Abstract
Background
FGF23 mediates cardiac fibrosis through the activation of pro-fibrotic factors in in vitro models and is markedly elevated in kidney disease. Left atrial global longitudinal strain (LA GLS) derived by echocardiographic speckle-tracking measures longitudinal shortening of the LA walls, quantifies atrial performance and may enable detection of early LA remodeling in the setting of normal ventricular function. We hypothesized that LA GLS is abnormal in children on hemodialysis (HD) compared to healthy controls of comparable age/sex distribution and that, among HD patients, greater FGF23 levels are associated with abnormal LA GLS.
Methods
Clinical and echocardiographic data from 29 children receiving HD and 13 healthy controls were collected in a cross-sectional single-center study. Plasma FGF23 concentrations were measured using ELISA. The primary outcome was LA GLS measured using 2D speckle-tracking strain analysis. Linear regression analysis was used to investigate predictors of LA GLS in HD.
Results
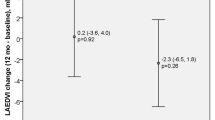
Median dialysis vintage was 1.5 (IQR 0.5–4.3) years. Median intact FGF23 levels were substantially higher in the HD vs. control group (1206 [215, 4707] vs. 51 [43, 66.5] pg/ml; P = 0.0001), and LA GLS was 39.9% SD 11.6 vs. 32.8% SD 5.7 (P = 0.04). Among HD patients, higher FGF23 was associated with lower LA GLS (β per unit Ln-FGF23: − 2.7; 95% CI slope − 5.4, − 0.1; P = 0.04 after adjustment for age, body size, and HD vintage. FGF23 was not associated with LA phasic reservoir, conduit, or contractile strain.
Conclusions
In children on HD and preserved left ventricular ejection fraction, greater FGF23 is associated with lower LA GLS (indicative of impaired atrial performance).
Graphical Abstract

A higher resolution version of the Graphical abstract is available as Supplementary information


Similar content being viewed by others
References
Portale AA, Wolf M, Juppner H, Messinger S et al (2014) Disordered FGF23 and mineral metabolism in children with CKD. Clin J Am Soc Nephrol 9:344–353. https://doi.org/10.2215/CJN.05840513
Isakova T, Wahl P, Vargas GS, Gutiérrez OM et al (2011) Fibroblast growth factor 23 is elevated before parathyroid hormone and phosphate in chronic kidney disease. Kidney Int 79:1370–1378. https://doi.org/10.1038/ki.2011.47
Pereira RC, Juppner H, Azucena-Serrano CE, Yadin O et al (2009) Patterns of FGF-23, DMP1, and MEPE expression in patients with chronic kidney disease. Bone 45:1161–1168. https://doi.org/10.1016/j.bone.2009.08.008
Wolf M (2012) Update on fibroblast growth factor 23 in chronic kidney disease. Kidney Int 82:737–747. https://doi.org/10.1038/ki.2012.176
Isakova T, Xie H, Barchi-Chung A, Vargas G et al (2011) Fibroblast growth factor 23 in patients undergoing peritoneal dialysis. Clin J Am Soc Nephrol 6:2688–2695. https://doi.org/10.2215/CJN.04290511
Viaene L, Bammens B, Meijers BK, Vanrenterghem Y et al (2012) Residual renal function is an independent determinant of serum FGF-23 levels in dialysis patients. Nephrol Dial Transplant 27:2017–2022. https://doi.org/10.1093/ndt/gfr596
Zaritsky J, Rastogi A, Fischmann G, Yan J, Kleinman K et al (2014) Short daily hemodialysis is associated with lower plasma FGF23 levels when compared with conventional hemodialysis. Nephrol Dial Transplant 29:437–441. https://doi.org/10.1093/ndt/gft382
