Abstract
Background
Cardiovascular (CV) complications are important causes of morbidity and mortality in children after kidney transplantation (KTx). In adults, central blood pressure (cBP) is an accepted predictor of CV sequelae. We aimed to assess the prognostic value of cBP over peripheral blood pressure (pBP) for existing CV damage.
Methods
We measured cBP and pBP in 48 pediatric KTx recipients (mean age: 13.5 ± 4.2 years). Assessment of left ventricular mass index (LVMI) and aortic pulse wave velocity (PWV) allowed detection of CV target organ damage. LVMI and PWV were used as endpoints in multivariable linear regression models, in which cBP and pBP were compared for their predictive value.
Results
Using cBP z-scores, we identified a larger number of patients with uncontrolled or untreated hypertension compared to pBP (36% vs. 7%). Central systolic blood pressure (cSBP) was a significant independent predictor of LVMI, while peripheral systolic blood pressure (pSBP) was not. Comparing central (cDBP) and peripheral (pDBP) diastolic blood pressure for their predictive value on PWV revealed a greater estimate for cDBP (0.035 vs. 0.026 for pDBP) along with a slightly better model fit for cDBP.
Conclusions
Our data in a small group of patients provide first evidence that cBP measurements in pediatric KTx recipients might be helpful in identifying patients at risk for the development of CV sequelae. Investigating a larger patient number, ideally repeatedly, is needed to create further evidence supporting our findings. In light of available devices measuring cBP noninvasively, the implementation of such clinical studies post-KTx care should be feasible.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children after kidney transplantation (KTx) suffer from a high cardiovascular (CV) burden and CV events are still among the most important causes of morbidity and mortality in these patients [1, 2]. Early vascular damages resembling athero- and arteriosclerotic processes have been detected by measuring carotid intima-media thickness and aortic pulse wave velocity (PWV) in this high-risk population [3,4,5,6,7]. Similarly, left ventricular hypertrophy (LVH) indicates early cardiac alterations and is frequently detected [3, 8]. These easy-to-measure parameters are well-accepted surrogate markers and have been shown to be highly predictive for future CV events in adult patients [9].
The prevalence of arterial hypertension is high in pediatric KTx recipients [3, 10]. It is not only a major risk factor for CV alterations [4, 11], but also negatively affects graft function [12, 13]. While arterial hypertension is a modifiable risk factor, blood pressure (BP) control in children after KTx remains difficult and needs to be optimized as reported in several recent studies [3, 10, 14, 15]. In addition, relying on peripheral blood pressure (pBP) may not be ideal. Studies in adults showed that central blood pressure (cBP) correlates better with the severity of CV alterations and is a better predictor of CV mortality [16, 17]. In hypertensive children and in children with type 1 diabetes, cBP showed good correlations with PWV [18, 19] and the prevalence of LVH [20]. The implementation of cBP measurements could therefore be helpful to identify high-risk patients. New devices such as the Mobil-O-Graph, which has been validated in children against invasive cBP measurements [21], allow non-invasive and easy-to-perform cBP measurements.
As no data for children after KTx currently exist, we aimed to examine the predictive value of cBP over pBP for existing CV damage detected by measurement of PWV and left ventricular mass index (LVMI) in pediatric KTx recipients. We used the Mobil-O-Graph as it not only has been validated against invasive recordings in children and adults [21, 22], but also because reference data with z-scores is available for children [23].
Methods
Study population
For this prospective study, we examined a total of 48 children, adolescents, and young adults, who received KTx before the age of 18 years. We included only patients with a functioning graft. Patient data (anthropometrics, underlying disease, transplantation history, dialysis prior to transplantation) and current medication information were obtained from the medical charts. Blood samples were obtained and analyzed in a central laboratory (Synlab, Heidelberg, Germany). The analysis included creatinine, cystatin C, and urea. Estimated glomerular filtration rate (eGFR) was calculated as proposed by Schwartz et al. (0.41 × height (cm)/plasma-creatinine (mg/dl)) [24]. Z-scores for height, weight [25], and waist circumference [26] were calculated. Overweight was defined as BMIz ≥ 1.036 (≥ 85th percentile) and < 1.645 (< 95th percentile) of sex-specific z-score range; obesity was defined as BMIz ≥ 1.645 (95th percentile) age and sex-specific z-score [27]. The study protocol was approved by the institutional review board (No. 504–2009) and all parents and children gave informed consent.
