon-Durey MA, Regnier CH, Nilsson SC, Kwan WH, Blouin J, Jablonski M, Renault N, Rameix-Welti MA, Loirat C, Sautes-Fridman C, Villoutreix BO, Blom AM, Fremeaux-Bacchi V (2010) Mutations in components of complement influence the outcome of factor I-associated atypical hemolytic uremic syndrome. Kidney Int 77:339–349
Nilsson SC, Kalchishkova N, Trouw LA, Fremeaux-Bacchi V, Villoutreix BO, Blom AM (2010) Mutations in complement factor I as found in atypical hemolytic uremic syndrome lead to either altered secretion or altered function of factor I. Eur J Immunol 40:172–185
Fakhouri F, Fila M, Provot F, Delmas Y, Barbet C, Chatelet V, Rafat C, Cailliez M, Hogan J, Servais A, Karras A, Makdassi R, Louillet F, Coindre JP, Rondeau E, Loirat C, Fremeaux-Bacchi V (2017) Pathogenic variants in complement genes and risk of atypical hemolytic uremic syndrome relapse after eculizumab discontinuation. Clin J Am Soc Nephrol 12:50–59
Delvaeye M, Noris M, De Vriese A, Esmon CT, Esmon NL, Ferrell G, Del-Favero J, Plaisance S, Claes B, Lambrechts D, Zoja C, Remuzzi G, Conway EM (2009) Thrombomodulin mutations in atypical hemolytic-uremic syndrome. N Engl J Med 361:345–357
Song D, Liu XR, Chen Z, Xiao HJ, Ding J, Sun SZ, Liu HY, Guo WY, Wang SX, Yu F, Zhao MH, Chinese Renal–TMA Network Institutes, (2017) The clinical and laboratory features of Chinese Han anti-factor H autoantibody-associated hemolytic uremic syndrome. Pediatr Nephrol 32:811–822
Fujisawa M, Kato H, Yoshida Y, Usui T, Takata M, Fujimoto M, Wada H, Uchida Y, Kokame K, Matsumoto M, Fujimura Y, Miyata T, Nangaku M (2018) Clinical characteristics and genetic backgrounds of Japanese patients with atypical hemolytic uremic syndrome. Clin Exp Nephrol 22:1088–1099
Westra D, Volokhina E, van der Heijden E, Vos A, Huigen M, Jansen J, van Kaauwen E, van der Velden T, van de Kar N, van den Heuvel L (2010) Genetic disorders in complement (regulating) genes in patients with atypical haemolytic uraemic syndrome (aHUS). Nephrol Dial Transplant 25:2195–2202
Geerdink LM, Westra D, van Wijk JA, Dorresteijn EM, Lilien MR, Davin JC, Komhoff M, Van Hoeck K, van der Vlugt A, van den Heuvel LP, van de Kar NC (2012) Atypical hemolytic uremic syndrome in children: complement mutations and clinical characteristics. Pediatr Nephrol 27:1283–1291
Fremeaux-Bacchi V, Fakhouri F, Garnier A, Bienaime F, Dragon-Durey MA, Ngo S, Moulin B, Servais A, Provot F, Rostaing L, Burtey S, Niaudet P, Deschenes G, Lebranchu Y, Zuber J, Loirat C (2013) Genetics and outcome of atypical hemolytic uremic syndrome: a nationwide French series comparing children and adults. Clin J Am Soc Nephrol 8:554–562
Lee JM, Park YS, Lee JH, Park SJ, Shin JI, Park YH, Yoo KH, Cho MH, Kim SY, Kim SH, Namgoong MK, Lee SJ, Lee JH, Cho HY, Han KH, Kang HG, Ha IS, Bae JS, Kim NK, Park WY, Cheong HI (2015) Atypical hemolytic uremic syndrome: Korean pediatric series. Pediatr Int 57:431–438
Abarrategui-Garrido C, Martinez-Barricarte R, Lopez-Trascasa M, de Cordoba SR, Sanchez-Corral P (2009) Characterization of complement factor H-related (CFHR) proteins in plasma reveals novel genetic variations of CFHR1 associated with atypical hemolytic uremic syndrome. Blood 114:4261–4271
Bernabeu-Herrero ME, Jimenez-Alcazar M, Anter J, Pinto S, Sanchez Chinchilla D, Garrido S, Lopez-Trascasa M, Rodriguez de Cordoba S, Sanchez-Corral P (2015) Complement factor H, FHR-3 and FHR-1 variants associate in an extended haplotype conferring increased risk of atypical hemolytic uremic syndrome. Mol Immunol 67:276–286