Carlson N, Mortensen OH, Axelsen M, Pedersen RS et al (2017) Clearance of sclerostin, osteocalcin, fibroblast growth factor 23, and osteoprotegerin by dialysis. Blood Purif 44:122–128. https://doi.org/10.1159/000465513
Gutierrez OM, Mannstadt M, Isakova T, Rauh-Hain JA et al (2008) Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis. N Engl J Med 359:584–592. https://doi.org/10.1056/NEJMoa0706130
Ix JH, Katz R, Kestenbaum BR, de Boer IH et al (2012) Fibroblast growth factor-23 and death, heart failure, and cardiovascular events in community-living individuals: CHS (cardiovascular health study). J Am Coll Cardiol 60:200–207. https://doi.org/10.1016/j.jacc.2012.03.040
Mitsnefes MM, Betoko A, Schneider MF, Salusky IB et al (2018) FGF23 and left ventricular hypertrophy in children with CKD. Clin J Am Soc Nephrol 13:45–52. https://doi.org/10.2215/CJN.02110217
Grabner A, Amaral AP, Schramm K, Singh S et al (2015) Activation of cardiac fibroblast growth factor receptor 4 causes left ventricular hypertrophy. Cell Metab 22:1020–1032. https://doi.org/10.1016/j.cmet.2015.09.002
Hao H, Li X, Li Q, Hairuo L et al (2016) FGF23 promotes myocardial fibrosis in mice through activation of beta-catenin. Oncotarget 7:64649–64664. https://doi.org/10.18632/oncotarget.11623
Nattel S, Harada M (2014) Atrial remodeling and atrial fibrillation: recent advances and translational perspectives. J Am Coll Cardiol 63:2335–2345. https://doi.org/10.1016/j.jacc.2014.02.555
Thomas L, Abhayaratna WP (2017) Left atrial reverse remodeling: mechanisms, evaluation, and clinical significance. JACC Cardiovasc Imaging 10:65–77. https://doi.org/10.1016/j.jcmg.2016.11.003
Chavers BM, Li S, Collins AJ, Herzog CA (2002) Cardiovascular disease in pediatric chronic dialysis patients. Kidney Int 62:648–653. https://doi.org/10.1046/j.1523-1755.2002.00472.x
Mathews TJ, Minino AM, Osterman MJ, Strobino DM, Guyer B (2011) Annual summary of vital statistics: 2008. Pediatrics 127:146–157. https://doi.org/10.1542/peds.2010-3175
van Huis M, Schoenmaker NJ, Groothoff JW, van der Lee JH et al (2016) Impaired longitudinal deformation measured by speckle-tracking echocardiography in children with end-stage renal disease. Pediatr Nephrol 31:1499–1508. https://doi.org/10.1007/s00467-016-3362-0
Gheissari A, Dehghan B, Ghaed Sharafi B, Abedini A et al (2019) Importance of mean platelet volume in predicting cardiac mechanics parameters and carotid-intima media thickness in children with end-stage renal disease and comparison with healthy children. Ther Apher Dial 23:451–459. https://doi.org/10.1111/1744-9987.12794
Thomas L, Muraru D, Popescu BA, Sitges M et al (2020) Evaluation of left atrial size and function: relevance for clinical practice. J Am Soc Echocardiogr 33:934–952. https://doi.org/10.1016/j.echo.2020.03.021
Yuda S, Muranaka A, Miura T (2016) Clinical implications of left atrial function assessed by speckle tracking echocardiography. J Echocardiogr 14:104–112. https://doi.org/10.1007/s12574-016-0283-7
Boyd AC, Richards DA, Marwick T, Thomas L (2011) Atrial strain rate is a sensitive measure of alterations in atrial phasic function in healthy ageing. Heart 97:1513–1519. https://doi.org/10.1136/heartjnl-2011-300134
Morris DA, Takeuchi M, Krisper M, Köhncke C et al (2015) Normal values and clinical relevance of left atrial myocardial function analysed by speckle-tracking echocardiography: multicentre study. Eur Heart J Cardiovasc Imaging 16:364–372. https://doi.org/10.1093/ehjci/jeu219
