Abstract
Pediatric patients on kidney replacement therapy (KRT) are among the most vulnerable during large-scale disasters, either natural or man-made. Hemodialysis (HD) treatments may be impossible because of structural damage and/or shortage of medical supplies, clean water, electricity, and healthcare professionals. Lack of peritoneal dialysis (PD) solutions and increased risk of infectious/non-infectious complications may make PD therapy challenging. Non-availability of immunosuppressants and increased risk of infections may result in graft loss and deaths of kidney transplant recipients. Measures to mitigate these risks must be considered before, during, and after the disaster including training of staff and patients/caregivers to cope with medical and logistic problems. Soon after a disaster, if the possibility of performing HD or PD is uncertain, patients should be directed to other centers, or the duration and/or number of HD sessions or the PD prescription adapted. In kidney transplant recipients, switching among immunosuppressants should be considered in case of non-availability of the medications. Post-disaster interventions target treating neglected physical and mental problems and also improving social challenges. All problems experienced by pediatric KRT patients living in the affected area are applicable to displaced patients who may also face extra risks during their travel and also at their destination. The need for additional local, national, and international help and support of non-governmental organizations must be anticipated and sought in a timely manner.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization Department of Emergency and Humanitarian Action (WHO/EHA) defines a disaster as “an occurrence, disrupting the normal conditions of existence and causing a level of suffering that exceeds the capacity of adjustment of the affected community” [1]. Disasters involve three components occurring simultaneously: (i) a hazard, (ii) a vulnerable population, and (iii) an inadequate capacity to cope with the potential adverse effects [2].
According to the triggering hazard, disasters may be natural or man-made. Natural disasters result from sudden, large-scale events caused by nature, which cannot be prevented or controlled. Earthquakes, hurricanes, tsunamis, and floods are some examples. Biological hazards, including epidemics and pandemics, also form a subgroup of natural disasters. On the other hand, all kinds of armed conflicts (wars, terrorist attacks, and religious conflicts), nuclear accidents, and structural collapses are examples of man-made disasters. Irrespective of the cause, occurrence rate and negative impact of disasters on humanity have increased in recent decades; some possible reasons include growth of world population, industrialization and urbanization, overpopulation in cities, and ongoing threats of wars and conflicts [3].
Disasters share certain commonalities, e.g., damage to infrastructure; panic, chaos, and disorganization of healthcare delivery; shortages of medical material and personnel; and an unanticipated increase in the numbers of patients presenting to the emergency services in a very short time. Therefore, an “all hazards model” (i.e., managing different hazard scenarios with a common plan for hazard mitigation and preparedness) [4] has been introduced. On the other hand, mechanisms, risk factors, and measures to mitigate damage and to treat affected patients may differ among various disasters. For example, wars may result in gunshot injuries, bleeding, and exposure to exogenous nephrotoxins; earthquakes are characterized by crush injuries and exposure to endogenous nephrotoxins, whereas tsunamis and hurricanes result in drowning [5]. Logistically, natural disasters may affect a huge population for a very short time period, whereas adverse effects of wars may last for several years; e.g., the Syrian war is now in its 11th year.
Disasters have many devastating consequences for the affected community. Although the entire population is at risk of being affected, children, particularly if they are chronically ill, represent a uniquely vulnerable group due to their special medical needs and dependence on their parents/caregivers [6]. In this review, we focus on the crises faced by pediatric dialysis and kidney transplant (KTx) patients during disasters, and interventions to be performed before, during, and after the event to mitigate the extent of their problems.
Statistics
Since 1994, natural disasters have affected more than 5 billion people around the globe [7]. In 2021, the Emergency Event Database (EM-DAT) recorded a total of 432 natural disasters, which affected 101.8 million people worldwide [8]. The most common events were floods, storms, and earthquakes. Asia was the most frequently and severely impacted continent, accounting for 40% of all natural hazards and 66% of the affected population.
Considering man-made disasters, during 2020, 34 armed conflicts were identified globally, which were most frequent in developing countries in Africa, Asia, and the Middle East [9]. Following the invasion of Ukraine on 24 February 2022, Europe also faced an armed conflict. In recent decades, conflicts affected not only the armed forces, but also civilians, including vulnerable population segments, especially the children. It is estimated that nearly 1 in every 5 children worldwide live in conflict zones and experience threats of wars [10].
Disasters mostly affect low-middle-income countries or poorer communities in well-developed nations, who already have a higher burden of health problems in their routine daily lives compared to their wealthier peers [11, 12]. Disasters may exaggerate existing health problems, causing severe consequences in dialysis and transplant patients, who need extensive and expensive technical infrastructure, equipment, medications, disposables, hygienic environments, and well-trained medical personnel. Although most publications come from high-income countries, their preparedness for disasters is not satisfactory either [13].
Despite the huge number of children living with dangers of disasters, very little is known about the fate of pediatric patients receiving kidney replacement therapy (KRT) in this setting.
Effects of disasters on pediatric dialysis and kidney transplant patients
General aspects
Mass disasters have direct and indirect effects on the general population. Because of their anatomical and physiological characteristics, limited self-preservation skills, and dependence on their caregivers, the risk of direct injuries to children is high [14]. In 2016, during the Syrian war, 23% of civilian casualties were children [15]. On 1 June 2022, the United Nations Human Rights Monitoring Mission in Ukraine reported, overall, 4168 killed and 4945 injured civilians, among whom 268 and 423 were children, respectively [16]. Most of these children are presumed to be previously healthy.
