Abstract
Background
Fluid overload associates with poor outcomes after neonatal cardiac surgery, but consensus does not exist for the most clinically relevant method of measuring fluid balance (FB). While weight change-based FB (FB-W) is standard in neonatal intensive care units, weighing infants after cardiac surgery may be challenging. We aimed to identify characteristics associated with obtaining weights and to understand how intake/output-based FB (FB-IO) and FB-W compare in the early postoperative period in this population.
Methods
Observational retrospective study of 2235 neonates undergoing cardiac surgery from 22 hospitals comprising the NEonatal and Pediatric Heart and Renal Outcomes Network (NEPHRON) database.
Results
Forty-five percent (n = 998) of patients were weighed on postoperative day (POD) 2, varying from 2 to 98% among centers. Odds of being weighed were lower for STAT categories 4 and 5 (OR 0.72; 95% CI 0.53–0.98), cardiopulmonary bypass (0.59; 0.42–0.83), delayed sternal closure (0.27; 0.19–0.38), prophylactic peritoneal dialysis use (0.58; 0.34–0.99), and mechanical ventilation on POD 2 (0.23; 0.16–0.33). Correlation between FB-IO and FB-W was weak for every POD 1–6 and within the entire cohort (correlation coefficient 0.15; 95% CI 0.12–0.17). FB-W measured higher than paired FB-IO (mean bias 12.5%; 95% CI 11.6–13.4%) with wide 95% limits of agreement (− 15.4–40.4%).
Conclusions
Weighing neonates early after cardiac surgery is uncommon, with significant practice variation among centers. Patients with increased severity of illness are less likely to be weighed. FB-W and FB-IO have weak correlation, and further study is needed to determine which cumulative FB metric most associates with adverse outcomes.
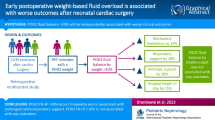
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information.




Similar content being viewed by others
References
Hassinger AB, Wald EL, Goodman DM (2014) Early postoperative fluid overload precedes acute kidney injury and is associated with higher morbidity in pediatric cardiac surgery patients. Pediatr Crit Care Med 15:131–138. https://doi.org/10.1097/PCC.0000000000000043
Hazle MA, Gajarski RJ, Yu S, Donohue J, Blatt NB (2013) Fluid overload in infants following congenital heart surgery. Pediatr Crit Care Med 14:44–49. https://doi.org/10.1097/PCC.0b013e3182712799
Seguin J, Albright B, Vertullo L, Lai P et al (2014) Extent, risk factors, and outcome of fluid overload after pediatric heart surgery. Crit Care Med 42:2591–2599
Lex DJ, Toth R, Czobor NR, Alexander SI et al (2016) Fluid overload is associated with higher mortality and morbidity in pediatric patients undergoing cardiac surgery. Pediatr Crit Care Med 17:307–314
Wilder NS, Yu S, Donohue JE, Goldberg CS, Blatt NB (2016) Fluid overload is associated with late poor outcomes in neonates following cardiac surgery. Pediatr Crit Care Med 17:420–427
Mah K, Hao S, Sutherland S, Kwiatkowski DM et al (2018) Fluid overload independent of acute kidney injury predicts poor outcomes in neonates following congenital heart surgery. Pediatr Nephrol 33:511–520. https://doi.org/10.1007/s00467-017-3818-x
Selewski DT, Cornell TT, Heung M, Troost JP et al (2014) Validation of the KDIGO acute kidney injury criteria in a pediatric critical care population. Intensive Care Med 40:1481–1488. https://doi.org/10.1007/s00134-014-3391-8
Selewski DT, Cornell TT, Blatt NB, Han YY et al (2012) Fluid overload and fluid removal in pediatric patients on extracorporeal membrane oxygenation requiring continuous renal replacement therapy. Crit Care Med 40:2694–2699
Rajalingam Y, Tourney S, McFarlane HJ (2001) Insensible fluid loss during cardiac surgery. Crit Care 5:2. https://doi.org/10.1186/cc1434
Young R (2012) Perioperative fluid and electrolyte management in cardiac surgery: a review. J Extracorpor Technol 44:20–26
Selewski DT, Charlton JR, Jetton JG, Guillet R et al (2015) Neonatal acute kidney injury. Pediatrics 136:e463–e473. https://doi.org/10.1542/peds.2014-3819
Starr MC, Charlton JR, Guillet R, Reidy K, Tipple TE, Jetton JG, Kent AL, Abitbol CL, Ambalavanan N, Mhanna MJ, Askenazi DJ, Selewski DT, Harer MW, Board NKC (2021) Advances in neonatal acute kidney injury. Pediatrics 148:e2021051220. https://doi.org/10.1542/peds.2021-051220
Testani JM, Brisco MA, Kociol RD, Jacoby D et al (2015) Substantial discrepancy between fluid and weight loss during acute decompensated heart failure treatment. Am J Med 128:776–783. https://doi.org/10.1016/j.amjmed.2014.12.020
Gist KM, Blinder JJ, Bailly D, Borasino S et al (2019) Neonatal and Paediatric Heart and Renal Outcomes Network: design of a multi-centre retrospective cohort study. Cardiol Young 29:511–518. https://doi.org/10.1017/S1047951119000210
Bates D, Mächler M, Bolker BM, Walker SC (2015) Fitting linear mixed-effects models using lme4. J Stat Softw 67:1–48. https://doi.org/10.18637/jss.v067.i01
Datta D 2017 blandr: a Bland-Altman method comparison package for R. https://github.com/deepankardatta/blandr
Selewski DT, Akcan-Arikan A, Bonachea EM, Gist KM et al (2019) The impact of fluid balance on outcomes in critically ill near-term/term neonates: a report from the AWAKEN study group. Pediatr Res 85:79–85. https://doi.org/10.1038/s41390-018-0183-9
Bailly DK, Alten JA, Gist KM, Mah KE et al (2022) Fluid accumulation after neonatal congenital cardiac operation: clinical implications and outcomes. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2021.12.078
Gaies M, Cooper DS, Tabbutt S, Schwartz SM et al (2015) Collaborative quality improvement in the cardiac intensive care unit: development of the Paediatric Cardiac Critical Care Consortium (PC4). Cardiol Young 25:951–957. https://doi.org/10.1017/S1047951114001450
Acknowledgements
The authors wish to acknowledge the data collection teams at all of the participating centers.