Li S, Zhou K, Du H, Shen C, Li Y, Che G (2017) Body surface area is a novel predictor for surgical complications following video-assisted thoracoscopic surgery for lung adenocarcinoma: a retrospective cohort study. BMC Surg 17:69. https://doi.org/10.1186/s12893-017-0264-4
Jovanovich A, You Z, Isakova T, Nowak K et al (2019) Fibroblast growth factor 23 trajectories in chronic hemodialysis patients: lessons from the HEMO study. Am J Nephrol 49:263–270. https://doi.org/10.1159/000497445
Bouma-de Krijger A, de Roij van Zuijdewijn CLM, Nubé MJ, Grooteman MPC et al, CONTRAST Study Group (2020) Change in FGF23 concentration over time and its association with all-cause mortality in patients treated with haemodialysis or haemodiafiltration. Clin Kidney J 14:891-897. https://doi.org/10.1093/ckj/sfaa028
Marino PN (2021) Left atrial conduit function: a short review. Physiol Rep 9:e15053. https://doi.org/10.14814/phy2.15053
Abhayaratna WP, Seward JB, Appleton CP, Douglas PS et al (2006) Left atrial size: physiologic determinants and clinical applications. J Am Coll Cardiol 47:2357–2363. https://doi.org/10.1016/j.jacc.2006.02.048
Bisbal F, Baranchuk A, Braunwald E, Bayes de Luna A, Bayes-Genis A (2020) Atrial failure as a clinical entity: JACC review topic of the week. J Am Coll Cardiol 75:222–232. https://doi.org/10.1016/j.jacc.2019.11.013
Meisel K, Yuan K, Fang Q, Bibby D, Lee R, Schiller NB (2019) Embolic stroke of undetermined source: a population with left atrial dysfunction. J Stroke Cerebrovasc Dis 28:1891–1896. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.04.004
Melenovsky V, Borlaug BA, Rosen B, Hat I et al (2007) Cardiovascular features of heart failure with preserved ejection fraction versus nonfailing hypertensive left ventricular hypertrophy in the urban Baltimore community: the role of atrial remodeling/dysfunction. J Am Coll Cardiol 49:198–207. https://doi.org/10.1016/j.jacc.2006.08.050
Santos AB, Kraigher-Krainer E, Gupta DK, Claggett B et al (2014) Impaired left atrial function in heart failure with preserved ejection fraction. Eur J Heart Fail 16:1096–1103. https://doi.org/10.1002/ejhf.147
Boixel C, Fontaine V, Rucker-Martin C, Milliez P et al (2003) Fibrosis of the left atria during progression of heart failure is associated with increased matrix metalloproteinases in the rat. J Am Coll Cardiol 42:336–344. https://doi.org/10.1016/s0735-1097(03)00578-3
Dolgilevich SM, Siri FM, Atlas SA, Eng C (2001) Changes in collagenase and collagen gene expression after induction of aortocaval fistula in rats. Am J Physiol Heart Circ Physiol 281:H207-214. https://doi.org/10.1152/ajpheart.2001.281.1.H207
Shen MJ, Arora R, Jalife J (2019) Atrial myopathy. JACC Basic Transl Sci 4:640–654. https://doi.org/10.1016/j.jacbts.2019.05.005
Altekin RE, Yanikoglu A, Karakas MS, Ozel D, Yilmaz H, Demir I (2013) Evaluation of left atrial function using two-dimensional speckle tracking echocardiography in end-stage renal disease patients with preserved left ventricular ejection fraction. Kardiol Pol 71:341–351. https://doi.org/10.5603/KP.2013.0061
Calleja AM, Rakowski H, Williams LK, Jamorski M, Chan CT, Carasso S (2016) Left atrial and ventricular systolic and diastolic myocardial mechanics in patients with end-stage renal disease. Echocardiography 33:1495–1503. https://doi.org/10.1111/echo.13284
Hassanin N, Alkemary A (2016) Detection of left atrium myopathy using two-dimensional speckle tracking echocardiography in patients with end-stage renal disease on dialysis therapy. Echocardiography 33:233–241. https://doi.org/10.1111/echo.13101