Of particular importance, the mental health of children is at lifelong risk. Psychological and psychiatric manifestations include acute stress reactions, post-traumatic stress disorder, depression, panic attacks, anxiety, phobia, and even psychosis [17, 18]. We have no information on the fate of chronically ill children, especially dialysis and KTx patients, as disaster victims. It can be speculated that they would be influenced at least as severely or more seriously than healthy children because of their healthcare needs.
Special aspects
In addition to direct injuries, several features adversely affect the health of pediatric kidney patients during mass disasters (Table 1) [19, 20].
Hemodialysis (HD) patients
Following natural disasters, dialysis units may not be able to perform routine treatments, and patients on maintenance HD may miss their scheduled dialysis sessions resulting in increased risks of morbidity and mortality [21,22,23,24,25]. Compared to natural disasters, armed conflicts last longer, and the consequences are even more grave [26].
Pediatric HD patients may be affected more seriously than adults on HD due to the limited availability of pediatric-sized equipment and personnel with pediatric dialysis experience [19, 27, 28]. Also, vascular access problems are more frequent as compared to adults [29]. Furthermore, children are usually less able to tolerate missed dialysis sessions as compared to adults because of a higher metabolic rate and reduced adherence to dietary restrictions, particularly when under stress.
Peritoneal dialysis (PD) patients
Compared to HD, patients on PD are less dependent on infrastructure, technology, specialized facilities, and healthcare personnel [30, 31]; therefore, the medical and logistical management of PD patients in disaster circumstances is easier than that of patients on HD. However, transport of bulky PD solutions to the affected area may be problematic.
Unhygienic conditions may increase the risk of both PD and HD exit site infections with the risk of peritonitis or septicemia [32, 33]. Hypervolemia and leakage due to lack of appropriate CAPD solutions have also been reported [32].
Children with acute kidney injury (AKI)
In addition to chronic dialysis patients, healthy children, who are injured during disaster, may also suffer from various types (prerenal, intrinsic, and postrenal) of AKI and need dialysis support. The most common etiology of AKI is crush syndrome [6], although this risk is lower in children due to their lower body surface area as compared to adults [34, 35]. Initially, crush injury-related AKI is prerenal; however, afterwards, many factors lead to intrinsic renal AKI due to acute tubular necrosis (ATN) [36].
Kidney transplant patients
Kidney transplant recipients face several important problems in disaster settings. During the COVID-19 pandemic, a cross-sectional web-based study among children with chronic diseases, including KTx patients, revealed that 3.6% of the patients experienced medication interruptions [37]. The non-availability of medications and/or noncompliance with therapy under chaotic circumstances may lead to a high risk of rejection [28, 38]. Importantly, noncompliance with therapy is particularly common in adolescent transplant recipients [39]. Furthermore, it can be speculated that, due to unhygienic housing conditions, the risk for all kinds of infections may increase in the immunosuppressed state [28].
Management of pediatric dialysis and kidney transplant patients during disasters
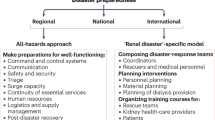
Disaster preparedness and a prompt response are key factors to prevent and/or mitigate adverse effects on the affected population. These measures can be studied in three phases: before, during, and after the disaster (Fig. 1).
Preparedness towards disasters, response after a disaster, and post-disaster interventions targeting optimal response in pediatric nephrology centers and pediatric patients/their caregivers. In disaster-prone countries/regions, preparedness is vital to decrease extent of post-disaster chaos and disorganization. Following a catastrophe, response includes coordination, mitigation, and action plans, all of which are mandatory to save as many lives as possible; internal help from other regions of the country and external help from other countries may be very useful if disasters cannot be coped with locally. Response is far from being ideal even in well-developed countries that are faced with frequent disasters; therefore, post-disaster interventions may be useful for improvement in disaster response in future events
Pre-disaster preparations
A national renal disaster response coordination system and planning is essential to decrease the extent of post-disaster chaos and disorganization. Subdivisions of this system as regional and also kidney center-based planning may be useful in providing pragmatic solutions to disaster-related problems.
The special needs of pediatric patients are often overlooked in the hospital disaster preparedness plans [40]. Planning for pediatric KRT is crucial and should include preparations at the level of the nephrology center as well as personal preparation of patients.
Center-level preparations
Since disasters cannot be anticipated, a sustainable and regularly updated disaster plan is needed [24, 25, 41]. Disaster planners should aim to deal with all unfavorable conditions, including local and general infrastructure problems (Table 2) [20, 42], which cover action plans on how to overcome shortages of dialysis equipment and supplies [41].
Considering personnel shortage, additional staff (who previously worked in the dialysis center, retired and community volunteers who can support the service beyond medical procedures and care) should be identified. Disasters occur from time-to-time, and unapplied medical information is easily forgotten. To provide the most efficient healthcare and to minimize the risk of malpractice, medical staff should be trained on disaster emergencies and disaster plans at appropriate intervals. Multidisciplinary psychosocial support teams with social workers, consultants, interpreters, and religious representatives should be established and trained on potential scenarios to provide services to staff and patients.