Blood pressure
BP measurements were performed as follows: pBP was measured using a validated oscillometric device (Dinamap v100, GE Medical System) after 5 min of rest in a seated position on the right and left arm, one measurement each. pBP z-scores (pBPz) were calculated according to the reference values from the National High Blood Pressure Education Program Working Group in Children and Adolescents [28]. cBP was measured using the Mobil-O-Graph (IEM: GmbH, Stollberg), a validated oscillometric device [21, 22]. Following the instructions of the manufacturer and previous reports [21] cBP was measured after a resting period of at least 5 min in a spinal position. The mean of three consecutive measurements taken on the right arm was used. The device’s software offers two different calibration (C) methods: C1 is based on the measurement of peripheral systolic (pSBP) and diastolic BP (pDBP) with the advantage of existing reference data for central systolic blood pressure (cSBP) values in children aged ≥ 8 years or ≥ 112 cm in girls or ≥ 123 cm in boys, respectively. Values are expressed as z-scores (cSBPz) adjusted for sex and either height or age [23]. C2 is based on the mean arterial BP and the peripheral diastolic BP (DPB) and is considered to provide better accuracy for cBP [29, 30], but offers no reference data. We report cBP based on both calibration methods for this study. We defined pBP values as elevated if the z-score for systolic BP (pSBPz) or diastolic BP (pDBPz) was ≥ 1.645 (95th percentile) [31]. Similarly, cSBP-C1 values with a z-score ≥ 1.645 (95th percentile) were considered elevated. Further classification of elevated BP also considered the use of antihypertensive medication. We defined patients on antihypertensive medication displaying elevated BP values as having “uncontrolled hypertension,” while those with normotensive BP were classified as “controlled hypertension.” Patients who did not receive antihypertensive drugs but displayed elevated BP values were classified as having “untreated hypertension.”
Pulse wave velocity, PWV
PWV was measured using the oscillometric Vicorder device (Skidmore Medical Limited, Bristol, UK; software version 8.3.7244.18754) following a standardized protocol in accordance with the current guidelines [32] as reported previously [33]. The measured velocities were expressed as absolute values and z-scores standardized to height (PWVz) [33].
Echocardiography
Transthoracic echocardiography was performed using a Philips CX 50 ultrasound device (Philips Medical System, Amsterdam, Netherlands), equipped with a 1–5-MHz transducer, according to the recommendations of the American Society of Echocardiography [34]. All studies were evaluated by a single experienced investigator. Wall thickness and dimensions of the left ventricle were measured in the parasternal short axis view at the level of the papillary muscles using M-mode. LVMI was calculated as proposed by Chinali et al. [35]. Children with a LVMI > 45/m2.16 were considered to have LVH.
Methods against bias
pBP and cBP were measured sequentially by a study nurse or a trained medical student. The devices were set to measure BP with mentioned repeats and results were stored in the devices’ data cache until all examinations were performed. Measurements were then transferred to the study’s case report form. Echocardiography was performed and evaluated by a single pediatric cardiologist. PWV was measured by two experienced physicians. None of the physicians was aware of the blood pressure examinations.
Statistical analysis
Data are given as mean ± standard deviation (SD) or frequency and percentage. Paired t-test was used for paired comparison of cBPz and pBPz and paired ANOVA for cBP-C1, cBP-C2, and pBP. Multiple comparisons were corrected with the Tukey adjustment. Multivariable linear regression analyses for LVMI and PWV were performed to investigate the effect of pBP, cBP-C1, and cBP-C2, adjusted for sex, age [10, 33, 36], and eGFR [13, 37, 38]. The goodness of fit, R2, was considered for the comparison of predictive values between cBP-C1, cBP-C2, and pBP on LVMI or PWV. A two-tailed p-value of < 0.05 was considered statistically significant. Statistical analysis was performed using the SAS Enterprise Guide 7.1 (Statistical Analysis Software, Cary, NC, USA).
