Abstract
Background
Elevated serum uric acid concentration is a risk factor for CKD progression. Its change over time and association with CKD etiology and concomitant changes in estimated glomerular filtration rate (eGFR) in children and adolescents are unknown.
Methods
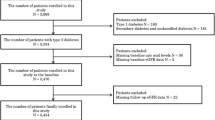
Longitudinal study of 153 children/adolescents with glomerular (G) and 540 with non-glomerular (NG) etiology from the CKD in Children (CKiD) study. Baseline serum uric acid, change in uric acid and eGFR over time, CKD etiology, and comorbidities were monitored. Adjusted linear mixed-effects regression models quantified the relationship between within-person changes in uric acid and concurrent within-person changes in eGFR.
Results
Participants with stable uric acid over follow-up had CKD progression which became worse for increased baseline uric acid (average annual percentage changes in eGFR were − 1.4%, − 7.7%, and − 14.7% in those with G CKD with baseline uric acid < 5.5 mg/dL, 5.5 − 7.5 mg/dL, and > 7.5 mg/dL, respectively; these changes were − 1.4%, − 4.1%, and − 8.6% in NG CKD). Each 1 mg/dL increase in uric acid over follow-up was independently associated with significant concomitant eGFR decreases of − 5.7% (95%CI − 8.4 to − 3.0%) (G) and − 5.1% (95%CI − 6.3 to − 4.0%) (NG) for those with baseline uric acid < 5.5 mg/dL and − 4.3% (95%CI − 6.8 to − 1.6%) (G) and − 3.3% (95%CI − 4.1 to − 2.6%) (NG) with baseline uric acid between 5.5 and 7.5 mg/dL.
Conclusions
Higher uric acid levels and increases in uric acid over time are risk factors for more severe progression of CKD in children and adolescents.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information.



Similar content being viewed by others
References
Oh TR, Choi HS, Kim CS, Bae EH, Ma SK, Sung SA, Kim YS, Oh KH, Ahn C, Kim SW (2019) Hyperuricemia has increased the risk of progression of chronic kidney disease: propensity score matching analysis from the KNOW-CKD study. Sci Rep 9:6681
Galan I, Goicoechea M, Quiroga B, Macías N, Santos A, García de Vinuesa MS, Verdalles Ú, Cedeño S, Verde E, Pérez de José A, García A, Luño J (2018) Hyperuricemia is associated with progression of chronic kidney disease in patients with reduced functioning kidney mass. Nefrologia 38:73–78
Li L, Yang C, Zhao Y, Zeng X, Liu F, Fu P (2014) Is hyperuricemia an independent risk factor for new-onset chronic kidney disease?: a systematic review and meta-analysis based on observational cohort studies. BMC Nephrol 15:122
See LC, Kuo CF, Chuang FH, Shen YM, Ko YS, Chen YM, Yu KH (2011) Hyperuricemia and metabolic syndrome: associations with chronic kidney disease. Clin Rheumatol 30:323–330
Toda A, Ishizaka Y, Tani M, Yamakado M (2014) Hyperuricemia is a significant risk factor for the onset of chronic kidney disease. Nephron Clin Pract 126:33–38
Pilemann-Lyberg S, Hansen TW, Tofte N, Winther SA, Theilade S, Ahluwalia TS, Rossing P (2019) Uric acid is an independent risk factor for decline in kidney function, cardiovascular events, and mortality in patients with type 1 diabetes. Diabetes Care 42:1088–1094
Ye M, Hu K, Jin J, Wu D, Hu P, He Q (2018) The association between time-mean serum uric acid levels and the incidence of chronic kidney disease in the general population: a retrospective study. BMC Nephrol 19:190
Johnson RJ, Bakris GL, Borghi C, Chonchol MB, Feldman D, Lanaspa MA, Merriman TR, Moe OW, Mount DB, Lozada LG, Stahl E, Weiner DE, Chertow GM (2018) Hyperuricemia, acute and chronic kidney disease, hypertension, and cardiovascular disease: report of a scientific workshop organized by the National Kidney Foundation. Am J Kidney Dis 71:851–865
