Abstract
Background
Children with chronic kidney disease (CKD) are at risk for cognitive dysfunction. The aim of this study was to investigate associations between executive functions (EF), anemia, and iron deficiency.
Methods
A total of 688 children > 6 years of age enrolled in the Chronic Kidney Disease in Children (CKiD) study who underwent evaluation for EF were included. Hemoglobin (Hgb) was characterized as low (1st–5th percentile) or very low (< 1st percentile) compared to normative values for age, sex, and race irrespective of erythropoiesis-stimulating agent (ESA) usage. Longitudinal analysis was conducted using consecutive visit pairs, with anemia status defined as new onset, resolved, or persistent. Linear mixed models with random intercept were used and adjusted for key covariates.
Results
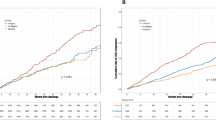
Anemia was present in 41% of children, and median Hgb was 11.8 gm/dl. New onset anemia was associated with lower digit span total score (− 0.75, 95% CI − 1.36, − 0.15, p = 0.01). Persistent anemia was associated with lower scores on color-word inhibition/switching (β = − 0.98; 95% CI − 1.78, − 0.18, p = 0.02). Errors of omission were significantly higher (worse) in those with persistent anemia (β = 2.67, 95% CI 0.18, 5.17, p = 0.04). Very low Hgb levels were significantly associated with lower color-word inhibition/switching scores (β = − 1.33, 95% CI − 2.16, − 0.51; p = 0.002). Anemia and low GFR were associated with lower category fluency scores compared to non-anemic subjects with higher GFR (β = − 1.09, 95% CI − 2.09, − 0.10, p = 0.03).
Conclusions
The presence of anemia, in addition to its severity and duration in children with CKD, is associated with poorer scores on select measures of EF.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
References
Johnson RJ, Warady BA (2013) Long-term neurocognitive outcomes of patients with end-stage renal disease during infancy. Pediatr Nephrol 28:1283–1291
Warady BA, Belden B, Kohaut E (1999) Neurodevelopmental outcome of children initiating peritoneal dialysis in early infancy. Pediatr Nephrol 13:759–765
Mendley SR, Matheson MB, Shinnar S, Lande MB, Gerson AC, Butler RW, Warady BA, Furth SL, Hooper SR (2015) Duration of chronic kidney disease reduces attention and executive function in pediatric patients. Kidney Int 87:800–806
Gipson DS, Hooper SR, Duquette PJ, Wetherington CE, Stellwagen KK, Jenkins TL, Ferris ME (2006) Memory and executive functions in pediatric chronic kidney disease. Child Neuropsychol 12:391–405. https://doi.org/10.1080/09297040600876311
Hooper SR, Johnson RJ, Gerson AC, Lande MB, Shinnar S, Harshman LA, Kogon AJ, Matheson M, Bartosh S, Carlson J, Warady BA, Furth SL (2022) Overview of the findings and advances in the neurocognitive and psychosocial functioning of mild to moderate pediatric CKD: perspectives from the Chronic Kidney Disease in Children (CKiD) cohort study. Pediatr Nephrol 37:765–775
Harshman LA, Johnson RJ, Matheson MB, Kogon AJ, Shinnar S, Gerson AC, Warady BA, Furth SL, Hooper SR (2019) Academic achievement in children with chronic kidney disease: a report from the CKiD cohort. Pediatr Nephrol 34:689–696
Chen K, Didsbury M, van Zwieten A, Howell M, Kim S, Tong A, Howard K, Nassar N, Barton B, Lah S, Lorenzo J, Strippoli G, Palmer S, Teixeira-Pinto A, Mackie F, McTaggart S, Walker A, Kara T, Craig JC, Wong G (2018) Neurocognitive and educational outcomes in children and adolescents with CKD: a systematic review and meta-analysis. Clin J Am Soc Nephrol 13:387–397