Results
Patient characteristics
We included 48 pediatric KTx recipients in the study. Mean age was 13.5 ± 4.2 years (range 5–24 years), 22 (46%) were girls, mean height was 151.3 ± 21.2 cm (z-score − 0.4 ± 1.3), and mean BMI was 20.7 ± 4.3 kg/m2 (z-score 0.3 ± 1.0). Congenital anomalies of the kidney and urinary tract (CAKUT) as the underlying disease was found in 32 patients (67%). Mean time since last transplantation was 5.5 ± 4.6 years, 20 patients (42%) were transplanted preemptively, and 4 (8%) received a re-transplantation. Mean eGFR was 76.8 ± 37.5 ml/min/1.73 m2. The majority of patients (n = 44, 92%) received a calcineurin inhibitor–based immunosuppression (cyclosporine A, n = 31; tacrolimus, n = 13) in combination with either mammalian target of rapamycin (mTOR) inhibitors (n = 39, 81%) or mycophenolate mofetil (MMF; n = 8, 17%). Twenty-three (48%) patients were on steroids.
BP measurements
Table 1 provides pBP or cBP assessments as absolute and standardized values.
pBP
Mean pSBP and pDBP were 113.2 ± 10.5 mmHg and 67.0 ± 10.3 mmHg, respectively. Five children (10%) had elevated pSBP, and three children (6%) had elevated pDBP values.
cBP
The Mobil-O-Graph provides C1 and C2 values based on two calibration methods. Mean cSBP-C1 and cDBP-C1 were 107.4 ± 8.8 mmHg and 73.3 ± 9.0 mmHg, while mean cSBP-C2 and cDBP-C2 were 116.5 ± 13.4 mmHg and 72.7 ± 9.1 mmHg. As illustrated in Fig. 1A, cSBP-C2 was significantly higher than cSBP-C1 (p < 0.001); for diastolic absolute values, there was no significant difference as presented in Fig. 1B.
Comparison of central (cBP) and peripheral (pBP) blood pressure. (A) Absolute systolic blood pressure (SBP) values based on two different calibration methods (C1 and C2) for cBP (cSBP-C1 and cSBP-C2) compared to pSBP. (B) Absolute diastolic blood pressure (DBP) values comparing cDBP-C1, cDBP-C2, and pDBP. (C) Z-scores for SBP comparing cSBPz-C1 adjusted for either height or age with pSBPz (adjusted for sex, age, height). Data are presented as absolute values or z-scores, respectively. Bars indicate the mean. The dotted line marks a z-score of 1.645. “*” indicates a significance of p < 0.05; “**” indicates a significance of < 0.001
Comparing cBP and pBP
SBP absolute values for cSBP-C1 were significantly lower than pSBP (p = 0.03), with no difference between cSBP-C2 and pSBP (Fig. 1A). DBP values for either cDBP-C1 or cDBP-C2 were both significantly higher compared to pDPB (p = 0.004 and p = 0.01; Fig. 1B). The two different cSBP-C1 z-scores (cSBPz-C1) adjusted for sex and either height or age were significantly higher than the pSBPz (p < 0.001 and p = 0.03) (Fig. 1C).
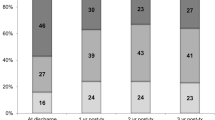
Based on SBP z-scores from pBP and cBP measurements and the use of antihypertensive medication, we aimed to group patients as being normotensive or having untreated, uncontrolled, or controlled hypertension. Based on pSBPz, we identified three (7%) patients having uncontrolled hypertension, 33 (79%) with controlled hypertension, and six (14%) had normotensive pBP values (Fig. 2A). Using cSBPz-C1, we identified 14 (33%) patients with uncontrolled hypertension, 22 (52%) with controlled hypertension, and five (12%) displayed normotensive cSBP-C1 values (Fig. 2B). In addition, one child (3%) was identified with untreated hypertension.
CV damage
As higher BP is known to cause CV damage, we evaluated the effect of pBP and cBP on LVMI and PWV, which we had measured in the majority of patients from our cohort.