Li C, Zhang J, Fan R, Wei Li et al (2019) Left atrial strain associated with alterations in cardiac diastolic function in patients with end-stage renal disease. Int J Cardiovasc Imaging 35:1803–1810. https://doi.org/10.1007/s10554-019-01622-9
Abid L, Charfeddine S, Kammoun S (2016) Relationship of left atrial global peak systolic strain with left ventricular diastolic dysfunction and brain natriuretic peptide level in end-stage renal disease patients with preserved left ventricular ejection fraction. J Echocardiogr 14:71–78. https://doi.org/10.1007/s12574-016-0276-6
Park CS, Kim YK, Song HC, Choi EJ et al (2012) Effect of preload on left atrial function: evaluated by tissue Doppler and strain imaging. Eur Heart J Cardiovasc Imaging 13:938–947. https://doi.org/10.1093/ehjci/jes069
Doan TT, Srivaths P, Liu A, Wilkes JK et al (2021) Left ventricular strain and left atrial strain are impaired during hemodialysis in children. Int J Cardiovasc Imaging 37:3489–3497. https://doi.org/10.1007/s10554-021-02350-9
Leifheit-Nestler M, Kirchhoff F, Nespor J, Richter B et al (2018) Fibroblast growth factor 23 is induced by an activated renin-angiotensin-aldosterone system in cardiac myocytes and promotes the pro-fibrotic crosstalk between cardiac myocytes and fibroblasts. Nephrol Dial Transplant 33:1722–1734. https://doi.org/10.1093/ndt/gfy006
Touchberry CD, Green TM, Tchikrizov V, Mannix JE et al (2013) FGF23 is a novel regulator of intracellular calcium and cardiac contractility in addition to cardiac hypertrophy. Am J Physiol Endocrinol Metab 304:E863-873. https://doi.org/10.1152/ajpendo.00596.2012
Patel RB, Ning H, de Boer IH, Kestenbaum B et al (2020) Fibroblast growth factor 23 and long-term cardiac function: the multi-ethnic study of atherosclerosis. Circ Cardiovasc Imaging 13:e011925. https://doi.org/10.1161/CIRCIMAGING.120.011925
Funding
VA IK2-CX002195 (SS), NIDDK K24DK110427 (JHI), VA-MERIT I01-CX001901 (KLN), NHLBI R01HL148182 (KLN), and NIDDK U2CDK129496 (IBS).
Author information
Authors and Affiliations
Contributions
Research idea and study design: SS, JHI, IBS, and KLN; data acquisition: IBS, MRH, NRP, SS, and KLN; data analysis/interpretation: NRP, JHI, SS, and KLN; statistical analysis: SS and NRP; supervision or mentorship: IBS, JHI, and KLN. Each author contributed important intellectual content during manuscript drafting or revision and agreed to be personally accountable for the individual’s own contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved, including with documentation in the literature if appropriate.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Ix is the principal investigator of an investigator-initiated research grant from Baxter International, serves as a data safety monitoring board member for Sanifit International, and has served on advisory boards for Alpha Young, AstraZeneca, Ardelyx Inc., and Jnana Inc. Dr. Salusky has served on advisory boards for Akebia, Inozyme, and Ardelyx. The remaining authors have declared no relevant conflicts of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sharma, S., Patel, N.R., Hanudel, M.R. et al. Plasma FGF23 is associated with left atrial remodeling in children on hemodialysis. Pediatr Nephrol 38, 2179–2187 (2023). https://doi.org/10.1007/s00467-022-05812-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05812-x