Abstract
Background
The leading cause of advanced chronic kidney disease (CKD) in children is congenital anomalies of the kidney and urinary tract (CAKUT). However, the most appropriate parameters of biochemical urine analysis for detecting CAKUT with kidney dysfunction are not known.
Methods
The present observational study analyzed data on children with CAKUT (stage 2–4 CKD) and the general pediatric population obtained from school urine screenings. The sensitivity and specificity of urine alpha 1-microglobulin-, beta 2-microglobulin-, protein-, and the albumin-to-creatinine ratios (AMCR, BMCR, PCR, ACR, respectively) in detecting CAKUT with kidney dysfunction were compared with those of the conventional urine dipstick, and the most appropriate of these four parameters were evaluated.
Results
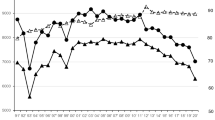
In total, 77 children with CAKUT and 1712 subjects in the general pediatric population fulfilled the eligibility criteria. Conventional dipstick urinalysis was insufficient due to its low sensitivity; even when the threshold of proteinuria was +/−, its sensitivity was only 29.7% for stage 2 and 44.1% for stage 3 CKD. Among the four parameters assessed, the AMCR and BMCR were adequate for detecting CAKUT in children with stage 3–4 CKD (the respective sensitivity and specificity of the AMCR for detecting CAKUT in stage 3 CKD was 79.4% and 97.5% while that of BMCR was 82.4% and 97.5%). These data were validated using national cohort data.
Conclusion
AMCR and BMCR are superior to dipstick urinalysis, PCR, and ACR in detecting CAKUT with kidney dysfunction, particularly stage 3 CKD. However, for AMCR, external validation is required.
Graphical Abstract
A higher resolution version of the Graphical abstract is available as Supplementary information



Similar content being viewed by others
Data availability
The first author and the corresponding author have the study data, which can be provided on reasonable request.
Code availability
Not applicable.
References
Toka HR, Toka O, Hariri A, Nguyen HT (2010) Congenital anomalies of kidney and urinary tract. Semin Nephrol 30:374–386
Becherucci F, Roperto RM, Materassi M, Romagnani P (2016) Chronic kidney disease in children. Clin Kidney J 9:583–591
Ishikura K, Uemura O, Ito S, Wada N, Hattori M, Ohashi Y, Hamasaki Y, Tanaka R, Nakanishi K, Kaneko T, Honda M, Pediatric CKD Study Group in Japan in conjunction with the Committee of Measures for Pediatric CKD of the Japanese Society of Pediatric Nephrology (2013) Pre-dialysis chronic kidney disease in children: results of a nationwide survey in Japan. Nephrol Dial Transplant 28:2345–2355
Hattori M, Sako M, Kaneko T, Ashida A, Matsunaga A, Igarashi T, Itami N, Ohta T, Gotoh Y, Satomura K, Honda M, Igarashi T (2015) End-stage renal disease in Japanese children: a nationwide survey during 2006–2011. Clin Exp Nephrol 19:933–938
Sanna-Cherchi S, Ravani P, Corbani V, Parodi S, Haupt R, Piaggio G, Innocenti ML, Somenzi D, Trivelli A, Caridi G, Izzi C, Scolari F, Mattioli G, Allegri L, Ghiggeri GM (2009) Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int 76:528–533
Wühl E, van Stralen KJ, Verrina E, Bjerre A, Wanner C, Heaf JG, Zurriaga O, Hoitsma A, Niaudet P, Palsson R, Ravani P, Jager KJ, Schaefer F (2013) Timing and outcome of renal replacement therapy in patients with congenital malformations of the kidney and urinary tract. Clin J Am Soc Nephrol 8:67–74
Murugapoopathy V, Gupta IR (2020) A primer on congenital anomalies of the kidneys and urinary tracts (CAKUT). Clin J Am Soc Nephrol 15:723–731
Furth SL, Pierce C, Hui WF, White CA, Wong CS, Schaefer F, Wühl E, Abraham AG, Warady BA, Chronic Kidney Disease in Children (CKiD), Effect of Strict Blood Pressure Control and ACE Inhibition on the Progression of CRF in Pediatric Patients (ESCAPE) Study Investigators (2018) Estimating time to ESRD in children with CKD. Am J Kidney Dis 71:783–792