It has been reported that dialysis patients’ unawareness of disaster preparedness plans of their centers can lead to missed dialysis sessions [25]. Therefore, patients and their families/caregivers should be informed of these plans.
Preparation of patients and caregivers
Educating and informing patients and their families/caregivers about an emergency can be useful to minimize the extent of risks (Table 2) [20, 42, 43]. Due to the risk that primary caregivers will be personally harmed by the disaster, another family member should also be trained to assume the responsibility. Families should be informed about the risk of interruption of the regular dialysis program and living in crowded, unhygienic conditions, which may trigger infections.
Patients’ and their caregivers’ training on self-disconnection technique from the machine is critical [44], and disaster drills can be performed to explain evacuation procedures in the case of an emergency. Primary caregivers of patients on automated PD (APD) program should be trained to perform manual exchanges.
An emergency bag containing at least a 2-week supply of regular medications and backup drugs is important for disaster preparedness at home (Table 2) [20, 42]. Parents/caregivers should keep reports describing current HD or PD prescriptions, medications, and also center contact information in a safe and easily accessible location. An emergency preparedness checklist may be useful to avoid any mistakes during the chaos of mass disasters [45].
Interventions during the disaster
Center-level interventions
Firstly, the structural condition of the centers should be evaluated. Capacity planning and the scope of healthcare cannot be assessed until the extent of building damage is determined. Management of manpower is vital to ensure provision of healthcare. The number of functioning personnel, staff duty schedule, and extra work hours should be established, and previously determined action plan be activated. The number of personnel who can be sent to other centers or vice versa should be also clarified. Patients should be referred to neighboring centers if their own centers are not functioning.
A communication network among staff, patients, and other stakeholders, including authorities and non-governmental organizations (NGOs), is critical to optimize healthcare coordination [41]. Determining and sharing of telemedicine channels on social media platforms may help direct patients to the best available centers. Several options (GoogleDuo, WhatsApp, Facetime) are applicable for telemedicine interaction [37]. Short informative videos and voice recordings can be sent to cell phones. Group chats for predefined problems may be conducted.
Considering limited resources, it is important to review routine laboratory assessments; only the most urgent biochemical parameters should be analyzed.
Burnout (prolonged response to chronic interpersonal stressors of the job or psychological response to work-related stress) is an important health problem among all healthcare personnel during disasters and may contribute to less efficient healthcare delivery [46]. It is characterized by exhaustion, feelings of cynicism, and professional inefficiency, and may be associated with psychologic/psychiatric and somatic problems. Burnout may result in medical mistakes and malpractice, patient disappointment, poor health outcomes, and a low morale among team members [46, 47].
Risk of burnout may be minimized by pre-disaster organizational preparedness, and intra-disaster specific measures, such as improving safety concerns and worries for malpractice, supporting mental health, improving medical staffing shortage, decreasing workload, and providing flexibility in working circumstances. Training on coping with stress and problematic conditions and maintaining physical health may be useful for preventing burnout as well [47].
If needs cannot be coped with locally, national and international help may become necessary, as seen with previous mass disasters [48]. The Renal Disaster Relief Task Force of the ISN [49], ERA [50], and ESPN [51] have been proven useful in previous disasters and the recent disaster in Ukraine. In addition to personnel and material help, consultation with foreign specialists proved very useful both for obtaining medical advice and to discuss logistic problems.
Interventions towards patients and caregivers
Patients and their caregivers should be informed of the center status, transportation options, and alternative pediatric nephrology/dialysis centers. When patients are transferred to other centers, it may be helpful for patient adaptation if one or more members of the local dialysis team accompany them, where possible. If the child’s usual dialysis program cannot be provided, high dose furosemide may be useful to prevent volume overload in patients with residual kidney function. Similarly, withholding beta blockers and renin–angiotensin–aldosterone blockers should be considered in patients at risk of hyperkalemia. Some practical suggestions on patient management are provided in Box 1.
Box 1. Practical suggestions for the patients and their caregivers, towards solution of frequent problems during mass disasters [20, 74].
Communication among patients |
-Create a network to communicate with other patients/families |
-Arrange group transportation to the center |
-Exchange drugs, PD fluids |
Unhygienic environments |
-Follow hygiene rules strictly |
-Wear masks |
-Consume safe, healthy, and proper food |
Limited dialysis possibilities |
-Avoid potassium-rich food |
-Decrease fluid intake |
-Consume salt-free diet |
-Consider additional medications (e.g., phosphate/potassium binders, sodium bicarbonate) |
PD practice difficulties |
-During power outages, use non-heated solutions or, during cold weather, consider wrapping up the solutions with hot-water bags |
-If a suitable antiseptic solution is not available for catheter exit site care, the following solution can be prepared: • 6 oz. (3/4 cup) boiled or bottled water • 4 oz. (1/2 cup) white vinegar • 1 ¾ teaspoons table salt is mixed and shaken well, put into a clean spray bottle and this mixture can be used for 1 week |
Hemodialysis patients
In an emergency situation, triage is extremely important [24]; patients who need urgent dialysis due to volume overload or other uremic symptoms and those with serious biochemical abnormalities should take priority for dialysis.