Hooper SR, Gerson AC, Butler RW, Gipson DS, Mendley SR, Lande MB, Shinnar S, Wentz A, Matheson M, Cox C, Furth SL, Warady BA (2011) Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin J Am Soc Nephrol 6:1824–1830. https://doi.org/10.2215/CJN09751110
Lande MB, Gerson AC, Hooper SR, Cox C, Matheson M, Mendley SR, Gipson DS, Wong C, Warady BA, Furth SL, Flynn JT (2011) Casual blood pressure and neurocognitive function in children with chronic kidney disease: a report of the children with chronic kidney disease cohort study. Clin J Am Soc Nephrol 6:1831–1837. https://doi.org/10.2215/CJN00810111
Ruebner RL, Laney N, Kim JY, Hartung EA, Hooper SR, Radcliffe J, Furth SL (2016) Neurocognitive dysfunction in children, adolescents, and young adults with CKD. Am J Kidney Dis 67:567–575
Verbitsky M, Kogon AJ, Matheson M, Hooper SR, Wong CS, Warady BA, Furth SL, Gharavi AG (2017) Genomic disorders and neurocognitive impairment in pediatric CKD. J Am Soc Nephrol 28:2303–2309
Atkinson MA, Martz K, Warady BA, Neu AM (2010) Risk for anemia in pediatric chronic kidney disease patients: a report of NAPRTCS. Pediatr Nephrol 25:1699–1706
Staples AO, Wong CS, Smith JM, Gipson DS, Filler G, Warady BA, Martz K, Greenbaum LA (2009) Anemia and risk of hospitalization in pediatric chronic kidney disease. Clin J Am Soc Nephrol 4:48–56
Walter T, De Andraca I, Chadud P, Perales CG (1989) Iron deficiency anemia: adverse effects on infant psychomotor development. Pediatrics 84:7–17
Marcus WL (1992) Development of infants with iron deficiency. N Engl J Med 326:575 (author reply 575-576)
Lozoff B, Jimenez E, Wolf AW (1991) Long-term developmental outcome of infants with iron deficiency. N Engl J Med 325:687–694
Marsh JT, Brown WS, Wolcott D, Carr CR, Harper R, Schweitzer SV, Nissenson AR (1991) rHuEPO treatment improves brain and cognitive function of anemic dialysis patients. Kidney Int 39:155–163
Nissenson AR (1992) Epoetin and cognitive function. Am J Kidney Dis 20:21–24
Stivelman JC (2000) Benefits of anaemia treatment on cognitive function. Nephrol Dial Transplant 15(Suppl 3):29–35
Singh NP, Sahni V, Wadhwa A, Garg S, Bajaj SK, Kohli R, Agarwal SK (2006) Effect of improvement in anemia on electroneurophysiological markers (P300) of cognitive dysfunction in chronic kidney disease. Hemodial Int 10:267–273
Slickers J, Duquette P, Hooper S, Gipson D (2007) Clinical predictors of neurocognitive deficits in children with chronic kidney disease. Pediatr Nephrol 22:565–572
Furth SL, Cole SR, Moxey-Mims M, Kaskel F, Mak R, Schwartz G, Wong C, Muñoz A, Warady BA (2006) Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin J Am Soc Nephrol 1:1006–1015
Pierce CB, Muñoz A, Ng DK, Warady BA, Furth SL, Schwartz GJ (2021) Age- and sex-dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int 99:948–956
Carlson J, Gerson AC, Matheson MB, Manne S, Warady BA, Hooper SR, Lande M, Harshman LA, Johnson RJ, Shinnar S, Kogon AJ, Furth S (2020) A longitudinal analysis of the effect of anemia on health-related quality of life in children with mild-to-moderate chronic kidney disease. Pediatr Nephrol 35:1659–1667
Amaral S, Hwang W, Fivush B, Neu A, Frankenfield D, Furth S (2006) Association of mortality and hospitalization with achievement of adult hemoglobin targets in adolescents maintained on hemodialysis. J Am Soc Nephrol 17:2878–2885
Warady BA, Ho M (2003) Morbidity and mortality in children with anemia at initiation of dialysis. Pediatr Nephrol 18:1055–1062
Idjradinata P, Pollitt E (1993) Reversal of developmental delays in iron-deficient anaemic infants treated with iron. Lancet 341:1–4
Walter T (2003) Effect of iron-deficiency anemia on cognitive skills and neuromaturation in infancy and childhood. Food Nutr Bull 24:S104-110