Harambat J, van Stralen KJ, Kim JJ, Tizard EJ (2012) Epidemiology of chronic kidney disease in children. Pediatr Nephrol 27:363–373
Hodson EM, Willis NS, Craig JC (2012) Growth hormone for children with chronic kidney disease. Cochrane Database Syst Rev 2:CD003264
Chen K, Didsbury M, van Zwieten A, Howell M, Kim S, Tong A, Howard K, Nassar N, Barton B, Lah S, Lorenzo J, Strippoli G, Palmer S, Teixeira-Pinto A, Mackie F, McTaggart S, Walker A, Kara T, Craig JC, Wong G (2018) Neurocognitive and educational outcomes in children and adolescents with CKD: a systematic review and meta-analysis. Clin J Am Soc Nephrol 13:387–397
Seikaly MG, Salhab N, Gipson D, Yiu V, Stablein D (2006) Stature in children with chronic kidney disease: analysis of NAPRTCS database. Pediatr Nephrol 21:793–799
Rodig NM, McDermott KC, Schneider MF, Hotchkiss HM, Yadin O, Seikaly MG, Furth SL, Warady BA (2014) Growth in children with chronic kidney disease: a report from the Chronic Kidney Disease in Children Study. Pediatr Nephrol 29:1987–1995
Altemose KE, Kumar J, Portale AA, Warady BA, Furth SL, Fadrowski JJ, Atkinson MA (2018) Vitamin D insufficiency, hemoglobin, and anemia in children with chronic kidney disease. Pediatr Nephrol 33:2131–2136
Atkinson MA, Warady BA (2018) Anemia in chronic kidney disease. Pediatr Nephrol 33:227–238
Rees L (2016) Growth hormone therapy in children with CKD after more than two decades of practice. Pediatr Nephrol 31:1421–1435
Drube J, Wan M, Bonthuis M, Wühl E, Bacchetta J, Santos F, Grenda R, Edefonti A, Harambat J, Shroff R, Tönshoff B, Haffner D, European Society for Paediatric Nephrology Chronic Kidney Disease Mineral and Bone Disorders, Dialysis, and Transplantation Working Groups (2019) Clinical practice recommendations for growth hormone treatment in children with chronic kidney disease. Nat Rev Nephrol 15:577–589
Murakami M, Yamamoto H, Ueda Y, Murakami K, Yamauchi K (1991) Urinary screening of elementary and junior high-school children over a 13-year period in Tokyo. Pediatr Nephrol 5:50–53
Yanagihara T, Kuroda N, Hayakawa M, Yoshida J, Tsuchiya M, Yamauchi K, Murakami M, Fukunaga Y (2007) Epidemiology of school urinary screening over a 30 year period in Tokyo. Pediatr Int 49:570–576
Murakami M, Hayakawa M, Yanagihara T, Hukunaga Y (2005) Proteinuria screening for children. Kidney Int Suppl 94:S23–S27
Imai E, Yamagata K, Iseki K, Iso H, Horio M, Mkino H, Hishida A, Matsuo S (2007) Kidney disease screening program in Japan: history, outcome, and perspectives. Clin J Am Soc Nephrol 2:1360–1366
Kidney Disease: Improving Global Outcomes (KDIGO) CKD work group (2013) KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3:1–150
Houser M (1984) Assessment of proteinuria using random urine samples. J Pediatr 104:845–848
Jones CA, Francis ME, Eberhardt MS, Chavers B, Coresh J, Engelgau M, Kusek JW, Byrd-Holt D, Narayan KM, Herman WH, Jones CP, Salive M, Agodoa LY (2002) Microalbuminuria in the US population: third National Health and Nutrition Examination Survey. Am J Kidney Dis 39:445–459
Joyce E, Glasner P, Ranganathan S, Swiatecka-Urban A (2017) Tubulointerstitial nephritis: diagnosis, treatment, and monitoring. Pediatr Nephrol 32:577–587
Hettinga YM, Scheerlinck LM, Lilien MR, Rothova A, de Boer JH (2015) The value of measuring urinary β2-microglobulin and serum creatinine for detecting tubulointerstitial nephritis and uveitis syndrome in young patients with uveitis. JAMA Ophthalmol 133:140–145
Uemura O, Nagai T, Ishikura K, Ito S, Hataya H, Gotoh Y, Fujita N, Akioka Y, Kaneko T, Honda M (2014) Creatinine-based equation to estimate the glomerular filtration rate in Japanese children and adolescents with chronic kidney disease. Clin Exp Nephrol 18:626–633
Uemura O, Nagai T, Ishikura K, Ito S, Hataya H, Gotoh Y, Fujita N, Akioka Y, Kaneko T, Honda M (2014) Cystatin C-based equation for estimating glomerular filtration rate in Japanese children and adolescents. Clin Exp Nephrol 18:718–725