Srivastava A, Kaze AD, McMullan CJ, Isakova T, Waikar SS (2018) Uric acid and the risks of kidney failure and death in individuals with CKD. Am J Kidney Dis 71:362–370
Zhu P, Liu Y, Han L, Xu G, Ran JM (2014) Serum uric acid is associated with incident chronic kidney disease in middle-aged populations: a meta-analysis of 15 cohort studies. PLoS One 9:e100801
Iseki K, Ikemiya Y, Inoue T, Iseki C, Kinjo K, Takishita S (2004) Significance of hyperuricemia as a risk factor for developing ESRD in a screened cohort. Am J Kidney Dis 44:642–650
Obermayr RP, Temml C, Gutjahr G, Knechtelsdorfer M, Oberbauer R, Klauser-Braun R (2008) Elevated uric acid increases the risk for kidney disease. J Am Soc Nephrol 19:2407–2413
Ben-Dov IZ, Kark JD (2011) Serum uric acid is a GFR-independent long-term predictor of acute and chronic renal insufficiency: the Jerusalem Lipid Research Clinic cohort study. Nephrol Dial Transplant 26:2558–2566
Tsai CW, Lin SY, Kuo CC, Huang CC (2017) Serum uric acid and progression of kidney disease: a longitudinal analysis and mini-review. PLoS One 12:e0170393
Rodenbach KE, Schneider MF, Furth SL, Moxey-Mims MM, Mitsnefes MM, Weaver DJ, Warady BA, Schwartz GJ (2015) Hyperuricemia and progression of CKD in children and adolescents: the chronic kidney disease in children (CKiD) cohort study. Am J Kidney Dis 66:984–992
Tsuji T, Ohishi K, Takeda A, Goto D, Sato T, Ohashi N, Fujigaki Y, Kato A, Yasuda H (2018) The impact of serum uric acid reduction on renal function and blood pressure in chronic kidney disease patients with hyperuricemia. Clin Exp Nephrol 22:1300–1308
Tsuruta Y, Mochizuki T, Moriyama T, Itabashi M, Takei T, Tsuchiya K, Nitta K (2014) Switching from allopurinol to febuxostat for the treatment of hyperuricemia and renal function in patients with chronic kidney disease. Clin Rheumatol 33:1643–1648
Sakai Y, Otsuka T, Ohno D, Murasawa T, Sato N, Tsuruoka S (2014) Febuxostat for treating allopurinol-resistant hyperuricemia in patients with chronic kidney disease. Ren Fail 36:225–231
Liu X, Liu K, Sun Q, Wang Y, Meng J, Xu Z, Shi Z (2018) Efficacy and safety of febuxostat for treating hyperuricemia in patients with chronic kidney disease and in renal transplant recipients: a systematic review and meta-analysis. Exp Ther Med 16:1859–1865
Chou HW, Chiu HT, Tsai CW, Ting IW, Yeh HC, Huang HC, Kuo CC (2018) Comparative effectiveness of allopurinol, febuxostat and benzbromarone on renal function in chronic kidney disease patients with hyperuricemia: a 13-year inception cohort study. Nephrol Dial Transplant 33:1620–1627
Badve SV, Pascoe EM, Tiku A, Boudville N, Brown FG, Cass A, Clarke P, Dalbeth N, ODay R, de Zoysa JR, Douglas B, Faull R, Harris DC, Hawley CM, Jones GRD, Kanellis J, Palmer SC, Perkovic V, Rangan GK, Reidlinger D, Robison L, Walker RJ, Walters G, Johnson DW, CKD-FIX Study Investigators (2020) Effects of allopurinol on the progression of chronic kidney disease. N Engl J Med 382:2504–2513
Doria A, Galecki AT, Spino C, Pop-Busui R, Cherney DZ, Lingvay I, Parsa A, Rossing P, Sigal RJ, Afkarian M, Aronson R, Caramori ML, Crandall JP, de Boer IH, Elliott TG, Goldfine AB, Haw JS, Hirsch IB, Karger AB, Maahs DM, McGill JB, Molitch ME, Perkins BA, Polsky S, Pragnell M, Robiner WN, Rosas SE, Senior P, Tuttle KR, Umpierrez GE, Wallia Am Weinstock RS, Wu C, Mauer M, PERL Study Group (2020) Serum urate lowering with allopurinol and kidney function in type 1 diabetes. N Engl J Med 382:2493–2503