LVMI
LVMI values were available for 47 patients. Mean LVMI was 38.3 ± 11.0 g/m2.16. Left ventricular hypertrophy was found in ten (21%) patients. We composed a multivariable linear regression model predicting LVMI and adjusted for sex, age, eGFR, and pSBP (Table 2). While we found a tendency for lower eGFR to affect LVMI, pSBP had no effect on LVMI. To evaluate whether either cSBP-C1 or cSBP-C2 would have predictive value for LVMI, we replaced pSBP in two respective models. While the introduction of cSBP-C1 revealed no significant effect on LVMI, cSBP-C2 showed a significant association with LVMI (estimate for cSBP-C2: 0.326, p = 0.04). In addition, the model including cSBP-C2 showed a superior fit (R2 = 0.182) when compared to the model including either pSBP (R2 = 0.156) or cSBP-C1 (R2 = 0.112).
PWV
PWV values were available for 43 patients. Mean absolute values for PWV were 5.6 ± 0.7 m/s, and the mean PWVz was 1.1 ± 1.1. Sixteen (37%) patients had an elevated PWVz.
Similar to what we had done for LVMI, we composed a multivariable linear regression model predicting PWV adjusted for sex, age, eGFR, and either pSBP or pDPB. We showed that higher pDBP was significantly and independently associated with higher PWV, while pSBP was not. Therefore, we used pDBP for the remaining analysis. Age, but neither sex nor eGFR, was an independent predictor of PWV. Introduction of either cDBP-C1 or cDBP-C2 revealed that both values were independently associated with higher PWV. We found higher estimates for cDBP-C1 and cDBP-C2 (0.033 and 0.035) compared to pDBP (0.026) along with a slightly better model fit for the cDBP-C1 and cDBP-C2 (R2 = 0.462 and R2 = 0.469 vs. R2 = 0.453; Table 2).
Discussion
We evaluated cBP compared to pBP in a cohort of pediatric KTx recipients with a rather high CV burden. We found not only a higher frequency of elevated cSBPz-C1 values when compared to pSBPz, we also found that cBP-C2 was superior over pBP in predicting LVMI and PWV, both important parameters reflecting CV target organ damage. While further investigations with larger patient numbers and longitudinal assessments are surely needed, our data suggest that a larger number of patients than expected has to be considered at risk for CV morbidity and potentially mortality and should be treated preventively. In light of the easy-to-use cBP devices, the implementation of routine cBP measurements into clinical practice to gain more insight into the CV health of pediatric KTx recipients would be feasible.
Our finding that cSBP-C2 was superior in predicting LVMI when compared to pSBP using a multivariable linear regression model extends previous findings, which showed similar associations but were limited to univariate approaches. A possible superiority of cSBP compared to pSBP in predicting LVM has been demonstrated in cohorts of adolescents with untreated hypertension compared to healthy peers [18, 20]. Using the Mobil-O-Graph device, Ntineri et al. demonstrated a higher sensitivity of cSBP-C2 compared to pSBP in predicting LVMI using simultaneous 24-h peripheral and central ambulatory BP monitoring in individuals referred for suspected hypertension and healthy volunteers [20]. Comparable results using the Vicorder device and reference data derived from adults were published by Litwin et al. [18]. While multivariable linear regression models revealed no predictive value of cSBP for LVMI, a ROC analysis showed that cSBP had a greater predictive power for LVH than 24-h ambulatory SBP. Another study in obese children using the Mobil-O-Graph [39] found cBP to be higher in overweight children with and without hypertension. Higher cBP correlated with higher LVMI and PWV, but only in a univariate analysis. A study of 46 adult patients after kidney transplantation showed a significant association between cSBP and LVMI, again only in a univariate approach [40]. The fact that our patient cohort had a considerably high CV burden compared to the other studies discussed here may have allowed us to work out the importance of cSBP in this specific patient group.
We found that in our cohort cDBP-C2 over pDBP could be a better predictor of a higher PWV, which is an important indicator of early vascular damage. Although pDBP and cDBP were both relevant predictors of PWV, we saw a slightly better model fit using cDBP-C2. The few studies addressing this question come up with controversial results. While some studies reported no differences between cBP and pBP in their association with PWV [20, 41], other authors did [17,18,19]. Tagetti et al. [19] showed in a large cohort of children with type 1 diabetes that cSBP and cSBPz were significant predictors of PWV/PWVz in multivariable regression analysis adjusted for age, sex, and different diabetes-specific parameters. This study also demonstrated a superiority of cBP over pBP. In a large cohort of healthy children, Peluso et al. [17] demonstrated a stronger correlation of cBP compared to pBP with vascular alterations such as PWV, but this analysis was only univariate and the predictive value of cDBP over pDBP for higher PWV was not addressed. The study by Litwin et al. [18] also evaluated PWV and found an association of elevated cSBP with higher values for PWV-SDS.
