Abstract
Background
Long-term kidney outcomes of non-dialyzed children with Shiga-toxin Escherichia Coli hemolytic uremic syndrome (STEC-HUS) have been scantily studied. Therefore, we aimed to evaluate kidney outcomes and prognostic markers in these patients.
Methods
Non-dialyzed STEC-HUS patients followed for at least 5 years were included. They were grouped and compared according to kidney status at last visit: complete recovery (CR) or chronic kidney disease (CKD). Predictors of CKD evaluated at diagnosis were sex, age, leukocytes, hematocrit, hemoglobin (Hb), and serum creatinine (sCr). Peak sCr and time of follow-up were also analyzed.
Results
A total of 122 patients (62 female, median age at diagnosis 1.6 years) with a median follow-up of 11.3 years were included. At last visit, 82 (67%) had CR, 36 (30%) had CKD stage 1, and 4 (3%) had stage 2. No patient developed CKD stage 3–5. Median time to CKD was 5 years (IQR 3.1–8.76 years). Of the 122 patients, 18% evolved to CKD in the first 5 years, increasing to 28% at 10 and 33% at 20 years of follow-up. Serum Cr at diagnosis and peak sCr were significantly higher in patients with CKD than in those with CR.
Conclusions
One third of non-dialyzed STEC-HUS patients evolved to CKD after a median time of 5 years. However, CKD may appear even after 15 years of CR. Serum Cr was significantly higher among patients who evolved to CKD. These data reinforce that all non-dialyzed patients should be followed until adulthood.
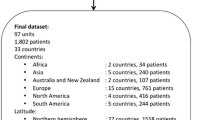
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information



Similar content being viewed by others
References
Siegler RL, Milligan MK, Burningham TH, Christofferson RD, Chang SY, Jorde LB (1991) Long-term outcome and prognostic indicators in the hemolytic-uremic syndrome. J Pediatr 118:195–200. https://doi.org/10.1016/s0022-3476(05)80482-2
Spizzirri FD, Rahman RC, Bibiloni N, Ruscasso JD, Amoreo OR (1997) Childhood hemolytic uremic syndrome in Argentina: long-term follow-up and prognostic features. Pediatr Nephrol 11:156–160. https://doi.org/10.1007/s004670050248
Spinale JM, Ruebner RL, Copelovitch L, Kaplan BS (2013) Long-term outcomes of Shiga toxin hemolytic uremic syndrome. Pediatr Nephrol 28:2097–2105. https://doi.org/10.1007/s00467-012-2383-6
Oakes RS, Kirkham JK, Nelson RD, Siegler RL (2008) Duration of oliguria and anuria as predictors of chronic renal-related sequelae in post-diarrheal hemolytic uremic syndrome. Pediatr Nephrol 23:1303–1308. https://doi.org/10.1007/s00467-008-0799
Cobeñas CJ, Alconcher LF, Spizzirri AP, Rahman RC (2007) Long-term follow-up of Argentinean patients with hemolytic uremic syndrome who had not undergone dialysis. Pediatr Nephrol 22:1343–1347. https://doi.org/10.1007/s00467-007-0522-2
Balestracci A, Meni Battaglia L, Toledo I, Martin SM, Puyol I, Beaudoin L, Robledo NL (2021) Diagnostic sensitivity of extended renal and hematologic criteria to define hemolytic uremic syndrome. Arch Argent Pediatr 119:238–244. https://doi.org/10.5546/aap.2021.eng.238
Coccia P, Ramírez F, Suárez A, Alconcher L, Balestracci A et al (2021) Acute peritoneal dialysis, complications and outcomes in 389 children with STEC-HUS: a multicenter experience. Pediatr Nephrol 36:1597–1606. https://doi.org/10.1007/s00467-020-04876-x
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263. https://doi.org/10.1542/peds.58.2.259
Hogg RJ, Furth S, Lemley KV, Portman R, Schwartz GJ, Coresh J, Balk E, Lau J, Levin A, Kausz AT, Eknoyan G, Levey AS, National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (2003) National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics 111:1416–1421. https://doi.org/10.1542/peds.111.6.1416