Problems related with water are common during mass disasters. Switching from hemodiafiltration to hemodialysis reduces water consumption. In addition, if the water purity is suboptimal, low-flux dialyzers should be preferred instead of high-flux filters. In case of problems with the water supply, the use of tank water can be considered [52]. Centers should be vigilant about the contamination of water supply if common symptoms such as fever, rigors, or signs of hemolysis appear in HD patients.
Reducing the number of weekly dialysis sessions and the duration of each session is critical in overwhelmed centers; this strategy is also valuable to decrease the transportation needs of the patients. The duration or number of dialysis sessions can be reduced starting from patients with residual kidney function and without risky laboratory parameters.
Dialysis inadequacy due to reduced number of dialysis sessions or shortened dialysis duration can be partially overcome by increasing dialysis efficacy. For example, in patients without a risk for dialysis disequilibrium, the upper limits of dialyzer surface area (1–1.2 times body surface area) and blood flow rate (5–8 ml/min/kg or 150–240 ml/min/m2 body surface area) can be used [53]. The dialysate flow rate should also be adjusted for water supply. It can be as low as 1.2 times the blood flow rate if the water supply is restricted; however, it can be increased up to 2 times the blood flow rate to increase the diffusion in limited dialysis time.
Switching from HD to PD should be considered if maintenance of HD is not possible. If required, portable home dialysis machines with bagged fluid can be considered. Most trained dialysis nurses will quickly adapt to using these machines, but on-line video support from expert centers must be available.
Peritoneal dialysis patients
Patients should contact their centers in the case of non-availability of their prescribed PD fluids. As a practical solution, PD fluids may be borrowed from other patients, or a new PD program can be prescribed for the available fluids.
In addition, the available PD fluid bags may need to be used sparingly to mitigate this problem. In patients on APD, longer treatment durations may be useful to ensure that solutions are fully consumed. Considering patients on continuous ambulatory peritoneal dialysis (CAPD), treatment might be continued without disconnecting the same bag as long as the volume of PD solution is sufficient. This may also be useful to reduce the risk of infection by avoiding frequent connections. If the environment is not suitable for connections, treatment may be postponed until circumstances improve [54].
Automated PD is most commonly used in the pediatric population. However, APD patients may not be able to continue their treatment during power outages and may need to change their dialysis modality [32]; therefore, patients using APD should have CAPD replacement solutions as well [42]. “Home-made” PD solutions can be produced in the hospital pharmacy as a last measure [55]. Switching from PD to HD or a combination of PD and HD as a hybrid treatment may be another option.
Peritonitis is frequent during mass disasters [32]; therefore, patients should be trained on empirical administration of antibiotics if they experience peritonitis symptoms and cannot reach their physicians.
AKI patients
Early and appropriate fluid therapy is vital to prevent or improve the outcome of AKI in crush victims. Fluid administration (for children: 0.9% NaCl, 15–20 ml/kg of body weight per hour) should be started as soon as safely possible after the victim is found [19, 56, 57], and maintained (0.33% or 0.45% NaCl solution at a rate of 3.000–6.000 ml/m2/24 h) during the first days [58]. In cases with intrinsic renal AKI, dialysis support may be necessary. Dialysis modality should be chosen keeping in mind the need for possible long-term dialysis for the child.
Infections and related problems are very common medical complications increasing morbidity and mortality among adult and pediatric crush victims [59, 60]. These problems can be minimized by performing meticulous wound care, avoiding unnecessary fasciotomies, following hygienic measures, and early diagnosis and treatment [56]. Long-term renal consequences of crush-related AKI are unclear; however, considering the high risk of chronic kidney disease (CKD) after AKI [61, 62], one can speculate that many pediatric victims may be faced with the risk of chronic kidney failure in the long term.
Kidney transplant recipients
Telemedicine for any modification in immunosuppressants may be useful for inexperienced physicians in the management of transplant patients. Communication and connections via non-governmental organizations (NGOs) and patient groups might be helpful to obtain medications. Switching between immunosuppressive medications should be considered when the usual drugs are no longer available. Changing from mycophenolate mofetil (MMF) to azathioprine (AZA), from tacrolimus to cyclosporine, or vice versa is possible. If relevant drugs are not accessible by any route, the dosage of available drugs can be increased [63].
Living in unhygienic conditions may increase the risk of infections [64], especially in immunosuppressed transplant recipients. In the recent war in Ukraine, the need for hygienic and safe shelters, in which children with their caregivers and medical personnel can stay, was highlighted. Many KTx and chronic dialysis patients were unable to protect themselves from the COVID-19 pandemic despite shielding precautions [65].
Post-disaster interventions and rehabilitation
Overall, post-disaster interventions target treating neglected physical and mental problems during the active phase of disasters, and also improving social challenges. Learning from previous mistakes is important.
Medical problems
During the chaotic conditions of disasters, many complications in dialysis and transplant patients may go undetected, or untreated even if they had been detected. Most of these problems are related to underdialysis, which may include, but are not limited to, fluid overload, suboptimal treatment of CKD mineral bone disease, anemia, and heart failure in dialysis patients. A-V access problems in HD patients and peritoneal access problems in PD patients deserve special attention because treatment of above-mentioned complications may not be possible without optimizing dialysis adequacy, which necessitates best possible routes for dialysis performance. All these problems should be revisited and treated accordingly.