Not only did we show the importance of cBP measurements in predicting CV damage, we also found an unexpected high prevalence of uncontrolled and untreated hypertension using cBP in our cohort of KTx recipients. While the latter could only be determined by using cSBPz-C1 levels, we must assume the results would have been similar if z-scores for cSBP-C2 values were available. Several recent studies reported a high prevalence of uncontrolled or untreated hypertension based on pBP measurements in pediatric patients after KTx [3, 10, 42], but data considering cBP in this particular high-risk group are not available yet. Previous studies used applanation tonometry (SphygmoCor) as an established method for estimating cBP. A comparison of the oscillometric device (Mobil-O-Graph) used in this study with the Sphygmocor revealed no significant differences for the cBP estimation and comparable reproducibility [43]. In light of arterial hypertension being a major but modifiable risk factor associated with CV complications and poor long-term prognosis in children and adolescents after KTx [2, 12, 13], a greater sensitivity in detecting patients with elevated BP in combination with an easy-to-use device will allow us to provide earlier treatment and should consecutively lower patient risk for a poor outcome.
Limitations of our study are the cross-sectional approach and the small sample size. The high prevalence of early CV alterations still enabled us to provide insight into the predictive capacity of cBP and thereby the clinical relevance of these findings in our particular cohort. Further longitudinal assessment within a larger group of patients is required to confirm our results.
Conclusion
While in adults the prognostic value of cBP had been repeatedly reported [16, 17], the predictive power of cBP in context of CV disease in children, especially after KTx, had not been studied. With our data, we provide the first evidence that cBP measurements in pediatric KTx recipients could be helpful in identifying patients at risk for the development of important CV sequelae. Studies investigating a larger number of patients at multiple time points are needed to further support our findings on the predictive capacity of cBP in children. In light of the availability of devices capable of measuring cBP noninvasively and with only minimal training, the implementation of such clinical studies post-KTx care should be feasible.
Data availability
Data available upon reasonable request to the corresponding author.
Code availability
Not applicable.
References
Weaver DJ, Mitsnefes M (2018) Cardiovascular disease in children and adolescents with chronic kidney disease. Semin Nephrol 38:559–569. https://doi.org/10.1016/j.semnephrol.2018.08.002
Foster BJ, Dahhou M, Zhang X, Platt RW, Hanley JA (2011) Change in mortality risk over time in young kidney transplant recipients. Am J Transplant 11:2432–2442. https://doi.org/10.1111/j.1600-6143.2011.03691.x
Borchert-Morlins B, Thurn D, Schmidt BMW, Buscher AK, Oh J, Kier T, Bauer E, Baig S, Kanzelmeyer N, Kemper MJ, Buscher R, Melk A (2017) Factors associated with cardiovascular target organ damage in children after renal transplantation. Pediatr Nephrol 32:2143–2154. https://doi.org/10.1007/s00467-017-3771-8
Sugianto RI, Memaran N, Schmidt BMW, Doyon A, Thurn-Valsassina D, Alpay H, Anarat A, Arbeiter K, Azukaitis K, Bayazit AK, Bulut IK, Caliskan S, Canpolat N, Duzova A, Gellerman J, Harambat J, Homeyer D, Litwin M, Mencarelli F, Obrycki L, Paripovic D, Ranchin B, Shroff R, Tegtbur U, von der Born J, Yilmaz E, Querfeld U, Wuhl E, Schaefer F, Melk A (2022) Findings from 4C-T Study demonstrate an increased cardiovascular burden in girls with end stage kidney disease and kidney transplantation. Kidney Int 101:585–596. https://doi.org/10.1016/j.kint.2021.11.032