Furth SL, Abraham AG, Jerry-Fluker J, Schwartz GJ, Benfied M, Kaskel F, Wong C, Mak RH, Moxey-Mims M, Warady BA (2011) Metabolic abnormalities, cardiovascular disease risk factors, and GFR decline in children with chronic kidney disease. Clin J Am Soc Nephrol 6:2132–2140
Pierce CB, Muñoz A, Ng DK, Warady BA, Furth SL, Schwartz GJ (2021) Age- and sex- dependent clinical equations to estimate glomerular filtration rates in children and young adults with chronic kidney disease. Kidney Int 99:948–956
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK, Gidding SS, Goodwin C, Leu MG, Powers ME, Rea C, Samuels J, Simasek M, Thaker VV, Urbina EM, SUBCOMMITTEE ON SCREENING AND MANAGEMENT OF HIGH BLOOD PRESSURE IN CHILDREN
Pierce CB, Cox C, Saland JM, Furth SL, Muñoz A (2011) Methods for characterizing differences in longitudinal glomerular filtration rate changes between children with glomerular chronic kidney disease and those with nonglomerular chronic kidney disease. Am J Epidemiol 174:604–612
Ng DK, Portale AA, Furth SL, Warady BA, Munoz A (2018) Time-varying coefficient of determination to quantify the explanatory power of biomarkers on longitudinal GFR among children with chronic kidney disease. Ann Epidemiol 28:549–556
Schneider MF, Muñoz A, Ku E, Warady BA, Furth SL, Schwartz GJ (2021) Estimation of albumin-creatinine ratio from protein-creatinine ratio in urine of children and adolescents with CKD. Am J Kidney Dis 77:824–827
Repetto HA (2005) Long-term course and mechanisms of progression of renal disease in hemolytic uremic syndrome. Kidney int Suppl 97:S102-106
Spizzirri FD, Rahman RC, Bibiloni N, Ruscasso JD, Amoreo OR (1997) Childhood hemolytic uremic syndrome in Argentina: long-term follow-up and prognostic features. Pediatr Nephrol 11:156–160
Caletti MG, Lejarraga H, Kelmansky D, Missoni M (2004) Two different therapeutic regimes in patients with sequelae of hemolytic-uremic syndrome. Pediatr Nephrol 19:1148–1152
Ng DK, Matheson MB, Warady BA, Mendley SR, Furth SL, Muñoz A (2019) Incidence of initial renal replacement therapy over the course of kidney disease in children. Am J Epidemiol 188:2156–2164
Saland JM, Kupferman JC, Pierce CB, Flynn JT, Mitsnefes MM, Warady BA, Furth SL (2019) Change in dyslipidemia with declining glomerular filtration rate and increasing proteinuria in children with CKD. Clin J Am Soc Nephrol 14:1711–1718
Chung TT, Yu KH, Kuo CF, Luo SF, Chiou MJ, Lan WC, Chen JS, Tseng WY, Hsieh AH, Wang LC (2019) Impact of urate-lowering drugs on the progression and recovery from chronic kidney disease among gout patients. Arthritis Res Ther 21:210
Liu X, Zhai T, Ma R, Luo C, Wang H, Liu L (2018) Effects of uric acid-lowering therapy on the progression of chronic kidney disease: a systematic review and meta-analysis. Ren Fail 40:289–297
Sampson AL, Singer RF, Walters GD (2017) Uric acid lowering therapies for preventing or delaying the progression of chronic kidney disease. Cochrane Database Syst Rev 10:CD009460
Sanchez-Lozada LG, Tapia E, Soto V, Avila-Casado C, Franco M, Wessale JL, Zhao L, Johnson RJ (2008) Effect of febuxostat on the progression of renal disease in 5/6 nephrectomy rats with and without hyperuricemia. Nephron Physiol 108:69–78
Cheung KWK, van Groen BD, Spaans E, van Borselen MD, de Bruijn A, Simons-Oosterhuis Y, Tibboel D, Samson JN, Verdijk RM, Smeets B, Zhang L, Huang SM, Giacomini KM, de Wildt SN (2019) A comprehensive analysis of ontogeny of renal drug transporters: mRNA analyses, quantitative proteomics, and localization. Clin Pharmacol Ther 106:1083–1092