Mental problems
Pediatric patients on KRT are already susceptible to various mental troubles. Extreme stress and psychologic effects of armed conflict may trigger several mental health problems [17, 18]. These problems may need skilled help from experienced pediatric psychologists or psychiatrists.
Social drawbacks
Children requiring KRT are dependent upon their caregivers for survival; morbidity or mortality of these individuals may deeply affect the child’s well-being. Therefore, separated families must be united as quickly as possible. Education of the pediatric kidney patients, which is problematic even in normally functioning societies, may be hampered by austere circumstances. Help of authorities and NGOs may be asked for in accomplishing these targets [66].
Preparations for future disasters
Unfortunately, natural and man-made disasters are inevitable, and medical/logistical mistakes are quite common during these catastrophes. In order to avoid repetition of the mistakes, briefing and debriefing sessions are needed about evaluating disaster response from a pediatric nephrology point of view. Revisions in the action plans may be required to mitigate the effects of disasters on this vulnerable population. Also, topics on pediatric disaster medicine, disaster response, special problems faced by pediatric nephrologists and kidney patients, and potential solutions for these problems should be included in continuing education programs and web pages of IPNA, ESPN, and other international and national pediatric nephrology societies. Creating a Disaster Relief Task Force by these societies is useful to collaborate with the centers and intervene in a timely manner in the acute phase of disasters.
Challenges related with pediatric refugee kidney patients
Wars can force people to flee their homes. Displacement may be within the borders of the home country (internally displaced persons) or across the national borders (refugees). Low-income countries host approximately 85% of the world’s refugee population [67]. According to the data of the United Nations Refugee Agency (UNHCR), a total of 35 million forcibly displaced children exist across the globe at the end of 2020, and nearly 13 million of them being refugees [67, 68].
There is limited information about the outcome of pediatric refugee patients receiving KRT. In a 6-year period between 2005 and 2010, 335 Afghan pediatric kidney patients were reported in Iran, of whom 116 (35%) were diagnosed with stage 5 CKD, although no information existed about KRT practice in this population [69]. Another study provided data on 633 Syrian refugee children with kidney disease, from 22 pediatric nephrology centers in Turkey between 2012 and 2020. Fifty-eight of these patients were on a chronic dialysis program; 31 of them were being treated with HD and 27 with PD, while 6 children survived with KTx; maintenance dialysis was started in 54 in Turkey [70]. A survey among German pediatric nephrologists revealed that a total of 69 refugee children, who had arrived in the country between 2015 and 2017, had been treated with KRT (43 on HD, 9 on PD, and 17 with KTx) [71]. The number of refugee children on dialysis (n = 52) represented 22% of the total pediatric dialysis population (n = 232) in Germany.
All problems cited for pediatric dialysis and KTx patients living in the affected area are valid for displaced patients as well. Moreover, they are at risk of limited access to basic needs and healthcare during their travel and also at the destination [72]. Most importantly, the vast majority of refugee patients are dependent upon the support of their caregivers, who may be separated from the children [19]. This logistic drawback may result in deficient treatment, psychological trauma, morbidity, and even mortality.
In addition, refugee kidney patients on KRT may suffer from financial barriers, complex referral systems, and limited healthcare in the host country, whereas suboptimal health education, lack of their previous medical data, and language barriers exaggerate all these problems [70, 73], [74]. Considering that most of the host countries are low- and middle-income countries with limited resources, management of all these medical, social, and logistic problems are very complex. International help and support is essential in order to mitigate, if not to avoid, these drawbacks [66].
During evacuation, priority must be given to pediatric KRT patients requiring dialysis, because this group is extremely vulnerable. Triage at admission centers is also critical; patients in urgent need of dialysis should be identified and dialyzed at the earliest convenience.
Conclusions
Disasters are inevitable and occur unexpectedly. Vulnerable populations, especially pediatric kidney patients on KRT, are even more seriously affected in suboptimal circumstances. These children may suffer from long-lasting physical, mental, and social trauma even if they survive the disaster. Therefore, training of pediatric nephrologists and also other specialties about the hazards to these patients during disasters is mandatory. Disaster planning should include specific precautions to protect pediatric kidney patients. Adapting treatment protocols for pediatric dialysis and KTx patients during active phases of conflicts and applying rehabilitation measures after termination of conflicts may reduce the impact of disasters on these children.