Cubillos CMP, Del Salas P, Zambrano PO (2015) Microalbuminuria in pediatric patients diagnosed with hemolytic uremic syndrome. Rev Chil Pediatr 86:92–96. https://doi.org/10.1016/j.rchipe.2015.04.019
Flynn JT, Kaelber DC, Baker-Smith CM, Subcommittee on screening and management of high blood pressure in children et al (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140:e20171904. https://doi.org/10.1542/peds.2017-3035
KDIGO CKD Work Group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150. https://www.kisupplements.org/article/S2157-1716(16)30005-3/fulltext
Pundzienė B, Dobilienė D, Čerkauskienė R, Mitkienė R, Medzevičienė A, Darškuvienė E, Jankauskienė A (2015) Long-term follow-up of children with typical hemolytic uremic syndrome. Medicina 51:146–151. https://doi.org/10.1016/j.medici.2015.06.004
Monet-Didailler C, Godron-Dubrasquet A, Madden I, Delmas Y, Llanas B, Harambat J (2019) Long-term outcome of diarrhea-associated hemolytic uremic syndrome is poorly related to markers of kidney injury at 1-year follow-up in a population-based cohort. Pediatr Nephrol 34:657–662. https://doi.org/10.1007/s00467-018-4131-z
Repetto HA (2005) Long-term course and mechanisms of progression of renal disease in hemolytic uremic syndrome. Kidney Int 97:S102–S106. https://doi.org/10.1111/j.1523-1755.2005.09717.x
Lou-Meda R, Oakes RS, Gilstrap JN, Williams CG, Siegler RL (2007) Prognostic significance of microalbuminuria in postdiarrheal hemolytic uremic syndrome. Pediatr Nephrol 22:117–120. https://doi.org/10.1007/s00467-006-0283-3
Small G, Watson AR, Evans JH, Gallagher J (1999) Hemolytic uremic syndrome: defining the need for long-term follow-up. Clin Nephrol 52:352–356
Van Dyck M, Proesmans W (2004) Renoprotection by ACE inhibitors after severe hemolytic uremic syndrome. Pediatr Nephrol 19:688–690. https://doi.org/10.1007/s00467-004-1451-y
Caletti MG, Missoni M, Vezzani C, Grignoli M, Piantanida JJ, Repetto HA, Exeni R, Rasse SM (2011) Effect of diet, enalapril, or losartan in post-diarrheal hemolytic uremic syndrome nephropathy. Pediatr Nephrol 26:1247–1254. https://doi.org/10.1007/s00467-011-1867-0
Caletti MG, Balestracci A, Missoni M, Vezzani C (2013) Additive antiproteinuric effect of enalapril and losartan in children with hemolytic uremic syndrome. Pediatr Nephrol 28:745–750. https://doi.org/10.1007/s00467-012-2374-7
Ardissino G, Daccò V, Testa S, Civitillo CF, Tel F, Possenti I, Belingheri M, Castorina P, Bolsa-Ghiringhelli N, Tedeschi S, Paglialonga F, Salardi S, Consonni D, Zoia E, Salice P, Chidini G (2015) Hemoconcentration: a major risk factor for neurological involvement in hemolytic uremic syndrome. Pediatr Nephrol 30:345–352. https://doi.org/10.1007/s00467-014-2918-0
Acknowledgements
The authors gratefully acknowledge the assistance of Alejandro Balestracci, MD PhD, in the preparation of this manuscript and María Eugenia Elorza, PhD in Economics, and Fernanda Villarreal, PhD in Economics, for the statistical analysis done at Universidad Nacional del Sur.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This was an observational, retrospective study. The Review Boards and Ethics Committees approved this study. The requirement to obtain informed consent was waived by the institutional review boards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alconcher, L.F., Lucarelli, L.I. & Bronfen, S. Long-term kidney outcomes in non-dialyzed children with Shiga-toxin Escherichia coli associated hemolytic uremic syndrome. Pediatr Nephrol 38, 2131–2136 (2023). https://doi.org/10.1007/s00467-022-05851-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05851-4