Mitsnefes MM, Kimball TR, Witt SA, Glascock BJ, Khoury PR, Daniels SR (2004) Abnormal carotid artery structure and function in children and adolescents with successful renal transplantation. Circulation 110:97–101. https://doi.org/10.1161/01.CIR.0000133412.53089.26
Degi A, Kerti A, Kis E, Cseprekal O, Tory K, Szabo AJ, Reusz GS (2012) Cardiovascular risk assessment in children following kidney transplantation. Pediatr Transplant 16:564–576. https://doi.org/10.1111/j.1399-3046.2012.01730.x
Litwin M, Wuhl E, Jourdan C, Trelewicz J, Niemirska A, Fahr K, Jobs K, Grenda R, Wawer ZT, Rajszys P, Troger J, Mehls O, Schaefer F (2005) Altered morphologic properties of large arteries in children with chronic renal failure and after renal transplantation. J Am Soc Nephrol 16:1494–1500. https://doi.org/10.1681/ASN.2004110932
Hamdani G, Nehus EJ, Hanevold CD, Sebestyen Van Sickle J, Woroniecki R, Wenderfer SE, Hooper DK, Blowey D, Wilson A, Warady BA, Mitsnefes MM (2017) Ambulatory blood pressure, left ventricular hypertrophy, and allograft function in children and young adults after kidney transplantation. Transplantation 101:150–156. https://doi.org/10.1097/TP.0000000000001087
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP (1990) Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 322:1561–1566. https://doi.org/10.1056/NEJM199005313222203
Sugianto RI, Schmidt BMW, Memaran N, Duzova A, Topaloglu R, Seeman T, Konig S, Dello Strologo L, Murer L, Ozcakar ZB, Bald M, Shenoy M, Buescher A, Hoyer PF, Pohl M, Billing H, Oh J, Staude H, Pohl M, Genc G, Klaus G, Alparslan C, Grenda R, Rubik J, Krupka K, Tonshoff B, Wuhl E, Melk A (2020) Sex and age as determinants for high blood pressure in pediatric renal transplant recipients: a longitudinal analysis of the CERTAIN Registry. Pediatr Nephrol 35:415–426. https://doi.org/10.1007/s00467-019-04395-4
Kitzmueller E, Vecsei A, Pichler J, Bohm M, Muller T, Vargha R, Csaicsich D, Aufricht C (2004) Changes of blood pressure and left ventricular mass in pediatric renal transplantation. Pediatr Nephrol 19:1385–1389. https://doi.org/10.1007/s00467-004-1672-0
Stabouli S, Printza N, Dotis J, Gkogka C, Kollios K, Kotsis V, Papachristou F (2016) Long-term changes in blood pressure after pediatric kidney transplantation. Am J Hypertens 29:860–865. https://doi.org/10.1093/ajh/hpv192
Hamdani G, Nehus EJ, Hooper DK, Mitsnefes MM (2016) Masked hypertension and allograft function in pediatric and young adults kidney transplant recipients. Pediatr Transplant 20:1026–1031. https://doi.org/10.1111/petr.12752
Sinha MD, Kerecuk L, Gilg J, Reid CJ (2012) Systemic arterial hypertension in children following renal transplantation: prevalence and risk factors. Nephrol Dial Transplant 27:3359–3368. https://doi.org/10.1093/ndt/gfr804
Seeman T (2012) Ambulatory blood pressure monitoring in pediatric renal transplantation. Curr Hypertens Rep 14:608–618. https://doi.org/10.1007/s11906-012-0301-8
Roman MJ, Devereux RB (2014) Association of central and peripheral blood pressures with intermediate cardiovascular phenotypes. Hypertension 63:1148–1153. https://doi.org/10.1161/HYPERTENSIONAHA.114.03361
Peluso G, Garcia-Espinosa V, Curcio S, Marota M, Castro J, Chiesa P, Giachetto G, Bia D, Zocalo Y (2017) High central aortic rather than brachial blood pressure is associated with carotid wall remodeling and increased arterial stiffness in childhood. High Blood Press Cardiovasc Prev 24:49–60. https://doi.org/10.1007/s40292-017-0179-2
Litwin M, Obrycki L, Niemirska A, Sarnecki J, Kulaga Z (2019) Central systolic blood pressure and central pulse pressure predict left ventricular hypertrophy in hypertensive children. Pediatr Nephrol 34:703–712. https://doi.org/10.1007/s00467-018-4136-7