References
WHO/EHA (2002) Disasters & emergencies. Definitions. https://apps.who.int/disasters/repo/7656.pdf. Accessed 4 June 2022
The United Nations International Strategy for Disaster Reduction (UNISDR) (2009) Disaster risk reduction. https://www.unisdr.org/files/7817_UNISDRTerminologyEnglish.pdf. Accessed 4 June 2022
Al-Jazairi AF (2017) Disasters and disaster medicine. https://www.intechopen.com/chapters/58936. Accessed 4 June 2022
Bodas M, Kirsch TD, Peleg K (2020) Top hazards approach – rethinking the appropriateness of the All-Hazards approach in disaster risk management. https://www.sciencedirect.com/science/article/abs/pii/S2212420919316358. Accessed 25 Aug 2022
Sever MS, Vanholder R, Luyckx V, Eckardt KU, Kolesnyk M, Wiecek A, Pawlowicz-Szlarska E, Gallego D, Shroff R, Skoberne A, Nistor I, Sekkarie M, Ivanov D, Noruisiene E, Tuglular S, Renal Disaster Relief Task Force of the ERA (2022) Armed conflicts and kidney patients: a consensus statement from the renal disaster relief task force of the ERA. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfac247
Sever MS, Sever L, Vanholder R (2020) Disasters, children and the kidneys. Pediatr Nephrol 35:1381–1393
Childfund (2013) The devastating impact of natural disasters. https://www.childfund.org/Content/NewsDetail/2147489272/. Accessed 4 June 2022
EM-DAT, The Internationale Disaster Database (2021) 2021 Report. https://www.emdat.be/publications. Accessed 4 June 2022
Milián IN ea (2021) Escola de Cultura de Pau. Alert 2021! Report on conflicts, human rights and peacebuilding. Barcelona: Icaria. https://reliefweb.int/sites/reliefweb.int/files/resources/alerta21i.pdf. Accessed 4 June 2022
Graham G; Save the Children (2019) Stop the war on children. Available at: https://www.stopwaronchildren.org/ Accessed April 5, 2022
Roy N, Thakkar P, Shah H (2011) Developing-world disaster research: present evidence and future priorities. Disaster Med Public Health Prep 5:112–116
Center for the study of traumatic stress disasters and poverty: natural disasters disproportionately affect the world’s low-income countries https://www.cstsonline.org/assets/media/documents/CSTS_FS_Disasters_and_Poverty_Natural_Disasters_Disproportionally_Affect_the_Worlds_low_income.pdf. Accessed 25 Aug 2022
Lee AC, Booth A, Challen K, Gardois P, Goodacre S (2014) Disaster management in low- and middle-income countries: scoping review of the evidence base. Emerg Med J 31:e78-83
Grindlay J, Breeze KM (2016) Planning for disasters involving children in Australia: a practical guide. J Paediatr Child Health 52:204–212
Guha-Sapir D, Schluter B, Rodriguez-Llanes JM, Lillywhite L, Hicks MH (2018) Patterns of civilian and child deaths due to war-related violence in Syria: a comparative analysis from the Violation Documentation Center dataset, 2011–16. Lancet Glob Health 6:e103–e110
United Nations High Commissioner for Human Rights (OHCHR) (2022) Number of civilian casualties during the war in Ukraine 2022
Kar N (2009) Psychological impact of disasters on children: review of assessment and interventions. World J Pediatr 5:5–11
Slone M, Mann S (2016) Effects of war, terrorism and armed conflict on young children: a systematic review. Child Psychiatry Hum Dev 47:950–965
Sever L, Balat A (2020) Renal crisis in children during armed conflict. Semin Nephrol 40:408–420
Vanholder R, De Weggheleire A, Ivanov DD, Luyckx V, Slama S, Sekkarie M, Sever MS, Shroff R (2022) Continuing kidney care in conflicts. Nat Rev Nephrol. https://doi.org/10.1038/s41581-022-00588-7
Sever MS, Erek E, Vanholder R, Kalkan A, Guney N, Usta N, Yilmaz C, Kutanis C, Turgut R, Lameire N (2004) Features of chronic hemodialysis practice after the Marmara earthquake. J Am Soc Nephrol 15:1071–1076
Kutner NG, Muntner P, Huang Y, Zhang R, Cohen AJ, Anderson AH, Eggers PW (2009) Effect of Hurricane Katrina on the mortality of dialysis patients. Kidney Int 76:760–766
Anderson AH, Cohen AJ, Kutner NG, Kopp JB, Kimmel PL, Muntner P (2009) Missed dialysis sessions and hospitalization in hemodialysis patients after Hurricane Katrina. Kidney Int 75:1202–1208
Lempert KD, Kopp JB (2019) Renal failure patients in disasters. Disaster Med Public Health Prep 13:782–790
Smith RS, Zucker RJ, Frasso R (2020) Natural disasters in the Americas, dialysis patients, and implications for emergency planning: a systematic review. Prev Chronic Dis 17:E42
International Committee of the Red Cross (ICRC) Hidden cost of war: in Yemen, thousands could die of kidney failure. https://www.icrc.org/en/document/yemen-hidden-cost-war-thousands-kidney-dialysis-patients-risk-death
