Abstract
Background
Understanding which children are at highest risk for high blood pressure (HBP) can inform surveillance and treatment. This study evaluated sex differences in childhood HBP and its associations with socioeconomic status.
Methods
This retrospective cross-sectional study assessed 74,233 children with data from a national primary care electronic medical record database. Differences between sex and material and social deprivation scores for children with and without HBP were examined. Covariates included age, BMI z-score, diabetes, hyperlipidemia, and depression. HBP was defined as > 90th percentile for < 13-year-olds, and ≥ 120/80 for age ≥ 13 years on 2 separate occasions between 2010 and 2017.
Results
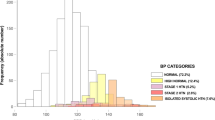
The prevalence of HBP was 10.2% in males and 7.6% in females (p < 0.0001). Children with HBP had higher BMI z-scores (0.66 vs. 0.18, p < 0.0001), and higher rates of diabetes (1.31 vs. 0.54%, p < 0.0001), depression (9.89 vs. 7.11%, p < 0.0001), and hyperlipidemia (2.82 vs. 0.86%, p < 0.0001). In univariate regression analyses, boys in the most materially deprived quintile had increased odds of HBP (OR 1.24 (95% CI 1.08–1.43)), whereas females did not (OR 1.11 (95% CI 0.95–1.29)). In multivariate regression, male sex was associated with HBP with adjusted OR of 1.39 (95% CI 1.24–1.55). After statistical adjustment, material deprivation was no longer significant (aOR 1.05, 95% CI 0.94–1.17).
Conclusions
Male sex is associated with HBP in Canadian children. This study also suggests a possible association between material deprivation and HBP, particularly in boys. Further study is required to better understand this relationship.
Graphical abstract

A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
Abbreviations
- BP:
-
Blood pressure
- HBP:
-
High blood pressure
- CVD:
-
Cardiovascular disease
- SES:
-
Socioeconomic status
- CPCSSN:
-
Canadian Primary Care Sentinel Surveillance Network
- EMR:
-
Electronic medical record
- BMI:
-
Body mass index
- DA:
-
Dissemination area
- ABSM:
-
Area-based socioeconomic measure
- WCH:
-
White-coat hypertension
References
Chen X, Wang Y (2008) Tracking of blood pressure from childhood to adulthood. Circulation 117:3171–3180. https://doi.org/10.1161/CIRCULATIONAHA.107.730366
Cheung EL, Bell CS, Samuel JP, Poffenbarger T, Redwine KM, Samuels JA (2017) Race and obesity in adolescent hypertension. Pediatrics 139:e20161433. https://doi.org/10.1542/peds.2016-1433
Theodore RF, Broadbent J, Nagin D, Ambler A, Hogan S, Ramrakha S, Cutfield W, Williams MJA, Harrington H, Moffitt TE, Caspi A, Milne B, Poulton R (2015) Childhood to early-midlife systolic blood pressure trajectories. Hypertension 66:1108–1115. https://doi.org/10.1161/HYPERTENSIONAHA.115.05831
Miller GE, Chen E, Fok AK, Walker H, Lim A, Nicholls EF, Cole S, Kobor MS et al (2009) Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proc Natl Acad Sci 106:14716–14721. https://doi.org/10.1073/pnas.0902971106
Miller GE, Chen E, Parker KJ (2011) Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving towards a model of behavioral and biological mechanisms. Psychol Bull 137:959–997. https://doi.org/10.1037/a0024768
Jackson SL, Yang EC, Zhang Z (2018) Income disparities and cardiovascular risk factors among adolescents. Pediatrics 142:e20181089. https://doi.org/10.1542/peds.2018-1089
Kivimäki M, Lawlor DA, Smith GD, Keltikangas-Järvinen L, Elovainio M, Vahtera J, Pulkki-Råback L, Taittonen L, Viikari JSA, Raitakari OT (2006) Early socioeconomic position and blood pressure in childhood and adulthood. Hypertension 47:39–44. https://doi.org/10.1161/01.HYP.0000196682.43723.8a
Jimenez MP, Wellenius G, Subramanian SV, Buka S, Eaton C, Gilman SE, Loucks EB (2019) Longitudinal associations of neighborhood socioeconomic status with cardiovascular risk factors: a 46-year follow-up study. Soc Sci Med 241:112574. https://doi.org/10.1016/j.socscimed.2019.112574
Rivera L, Lebenbaum M, Rosella L (2015) The influence of socioeconomic status on future risk for developing type 2 diabetes in the Canadian population between 2011 and 2022: differential associations by sex. Int J Equity Health 14:101. https://doi.org/10.1186/s12939-015-0245-0
Baek TH, Lee HY, Lim NK, Park HY (2015) Gender differences in the association between socioeconomic status and hypertension incidence: the Korean Genome and Epidemiology Study (KoGES). BMC Public Health 15:852. https://doi.org/10.1186/s12889-015-2175-
Thomas AJ, Eberly LE, Smith GD, Neaton JD, Stamler J (2005) Race/Ethnicity, income, major risk factors, and cardiovascular disease mortality. Am J Public Health 95:1417–1423. https://doi.org/10.2105/AJPH.2004.048165
Johnston I, Miles B, Soos B, Garies S, Perez G, Queenan J, Drummond N, Singer A (2022) A cross-sectional study evaluating cardiovascular risk and statin prescribing in the Canadian Primary Care Sentinel Surveillance Network database. BMC Primary Care 23:128. https://doi.org/10.1186/s12875-022-01735-6
Queenan JA, Williamson T, Khan S, Drummond N, Garies S, Morkem R, Birtwhistle R (2016) Representativeness of patients and providers in the Canadian Primary Care Sentinel Surveillance Network: a cross-sectional study. CMAJ Open 4:E28–E32. https://doi.org/10.9778/cmajo.20140128
Kivimäki M, Vahtera J, Tabák AG, Halonen JI, Vineis P, Pentti J, Pahkala K, Rovio S, Viikari J, Kähönen M, Juonala M, Ferrie JE, Stringhini S, Raitakari OT (2018) Neighbourhood socioeconomic disadvantage, risk factors, and diabetes from childhood to middle age in the Young Finns Study: a cohort study. Lancet Public Health 3:e365–e373. https://doi.org/10.1016/S2468-2667(18)30111-7
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM (2017) Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140:e20171904. https://doi.org/10.1542/peds.2017-1904
Pampalon R, Hamel D, Gamache P, Raymond G (2009) A deprivation index for health planning in Canada. Chronic Dis Can 29:178–191. https://doi.org/10.24095/hpcdp.29.4.05
Pampalon R, Hamel D, Gamache P, Philibert M, Raymound G, Simpson A (2012) An area-based material and social deprivation index for public health in Quebec and Canada. Can J Public Health 103(Sup 2):S17–S22. https://doi.org/10.1007/BF03403824
Center for Disease Control and Prevention (2002) 2000 CDC growth charts for the United States: Methods and development. https://www.cdc.gov/nchs/data/series/sr_11/sr11_246.pdf. Accessed 22 September 2022.