Sweeney DE, Vallon V, Rieg T, Wu W, Gallegos TF, Nigam SK (2011) Functional maturation of drug transporters in the developing, neonatal, and postnatal kidney. Mol Pharmacol 80:147–154
Passwell JH, Modan M, Brish M, Orda S, Boichis H (1974) Fractional excretion of uric acid in infancy and childhood. Index of tubular maturation. Arch Dis Child 49:878–882
Baldree LA, Stapleton FB (1990) Uric acid metabolism in children. Pediatr Clin North Am 37:391–418
Stiburkova B, Bleyer AJ (2012) Changes in serum urate and urate excretion with age. Adv Chronic Kidney Dis 19:372–376
Wilcox WD (1996) Abnormal serum uric acid levels in children. J Pediatr 128:731–741
Kubota M (2019) Hyperuricemia in children and adolescents: present knowledge and future directions. J Nutr Metab 2019:3480718
Kubota M, Nagai A, Tang L, Tokuda M (2011) Investigation on hyperuricemia in children with obesity or various pediatric disorders. Nucleosides Nucleotides Nucleic Acids 30:1051–1059
Suzuki Y, Sudo J (1987) Possible mechanism responsible for allopurinol-nephrotoxicity: lipid peroxidation and systems of producing- and scavenging oxygen radicals. Jpn J Pharmacol 45:271–279
Tan PK, Liu S, Gunic E, Miner JN (2017) Discovery and characterization of verinurad, a potent and specific inhibitor of URAT1 for the treatment of hyperuricemia and gout. Sci Rep 7:665
Acknowledgements
Data in this manuscript were collected by the Chronic Kidney Disease in children prospective cohort study (CKiD) with clinical coordinating centers (principal investigators) at Children’s Mercy Hospital and the University of Missouri—Kansas City (Bradley Warady, MD) and Children’s Hospital of Philadelphia (Susan Furth, MD, PhD), Central Biochemistry Laboratory (George Schwartz, MD) at the University of Rochester Medical Center, and data coordinating center (Alvaro Muñoz, PhD and Derek Ng, PhD) at the Johns Hopkins Bloomberg School of Public Health. The CKiD website is located at https://statepi.jhsph.edu/ckid and a list of CKiD site principal investigators can be found at https://statepi.jhsph.edu/ckid/site-investigators/. Please refer to the supplemental document which contains the list of the site principal investigators.
Funding
The CKiD Study is funded by the National Institute of Diabetes and Digestive and Kidney Diseases, with additional funding from the National Institute of Child Health and Human Development and the National Heart, Lung, and Blood Institute (U01-DK-66143, U01-DK66174, U24-DK-082194, U24-DK-66116).
Author information
Authors and Affiliations
Contributions
GJS: conceived and designed work, drafted and revised MS, and approved final version.
JLR: conducted the statistical analyses, drafted and revised MS, and approved final version.
SRH: revised MS and approved final version.
SLF: revised MS and approved final version.
DJW: revised MS and approved final version.
BAW: revised MS and approved final version.
MFS: designed work and conducted statistical analyses, drafted and revised MS, and approved final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schwartz, G.J., Roem, J.L., Hooper, S.R. et al. Longitudinal changes in uric acid concentration and their relationship with chronic kidney disease progression in children and adolescents. Pediatr Nephrol 38, 489–497 (2023). https://doi.org/10.1007/s00467-022-05620-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05620-3