Sugisawa H, Shinoda T, Shimizu Y, Kumagai T (2021) Cognition and implementation of disaster preparedness among japanese dialysis facilities. Int J Nephrol 2021:6691350
Sever MS, Lameire N, Van Biesen W, Vanholder R (2015) Disaster nephrology: a new concept for an old problem. Clin Kidney J 8:300–309
Shroff R, Wright E, Ledermann S, Hutchinson C, Rees L (2003) Chronic hemodialysis in infants and children under 2 years of age. Pediatr Nephrol 18:378–383
Zoraster R, Vanholder R, Sever MS (2007) Disaster management of chronic dialysis patients. Am J Disaster Med 2:96–106
Kumar V, Ramachandran R, Rathi M, Kohli HS, Sakhuja V, Jha V (2013) Peritoneal dialysis: the great savior during disasters. Perit Dial Int 33:327–329
Ozener C, Ozdemir D, Bihorac A (2000) The impact of the earthquake in northwestern Turkey on the continuous ambulatory peritoneal dialysis patients who were living in the earthquake zone. Adv Perit Dial 16:182–185
Gorbatkin C, Finkelstein FO, Kazancioglu RT (2020) Peritoneal Dialysis during Active War. Semin Nephrol 40:375–385
Sever MS, Erek E, Vanholder R, Akoglu E, Yavuz M, Ergin H, Tekce M, Korular D, Tulbek MY, Keven K, van Vlem B, Lameire N, Marmara Earthquake Study Group (2001) The Marmara earthquake: epidemiological analysis of the victims with nephrological problems. Kidney Int 60:1114–1123
Hatamizadeh P, Najafi I, Vanholder R, Rashid-Farokhi F, Sanadgol H, Seyrafian S, Mooraki A, Atabak S, Samimagham H, Pourfarziani V, Broumand B, Van Biesen W, Lameire N (2006) Epidemiologic aspects of the Bam earthquake in Iran: the nephrologic perspective. Am J Kidney Dis 47:428–438
Vanholder R, Sever MS, Erek E, Lameire N (2000) Rhabdomyolysis. J Am Soc Nephrol 11:1553–1561
Aydemir S, Ocak S, Saygili S, Hopurcuoglu D, Haslak F, Kiykim E, Aktuglu Zeybek C, Celkan T, Demirgan EB, Kasapcopur O, Cokugras H, Kiykim A, Canpolat N (2021) Telemedicine Applications in a Tertiary Pediatric Hospital in Turkey During COVID-19 Pandemic. Telemed J E Health 27:1180–1187
Kadowaki M, Saito M, Amada N, Haga I, Nakamura A, Tokodai K (2014) Medication compliance in renal transplant patients during the Great East Japan Earthquake. Transplant Proc 46:610–612
Maximo Silva AC, Sanders-Pinheiro H, Leite RF, Joseph MPC, Pestana JOM, Schirmer J, Bartira de Aguiar R (2020) Nonadherence to immunosuppressive medications following pediatric kidney transplantation within full cost coverage health system: prevalence and correlates. Exp Clin Transplant 18:577–584
Burke RV, Iverson E, Goodhue CJ, Neches R, Upperman JS (2010) Disaster and mass casualty events in the pediatric population. Semin Pediatr Surg 19:265–270
Sever MS, Lameire N, Vanholder R (2009) Renal disaster relief: from theory to practice. Nephrol Dial Transplant 24:1730–1735
Tamura H, Kuraoka S, Hidaka Y, Nagata H, Nakazato H (2020) Pediatric Peritoneal Dialysis During the Recent Earthquakes in Japan and Recommendations for Future Disaster Preparation. Kidney Int Rep 5:1061–1065
Murakami N, Siktel HB, Lucido D, Winchester JF, Harbord NB (2015) Disaster Preparedness and Awareness of Patients on Hemodialysis after Hurricane Sandy. Clin J Am Soc Nephrol 10:1389–1396
Liossatou A, Golland E (2021) Disaster preparedness and evacuation plan (DPEP) in haemodialysis units: patients’ emergency self-disconnection through “Clamp and Cut” procedure. https://www.edtnaerca.org/resource/edtna/files/ElectronicLibrary_Managing_5-21%20(2).pdf. Accessed 14 June 2022
IPRO End stage renal disease network program Be Prepared for Emergencies - Information to keep on hand. https://esrd.ipro.org/wp-content/uploads/2021/04/ALL-NW-Disaster-Tip-Sheet_V1-1.pdf. Accessed 4 June 2022
Maslach C, Leiter MP (2016) Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry 15:103–111
Sever MS, Ortiz A, Maggiore U, Bac-Garcia E, Vanholder R (2021) Mass disasters and burnout in nephrology personnel: from earthquakes and hurricanes to COVID-19 pandemic. Clin J Am Soc Nephrol 16:829–837
Vanholder R, Sever MS, De Smet M, Erek E, Lameire N (2001) Intervention of the Renal Disaster Relief Task Force in the 1999 Marmara, Turkey earthquake. Kidney Int 59:783–791
Lameire N, Sever MS, Van Biesen W, Vanholder R (2020) Role of the International and national renal organizations in natural disasters: strategies for renal rescue. Semin Nephrol 40:393–407
European Renal Association (ERA) Help for Ukraine. https://www.era-online.org/en/help-for-ukraine/. Accessed 16 June 2022
European Society for Paediatric Nephrology (ESPN) Ukraine Task Force. https://www.espn-online.org/ukraine-task-force/. Accessed 16 June 2022
Centers for Disease Control and Prevention (CDC) Safe Use of “Tanker” Water for Dialysis. https://www.cdc.gov/disasters/watertanker.html. Accessed 14 June 2022