Williamson T, Green ME, Birtwhistle R, Khan S, Garies S, Wong S, Natarajan N, Manca D, Drummond N (2014) Validating the 8 CPCSSN case definitions for chronic disease surveillance in a primary care database of electronic health records. Ann Fam Med 12:367–372. https://doi.org/10.1370/afm.1644
Kosowan L, Wicklow B, Queenan J, Yeung R, Amed S, Singer A (2019) Enhancing health surveillance: validation of a novel electronic medical records-based definition of cases of pediatric type 1 and type 2 diabetes mellitus. Can J Diabetes 43:392–398. https://doi.org/10.1016/j.jcjd.2019.02.005
Ding L, Singer A, Kosowan L, Dart A (2022) Pediatric hypertension screening and recognition in primary care clinics in Canada. Paediatr Child Health 27:118–126. https://doi.org/10.1093/pch/pxab081
Sharma AK, Metzger DL (2017) Calculator: AAP 2017 pediatric blood pressure percentiles. https://apps.cpeg-gcep.net/BPz_cpeg_dde/ Accessed 12 January 2021
Mills KT, Stefanescu A, He J (2020) The global epidemiology of hypertension. Nat Rev Nephrol 16:223–237. https://doi.org/10.1038/s41581-019-0244-2
Fallah Z, Kelishadi R, Heshmat R, Motlagh ME, Ardalan G, Kasaeian A, Asayesh H, Qorbani M (2015) A nationwide report on blood pressure of children and adolescents according to socioeconomic status: the CASPIAN-IV study. J Res Med Sci 20:646–655. https://doi.org/10.4103/1735-1995.166210
Dekkers JC, Snieder H, van den Oord EJCG, Treiber FA (2002) Moderators of blood pressure development from childhood to adulthood: a 10-year longitudinal study. J Pediatr 141:770–779. https://doi.org/10.1067/mpd.2002.128113
Matheson FI, White HL, Moineddin R, Dunn JR, Glazier RH (2010) Neighbourhood chronic stress and gender inequalities in hypertension among Canadian adults: a multilevel analysis. J Epidemiol Community Health 64:705–713. https://doi.org/10.1136/jech.2008.083303
Neufcourt L, Deguen S, Bayat S, Zins M, Grimaud O (2020) Gender differences in the association between socioeconomic status and hypertension in France: a cross-sectional analysis of the CONSTANCES cohort. PLoS One 15:e0231878. https://doi.org/10.1371/journal.pone.0231878
Kaelber DC, Localio AR, Ross M, Leon JB, Pace WD, Wasserman RC, Grundmeier RW, Steffes J, Fiks AG (2020) Persistent hypertension in children and adolescents: a 6-year cohort study. Pediatrics 146:e20193778. https://doi.org/10.1542/peds.2019-3778
US Preventive Services Task Force, Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, Donahue K, Doubeni CA, Epling JWJ, Kubik M, Ogedegbe G, Pbert L, Silverstein M, Simon MA, Tseng CW, Wong JB (2020) Screening for high blood pressure in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA 324:1878–1883. https://doi.org/10.1001/jama.2020.20122
Funding
This work was funded by the Children’s Hospital Research Institute of Manitoba (CHRIM) as a catalyst grant from the Diabetes Research Institute of Manitoba (DREAM) Research Theme.
Author information
Authors and Affiliations
Contributions
S. Telencoe conceptualized and designed the study, preformed initial data analysis, created the first draft and revised the final copy of the manuscript. L. Kosowan conducted the statistical analysis and provided revisions for the final manuscript. A. Singer provided consultative support for the database and provided revisions for the final manuscript. A. Dart conceptualized and designed the study, supervised, and revised the entirety of the study. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Telencoe, S., Singer, A., Kosowan, L. et al. An analysis of sex differences and socioeconomic deprivation among Canadian children with high blood pressure: a retrospective, cross-sectional study. Pediatr Nephrol 38, 2137–2145 (2023). https://doi.org/10.1007/s00467-022-05841-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05841-6