NEPHRON Investigators (Contributing authors)
The following individuals served as collaborators and site investigators for the NEPHRON study and are collaborators on this manuscript and should be indexed in PubMed as collaborators on this manuscript:
Parthak Prodhan, MDa, Xiomara Garcia, MDa, Shannon Ramer, BSN, RNCa, Mindy Albertson, RNa, Michael Gaies, MD, MPH, MSb, David S. Cooper, MD, MPHb, Zahidee Rodriquez, MDb, Mary Lukacsb, Dominic Zanaboni, MDc, Joan Sanchez de Toledo, MD, PhDd, Yuliya A. Domnina, MDd, Lucas Saenz, MDd, Tracy Baust, BAd, Jane Kluck, RN, BSNe, Linda Duncan, RN, BSNe, Joshua D. Koch, MDf, Joshua Freytagg, Amanda Sammonsg, Hideat Abrahag, John Butcherg, Jun Sasaki, MDh, Rebecca A. Bertrandt, MDi, Jason R. Buckley, MDj, Luke Schroeder, MDj, Aanish Raees, MBBSk, Lisa J. Sosa, ARNPl, Natasha S. Afonso, MD, MPHm, Erika R. O’Neal, MDm, Javier J. Lasa, MDm, Patrick A. Phillipsn, Amy Ardisanao, Kim Gonzalezo, Tammy Domano, Suzanne Vierso, Wenying Zhang, MSp, Kristal M. Hock, MSN, RN, CNLq, Santiago Borasino, MD, MPHq, Joshua J. Blinder, MDr
aArkansas Children’s Hospital, University of Arkansas for Medical Sciences, Little Rock, Arkansas; bDivision of Pediatric Cardiology, The Heart Institute, Department of Pediatrics, Cincinnati Children’s Hospital Medical Center, University of Cincinnati College of Medicine, Cincinnati, Ohio; cDivision of Cardiac Critical Care Medicine, Department of Anesthesia/Critical Care, Children’s Hospital of Philadelphia, University of Pennsylvania Perelman School of Medicine, Philadelphia, Pennsylvania; dDepartment of Critical Care Medicine and Pediatrics, UMPC Children’s Hospital of Pittsburg, University of Pittsburg School of Medicine, Pittsburg, Pennsylvania; eChildren’s Hospital of Wisconsin, Milwaukee, Wisconsin; fDivision of Critical Care Medicine, Department of Pediatrics, Children’s Medical Center of Dallas, University of Texas Southwestern Medical School, Dallas, Texas; gCincinnati Children’s Hospital Medical Center, Cincinnati, Ohio; hDivision of Cardiac Critical Care Medicine, Nicklaus Children’s Hospital, Miami, Florida; iDivision of Critical Care, Department of Pediatrics, Children’s Wisconsin, Medical College of Wisconsin, Milwaukee, Wisconsin; jMedical University of South Carolina Children’s Hospital, Charleston, South Carolina; kMonroe Carell Jr. Children’s Hospital at Vanderbilt, Vanderbilt, Tennessee; lNicklaus Children’s Hospital, Miami, Florida; mPediatric Critical Care, Texas Children’s Hospital, Baylor College of Medicine, Houston, Texas; nChildren’s of Alabama, University of Alabama at Birmingham, Birmingham, Alabama; oCS Mott Children’s Hospital, University of Michigan, Ann Arbor, Michigan; pCenter for Health Outcomes and Policy, University of Michigan, Ann Arbor, Michigan; qSection of Cardiac Critical Care Medicine, Department of Pediatric Cardiology, University of Alabama at Birmingham, Birmingham, Alabama; rLucile Packard Children’s Hospital Stanford, Palo Alto, California.
Funding
This study is financially supported by Castin’ ‘N Catchin’ Charity Organization and Cincinnati Children’s Hospital Medical Center Heart Institute Research Core.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Neumayr, T.M., Alten, J.A., Bailly, D.K. et al. Assessment of fluid balance after neonatal cardiac surgery: a description of intake/output vs. weight-based methods. Pediatr Nephrol 38, 1355–1364 (2023). https://doi.org/10.1007/s00467-022-05697-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05697-w