Besbas N, Gulhan B, Soylemezoglu O, Ozcakar ZB, Korkmaz E, Hayran M, Ozaltin F (2017) Turkish pediatric atypical hemolytic uremic syndrome registry: initial analysis of 146 patients. BMC Nephrol 18:6
Stolbova S, Bezdicka M, Prohaszka Z, Csuka D, Hrachovinova I, Burkert J, Simankova N, Pruhova S, Zieg J (2020) Molecular basis and outcomes of atypical haemolytic uraemic syndrome in Czech children. Eur J Pediatr 179:1739–1750
Wu D, Chen J, Ling C, Chen Z, Fan J, Sun Q, Meng Q, Liu X (2021) Clinical and genetic characteristics of atypical hemolytic uremic syndrome in children: a Chinese cohort study. Nephron 145:415–427
Holmes LV, Strain L, Staniforth SJ, Moore I, Marchbank K, Kavanagh D, Goodship JA, Cordell HJ, Goodship TH (2013) Determining the population frequency of the CFHR3/CFHR1 deletion at 1q32. PLoS One 8:e60352
Durey MA, Sinha A, Togarsimalemath SK, Bagga A (2016) Anti-complement-factor H-associated glomerulopathies. Nat Rev Nephrol 12:563–578
Hofer J, Riedl Khursigara M, Perl M, Giner T, Rosales A, Cortina G, Waldegger S, Jungraithmayr T, Wurzner R (2021) Early relapse rate determines further relapse risk: results of a 5-year follow-up study on pediatric CFH-Ab HUS. Pediatr Nephrol 36:917–925
Kar S, Krishnamurthy S, Karunakar P, Maya M, Thangaraj A, Agarwal Y (2021) A rare cause of recurrent acute kidney injury in a 3-year-old girl: answers. Pediatr Nephrol 36:2033–2037
Acknowledgements
We gratefully acknowledge Dr. Marie-Agnes Dragon-Durey (Hopital European Georges Pompidou, France) for helping establish the facility. We thank Dr. David Kavanagh (National Renal Complement Therapeutics Centre, UK) for suggestions to improve the manuscript.
Funding
Funding support by Indo-French Centre for the Promotion of Advanced Research (CEFIPRA) [IFC/A/4703–1/2015/1562; IFC/Network 1/2185]; Department of Biotechnology, Government of India [BT/PR14651/MED/30/566/2010]; Indian Council of Medical Research [Advanced Center for Research in Pediatric Kidney Diseases; 5/7/1090/2013-RHN]; Department of Science and Technology, Government of India [EMR12016/002781]; and the All India Institute of Medical Sciences, New Delhi [A-386].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
467_2022_5862_MOESM2_ESM.pdf
Supplementary file2 Supplementary Figure S1 Flow chart showing variant prioritization. Variants were filtered by focusing on nonsynonymous variants affecting coding region genes. Rare variants have minor allele frequency < 0.1% in 1000 Genome and Genome aggregation database. Predicted pathogenic variants include stop-gain mutations, indels, or missense variants with CADD score > 10 and/or those predicted pathogenic by Polyphen2. Variants below a depth of 40X and allele balance of < 0.3 did not get validated on Sanger, and therefore were excluded on additional hard filtering. The final dataset is comprised of 20 variants in all genes. CADD, Combined Annotation-Dependent Depletion; UTR, untranslated region (PDF 388 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Khandelwal, P., Joshi, A., Mathur, A. et al. Variants in complement genes are uncommon in patients with anti-factor H autoantibody-associated atypical hemolytic uremic syndrome. Pediatr Nephrol 38, 2659–2668 (2023). https://doi.org/10.1007/s00467-022-05862-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05862-1