Fischbach M, Fothergill H, Zaloszyc A, Seuge L (2012) Hemodiafiltration: the addition of convective flow to hemodialysis. Pediatr Nephrol 27:351–356
Woodrow G, Fan SL, Reid C, Denning J, Pyrah AN (2017) Renal Association Clinical Practice Guideline on peritoneal dialysis in adults and children. BMC Nephrol 18:333
Cullis B, Al-Hwiesh A, Kilonzo K, McCulloch M, Niang A, Nourse P, Parapiboon W, Ponce D, Finkelstein FO (2021) ISPD guidelines for peritoneal dialysis in acute kidney injury: 2020 update (adults). Perit Dial Int 41:15–31
Sever MS, Vanholder R (2013) Management of crush victims in mass disasters: highlights from recently published recommendations. Clin J Am Soc Nephrol 8:328–335
Gunal AI, Celiker H, Dogukan A, Ozalp G, Kirciman E, Simsekli H, Gunay I, Demircin M, Belhan O, Yildirim MA, Sever MS (2004) Early and vigorous fluid resuscitation prevents acute renal failure in the crush victims of catastrophic earthquakes. J Am Soc Nephrol 15:1862–1867
Iskit SH, Alpay H, Tugtepe H, Ozdemir C, Ayyildiz SH, Ozel K, Bayramicli M, Tetik C, Dagli TE (2001) Analysis of 33 pediatric trauma victims in the 1999 Marmara, Turkey earthquake. J Pediatr Surg 36:368–372
Keven K, Ates K, Sever MS, Yenicesu M, Canbakan B, Arinsoy T, Ozdemir N, Duranay M, Altun B, Erek E (2003) Infectious complications after mass disasters: the Marmara earthquake experience. Scand J Infect Dis 35:110–113
Donmez O, Meral A, Yavuz M, Durmaz O (2001) Crush syndrome of children in the Marmara Earthquake, Turkey. Pediatr Int 43:678–682
Stewart IJ, Sosnov JA, Howard JT, Orman JA, Fang R, Morrow BD, Zonies DH, Bollinger M, Tuman C, Freedman BA, Chung KK (2015) Retrospective analysis of long-term outcomes after combat injury: a hidden cost of war. Circulation 132:2126–2133
Greenberg JH, Coca S, Parikh CR (2014) Long-term risk of chronic kidney disease and mortality in children after acute kidney injury: a systematic review. BMC Nephrol 15:184
Alasfar S, Isreb M, Kaysi S, Hatahet K (2020) Renal transplantation in areas of armed conflict. Semin Nephrol 40:386–392
Baba S, Taniguchi H, Nambu S, Tsuboi S, Ishihara K, Osato S (1996) The Great Hanshin earthquake. Lancet 347:307–309
Canpolat N, Yildirim ZY, Yildiz N, Tasdemir M, Goknar N, Evrengul H, Gulmez R, Aksu B, Dursun H, Ozcelik G, Yavascan O, Cicek RY, Tulpar S, Hacihamdioglu DO, Nayir A, Alpay H (2022) COVID-19 in pediatric patients undergoing chronic dialysis and kidney transplantation. Eur J Pediatr 181:117–123
UNICEF War in Ukraine: support for children and families. https://www.unicef.org/emergencies/war-ukraine-pose-immediate-threat-children. Accessed 16 June 2022
United Nations Refugee Agency UNHCR Global trends forced displacement in 2020. https://www.unhcr.org/refugee-statistics/. Accessed 4 June 2022
United Nations Refugee Agency UNHCR (2020) Figures at a Glance. https://www.unhcr.org/figures-at-a-glance.html. Accessed 4 June 2022
Otoukesh S, Mojtahedzadeh M, Cooper CJ, Tolouian R, Said S, Ortega L, Didia SC, Behazin A, Sherzai D, Blandon P (2014) Lessons from the profile of kidney diseases among Afghan refugees. Med Sci Monit 20:1621–1627
Balat A, Kilic BD, Aksu B, Kara MA, Buyukcelik M, Agbas A, Eroglu FK, Gungor T, Alaygut D, Yildiz N, Bastug F, Atmis B, Melek E, Elmaci M, Tulpar S, Pehlivanoglu C, Doven SS, Comak E, Tabel Y, Gemici A, Uysal B, Ozzorlar GS, Kucuk N, Delibas A, Ozcelik G, Goknar N, Dursun I, Ertan P, Ozunan IA, Sonmez F (2022) Kidney disease profile and encountered problems during follow-up in Syrian refugee children: a multicenter retrospective study. Pediatr Nephrol 37:393–402
Lemke J, Schild R, Konrad M, Pape L, Oh J, Members of the German Society of Pediatric Nephrology (2021) Distribution and management of the pediatric refugee population with renal replacement: a German pediatric cohort. Pediatr Nephrol 36:271–277
Kadir A, Shenoda S, Goldhagen J, Pitterman S, Section On International Child Health (2018) The effects of armed conflict on children. Pediatrics 142:e20182586
Van Biesen W, Vanholder R, Ernandez T, Drewniak D, Luyckx V (2018) Caring for migrants and refugees with end-stage kidney disease in Europe. Am J Kidney Dis 71:701–709
Center for Disease Control (CDC) Natural disasters and severe weather. https://www.cdc.gov/disasters/icfordialysis.html. Accessed 17 June 2022
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sever, L., Pehlivan, G., Canpolat, N. et al. Management of pediatric dialysis and kidney transplant patients after natural or man-made disasters. Pediatr Nephrol 38, 315–325 (2023). https://doi.org/10.1007/s00467-022-05734-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05734-8