Tagetti A, Piona CA, Marcon D, Giontella A, Branz L, Bortolotti S, Morandi A, Maffeis C, Fava C (2021) Central systolic blood pressure is associated with early vascular damage in children and adolescents with type 1 diabetes. Front Cardiovasc Med 8:606103. https://doi.org/10.3389/fcvm.2021.606103
Ntineri A, Kollias A, Bountzona I, Servos G, Moyssakis I, Destounis A, Vazeou A, Soldatou A, Stergiou GS (2020) Twenty-four-hour ambulatory central blood pressure in adolescents and young adults: association with peripheral blood pressure and preclinical organ damage. J Hypertens 38:1980–1988. https://doi.org/10.1097/HJH.0000000000002518
Shiraishi M, Murakami T, Higashi K (2020) The accuracy of central blood pressure obtained by oscillometric noninvasive method using Mobil-O-Graph in children and adolescents. J Hypertens 38:813–820. https://doi.org/10.1097/HJH.0000000000002360
Weber T, Wassertheurer S, Rammer M, Maurer E, Hametner B, Mayer CC, Kropf J, Eber B (2011) Validation of a brachial cuff-based method for estimating central systolic blood pressure. Hypertension 58:825–832. https://doi.org/10.1161/HYPERTENSIONAHA.111.176313
Elmenhorst J, Hulpke-Wette M, Barta C, Dalla PR, Springer S, Oberhoffer R (2015) Percentiles for central blood pressure and pulse wave velocity in children and adolescents recorded with an oscillometric device. Atherosclerosis 238:9–16. https://doi.org/10.1016/j.atherosclerosis.2014.11.005
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637. https://doi.org/10.1681/ASN.2008030287
WHO Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl 450:76–85. https://doi.org/10.1111/j.1651-2227.2006.tb02378.x
Sharma AK, Metzger DL, Daymont C, Hadjiyannakis S, Rodd CJ (2015) LMS tables for waist-circumference and waist-height ratio Z-scores in children aged 5–19 y in NHANES III: association with cardio-metabolic risks. Pediatr Res 78:723–729. https://doi.org/10.1038/pr.2015.160
Barlow SE (2007) Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 120(Suppl 4):S164–S192. https://doi.org/10.1542/peds.2007-2329C
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Papaioannou TG, Karageorgopoulou TD, Sergentanis TN, Protogerou AD, Psaltopoulou T, Sharman JE, Weber T, Blacher J, Daskalopoulou SS, Wassertheurer S, Khir AW, Vlachopoulos C, Stergiopulos N, Stefanadis C, Nichols WW, Tousoulis D (2016) Accuracy of commercial devices and methods for noninvasive estimation of aortic systolic blood pressure: a systematic review and meta-analysis of invasive validation studies. J Hypertens 34:1237–1248. https://doi.org/10.1097/HJH.0000000000000921
Sharman JE, Avolio AP, Baulmann J, Benetos A, Blacher J, Blizzard CL, Boutouyrie P, Chen CH, Chowienczyk P, Cockcroft JR, Cruickshank JK, Ferreira I, Ghiadoni L, Hughes A, Jankowski P, Laurent S, McDonnell BJ, McEniery C, Millasseau SC, Papaioannou TG, Parati G, Park JB, Protogerou AD, Roman MJ, Schillaci G, Segers P, Stergiou GS, Tomiyama H, Townsend RR, Van Bortel LM, Wang J, Wassertheurer S, Weber T, Wilkinson IB, Vlachopoulos C (2017) Validation of non-invasive central blood pressure devices: ARTERY Society task force consensus statement on protocol standardization. Eur Heart J 38:2805–2812. https://doi.org/10.1093/eurheartj/ehw632
Lurbe E, Agabiti-Rosei E, Cruickshank JK, Dominiczak A, Erdine S, Hirth A, Invitti C, Litwin M, Mancia G, Pall D, Rascher W, Redon J, Schaefer F, Seeman T, Sinha M, Stabouli S, Webb NJ, Wuhl E, Zanchetti A (2016) 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens 34:1887–1920. https://doi.org/10.1097/HJH.0000000000001039
Van Bortel LM, Duprez D, Starmans-Kool MJ, Safar ME, Giannattasio C, Cockcroft J, Kaiser DR, Thuillez C (2002) Clinical applications of arterial stiffness, Task Force III: recommendations for user procedures. Am J Hypertens 15:445–452. https://doi.org/10.1016/s0895-7061(01)02326-3