Yoshida J, Tsuchiya M, Tatsuma N, Murakami M (2003) Mass screening for early detection of congenital kidney and urinary tract abnormalities in infancy. Pediatr Int 45:142–149
Tsuchiya M, Hayashida M, Yanagihara T, Yoshida J, Takeda S, Tatsuma N, Tsugu H, Hino Y, Munakata E, Murakami M (2003) Ultrasound screening for renal and urinary tract anomalies in healthy infants. Pediatr Int 45:617–623
Uwaezuoke SN, Ayuk AC, Muoneke VU, Mbanefo NR (2018) Chronic kidney disease in children: using novel biomarkers as predictors of disease. Saudi J Kidney Dis Transpl 29:775–784
Bartoli F, Pastore V, Calè I, Aceto G, Campanella V, Lasalandra C, Magaldi S, Niglio F, Basile A, Cocomazzi R (2019) Prospective study on several urinary biomarkers as indicators of renal damage in children with CAKUT. Eur J Pediatr Surg 29:215–222
D'Amico G, Bazzi C (2003) Pathophysiology of proteinuria. Kidney Int 63:809–825
Hogg RJ (2009) Screening for CKD in children: a global controversy. Clin J Am Soc Nephrol 4:509–515
Acknowledgments
We confirm that the results presented in this article have not been published previously in their entirety or in part. The authors would like to thank all the hospitals, institutions, pediatricians, and the Tokyo Health Organization for their cooperation. The authors would also like to thank Katsumi Abe and Yoshihiko Morikawa for their assistance with coordinating and supervising data collection, and James Robert Valera for his assistance with editing this manuscript, and Yoshinobu Nagaoka, Ryoko Harada, Yuko Hamasaki, and all members of the Pediatric CKD Study Group in Japan in conjunction with the Committee of Measures for Pediatric CKD of the Japanese Society for Pediatric Nephrology for providing us with the data.
Funding
The present study was supported by a Health, Labour and Welfare Sciences Research Grant (H25-jisedai-ippan-003) and childhood-onset, rare and intractable kidney disease in Japan, research on rare and intractable diseases Health, Labour and Welfare Sciences Research Grants (20FC1028).
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception and design of the study; to the acquisition, analysis, and interpretation of the data; or to the drafting and critical revision of the manuscript for important intellectual content. RH conceptualized and designed the study and wrote the first draft. KK interpreted the data and reviewed and revised the manuscript. MH helped conceptualize and design the study, interpreted the data, and helped revise the manuscript. SO and TM helped conceptualize and design the study. MT, OU, KK, NW, and AO coordinated and supervised data collection at each site. KI also provided us with the data and critically reviewed the analyses and the manuscript. As the biostatistician, TK carried out the analyses and interpreted the data. Furthermore, all the authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by a central ethics board (Tokyo Metropolitan Children’s Medical Center approval number H25-33; Fussa Hospital approval number 1; and Tokyo Health Organization) before commencement.
Consent to participate
The study data were retrospective and based on information in the patients’ medical records and records of annual screenings. Informed consent was waived in accordance with the related guidelines. The study protocol was displayed publicly on the website of Tokyo Metropolitan Children’s Medical Center and Tokyo Health Organization in accordance with the guidelines.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hamada, R., Kikunaga, K., Kaneko, T. et al. Urine alpha 1-microglobulin-to-creatinine ratio and beta 2-microglobulin-to-creatinine ratio for detecting CAKUT with kidney dysfunction in children. Pediatr Nephrol 38, 479–487 (2023). https://doi.org/10.1007/s00467-022-05577-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05577-3