Burden MJ, Westerlund AJ, Armony-Sivan R, Nelson CA, Jacobson SW, Lozoff B, Angelilli ML, Jacobson JL (2007) An event-related potential study of attention and recognition memory in infants with iron-deficiency anemia. Pediatrics 120:e336-345
Hooper SR, Gerson AC, Johnson RJ, Mendley SR, Shinnar S, Lande MB, Matheson MB, Gipson DS, Morgenstern B, Warady BA, Furth SL (2016) Neurocognitive, social-behavioral, and adaptive functioning in preschool children with mild to moderate kidney disease. J Dev Behav Pediatr 37:231–238. https://doi.org/10.1097/DBP0000000000000267
Choi S, O’Neil SH, Joshi AA, Li J, Bush AM, Coates TD, Leahy RM, Wood JC (2019) Anemia predicts lower white matter volume and cognitive performance in sickle and non-sickle cell anemia syndrome. Am J Hematol 94:1055–1065
Petranovic D, Batinac T, Petranovic D, Ruzic A, Ruzic T (2008) Iron deficiency anaemia influences cognitive functions. Med Hypotheses 70:70–72
KDIGO (2012) Anemia work group KDIGO clinical practice guideline for anemia in chronic kidney disease. Kidney Int Suppl 2(4):279–335
Besarab A, Bolton WK, Browne JK, Egrie JC, Nissenson AR, Okamoto DM, Schwab SJ, Goodkin DA (1998) The effects of normal as compared with low hematocrit values in patients with cardiac disease who are receiving hemodialysis and epoetin. N Engl J Med 339:584–590
Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, Reddan D (2006) Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 355:2085–2098
Pfeffer MA, Burdmann EA, Chen CY, Cooper ME, de Zeeuw D, Eckardt KU, Feyzi JM, Ivanovich P, Kewalramani R, Levey AS, Lewis EF, McGill JB, McMurray JJ, Parfrey P, Parving HH, Remuzzi G, Singh AK, Solomon SD, Toto R (2009) A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N Engl J Med 361:2019–2032
Rheault MN, Molony JT, Nevins T, Herzog CA, Chavers BM (2017) Hemoglobin of 12 g/dl and above is not associated with increased cardiovascular morbidity in children on hemodialysis. Kidney Int 91:177–182
Acknowledgements
Data in this manuscript were collected by the CKiD prospective cohort study with clinical coordinating centers (principal investigators) at Children’s Mercy Hospital and the University of Missouri–Kansas City (Dr. Bradley Warady) and the Children’s Hospital of Philadelphia (Dr. Susan Furth), the Central Biochemistry Laboratory (Dr. George Schwartz) at the University of Rochester Medical Center, and the data coordinating center (Drs. Alvaro Muñoz and Derek Ng) at the Johns Hopkins Bloomberg School of Public Health. The CKiD website is located at https://statepi.jhsph.edu/ckid, and a list of CKiD collaborators can be found at https://statepi.jhsph.edu/ckid/site-investigators/. Please refer to the supplemental document which contains the list of the site principal investigators.
Funding
The CKiD Study is supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases, with additional funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and the National Heart, Lung, and Blood Institute (U01-DK-66143, U01-DK-66174, U24-DK-082194, U24-DK-66116). The CKiD website is located at https://statepi.jhsph.edu/ckid and a list of CKiD collaborators can be found at https://statepi.jhsph.edu/ckid/site-investigators/.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Singh, N.S., Johnson, R.J., Matheson, M.B. et al. A longitudinal analysis of the effect of anemia on executive functions in children with mild to moderate chronic kidney disease. Pediatr Nephrol 38, 829–837 (2023). https://doi.org/10.1007/s00467-022-05682-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05682-3