Thurn D, Doyon A, Sozeri B, Bayazit AK, Canpolat N, Duzova A, Querfeld U, Schmidt BM, Schaefer F, Wuhl E, Melk A (2015) Aortic pulse wave velocity in healthy children and adolescents: reference values for the vicorder device and modifying factors. Am J Hypertens 28:1480–1488. https://doi.org/10.1093/ajh/hpv048
Lai WW, Geva T, Shirali GS, Frommelt PC, Humes RA, Brook MM, Pignatelli RH, Rychik J (2006) Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J Am Soc Echocardiogr 19:1413–1430. https://doi.org/10.1016/j.echo.2006.09.001
Chinali M, Emma F, Esposito C, Rinelli G, Franceschini A, Doyon A, Raimondi F, Pongiglione G, Schaefer F, Matteucci MC (2016) Left ventricular mass indexing in infants, children, and adolescents: a simplified approach for the identification of left ventricular hypertrophy in clinical practice. J Pediatr 170:193–198. https://doi.org/10.1016/j.jpeds.2015.10.085
Khoury PR, Mitsnefes M, Daniels SR, Kimball TR (2009) Age-specific reference intervals for indexed left ventricular mass in children. J Am Soc Echocardiogr 22:709–714. https://doi.org/10.1016/j.echo.2009.03.003
Kavey RE (2013) Left ventricular hypertrophy in hypertensive children and adolescents: predictors and prevalence. Curr Hypertens Rep 15:453–457. https://doi.org/10.1007/s11906-013-0370-3
Chen SC, Chang JM, Liu WC, Tsai YC, Tsai JC, Hsu PC, Lin TH, Lin MY, Su HM, Hwang SJ, Chen HC (2011) Brachial-ankle pulse wave velocity and rate of renal function decline and mortality in chronic kidney disease. Clin J Am Soc Nephrol 6:724–732. https://doi.org/10.2215/CJN.07700910
Wojtowicz J, Lempicka A, Luczynski W, Szczepanski W, Zomerfeld A, Semeran K, Bossowski A (2017) Central aortic pressure, arterial stiffness and echocardiographic parameters of children with overweight/obesity and arterial hypertension. Adv Clin Exp Med 26:1399–1404. https://doi.org/10.17219/acem/65485
Firat A, Kaya B, Balal M, Paydas S, Akilli R (2019) Relationship between peripheral-central blood pressure and cardiac-renal damage in kidney transplant recipients. Exp Clin Transplant 17:188–194. https://doi.org/10.6002/ect.MESOT2018.P59
Lurbe E, Torro MI, Alvarez-Pitti J, Redon P, Redon J (2016) Central blood pressure and pulse wave amplification across the spectrum of peripheral blood pressure in overweight and obese youth. J Hypertens 34:1389–1395. https://doi.org/10.1097/HJH.0000000000000933
Schaefer F, Doyon A, Azukaitis K, Bayazit A, Canpolat N, Duzova A, Niemirska A, Sozeri B, Thurn D, Anarat A, Ranchin B, Litwin M, Caliskan S, Candan C, Baskin E, Yilmaz E, Mir S, Kirchner M, Sander A, Haffner D, Melk A, Wuhl E, Shroff R, Querfeld U (2017) Cardiovascular phenotypes in children with CKD: the 4C study. Clin J Am Soc Nephrol 12:19–28. https://doi.org/10.2215/CJN.01090216
Weiss W, Gohlisch C, Harsch-Gladisch C, Tölle M, Zidek W, van der Giet M (2012) Oscillometric estimation of central blood pressure: validation of the Mobil-O-Graph in comparison with the SphygmoCor device. Blood Press Monit 17:128–131. https://doi.org/10.1097/MBP.0b013e328353ff63
Funding
Open Access funding enabled and organized by Projekt DEAL. Roche Organ Transplantation Research Foundation, Deutsche Herzstiftung.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the institutional review board (No. 504) and performed according to the Declaration of Helsinki.
Consent to participate
All parents and children gave their written informed consent before participation.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Greiner, AS., von der Born, J., Kohlmeier, L. et al. The significance of central blood pressure for cardiovascular target organ damage in children and adolescents after kidney transplantation. Pediatr Nephrol 38, 2791–2799 (2023). https://doi.org/10.1007/s00467-022-05857-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05857-y