Abstract
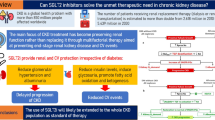
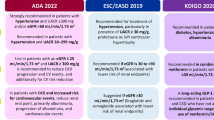
Chronic kidney disease (CKD) is a global public healthcare concern in the pediatric population, where glomerulopathies represent the second most common cause. Although classification and diagnosis of glomerulopathies still rely mostly on histopathological patterns, patient stratification should complement information supplied by kidney biopsy with clinical data and etiological criteria. Genetic determinants of glomerular injury are particularly relevant in children, with important implications for prognosis and treatment. Targeted therapies addressing the primary cause of the disease are available for a limited number of glomerular diseases. Consequently, in the majority of cases, the treatment of glomerulopathies is actually the treatment of CKD. The efficacy of the currently available strategies is limited, but new prospects evolve. Although the exact mechanisms of action are still under investigation, accumulating data in adults demonstrate the efficacy of sodium-glucose transporter 2 inhibitors (SGLT2i) in slowing the progression of CKD due to diabetic and non-diabetic kidney disease. SGLT2i has proved effective on other comorbidities, such as obesity, glycemic control, and cardiovascular risk that frequently accompany CKD. The use of SGLT2i is not yet approved in children. However, no pathophysiological clues theoretically exclude their application. The hallmark of pediatric CKD is the inevitable imbalance between the metabolic needs of a growing child and the functional capacity of a failing kidney to handle those needs. In this view, developing better strategies to address any modifiable progressor in kidney disease is mandatory, especially considering the long lifespan typical of the pediatric population. By improving the hemodynamic adaptation of the kidney and providing additional beneficial effects on the overall complications of CKD, SGLT2i is a candidate as a potentially innovative drug for the treatment of CKD and glomerular diseases in children.


Similar content being viewed by others
References
Becherucci F, Roperto RM, Materassi M, Romagnani P (2016) Chronic kidney disease in children. Clin Kidney J 9:583–591. https://doi.org/10.1093/ckj/sfw047
Romagnani P, Remuzzi G, Glassock R, Levin A et al (2017) Chronic kidney disease. Nat Rev Dis Primers 3:17088. https://doi.org/10.1038/nrdp.2017.88
Kula AJ, Somers MJG, American Society of Pediatric Nephrology (2021) Children with CKD are not little adults with CKD: pediatric considerations for the Advancing American Kidney Health Initiative. Clin J Am Soc Nephrol 16:470–472. https://doi.org/10.2215/CJN.11540720
Ingelfinger JR (2018) A disturbing legacy of childhood kidney disease. N Engl J Med 378:470–471. https://doi.org/10.1056/NEJMe1716499
Rheault MN, Wenderfer SE (2018) Evolving epidemiology of pediatric glomerular disease. Clin J Am Soc Nephrol 13:977–978. https://doi.org/10.2215/CJN.06220518
O’Shaughnessy MM, Hogan SL, Poulton CJ, Falk RJ et al (2017) Temporal and demographic trends in glomerular disease epidemiology in the Southeastern United States, 1986–2015. Clin J Am Soc Nephrol 12:614–623. https://doi.org/10.2215/CJN.10871016
Kopp JB, Anders HJ, Susztak K, Podestà MA et al (2020) Podocytopathies Nat Rev Dis Primers 6:68. https://doi.org/10.1038/s41572-020-0196-7
Landini S, Mazzinghi B, Becherucci F, Allinovi M et al (2020) Reverse phenotyping after whole-exome sequencing in steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol 15:89–100. https://doi.org/10.2215/CJN.06060519
Warejko JK, Tan W, Daga A, Schapiro D et al (2018) Whole exome sequencing of patients with steroid-resistant nephrotic syndrome. Clin J Am Soc Nephrol 13:53–62. https://doi.org/10.2215/CJN.04120417
Becherucci F, Landini S, Cirillo L, Mazzinghi B, Romagnani P (2020) Look alike, sound alike: phenocopies in steroid-resistant nephrotic syndrome. Int J Environ Res Public Health 17:8363. https://doi.org/10.3390/ijerph17228363
Wuttke M, Schaefer F, Wong CS, Köttgen A (2015) Genome-wide association studies in nephrology: using known associations for data checks. Am J Kidney Dis 65:217–222. https://doi.org/10.1053/j.ajkd.2014.09.019
Anders HJ, Peired AJ, Romagnani P (2020) SGLT2 inhibition requires reconsideration of fundamental paradigms in chronic kidney disease, ‘diabetic nephropathy’, IgA nephropathy and podocytopathies with FSGS lesions. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfaa329
Luyckx VA, Perico N, Somaschini M, Manfellotto D et al (2017) A developmental approach to the prevention of hypertension and kidney disease: a report from the Low Birth Weight and Nephron Number Working Group. Lancet 390:424–428. https://doi.org/10.1016/S0140-6736(17)30576-7
Khalsa DD, Beydoun HA, Carmody JB (2016) Prevalence of chronic kidney disease risk factors among low birth weight adolescents. Pediatr Nephrol 31:1509–1516. https://doi.org/10.1007/s00467-016-3384-7
Low Birth Weight and Nephron Number Working Group (2017) The impact of kidney development on the life course: a consensus document for action. Nephron 136:3–49. https://doi.org/10.1159/000457967
Ruggajo P, Svarstad E, Leh S, Marti HP, Reisæther AV, Vikse BE (2016) Low birth weight and risk of progression to end stage renal disease in IgA nephropathy–a retrospective registry-based cohort study. PLoS One 11:e0153819. https://doi.org/10.1371/journal.pone.0153819
Nada A, Jetton JG (2021) Pediatric onco-nephrology: time to spread the word-part II: long-term kidney outcomes in survivors of childhood malignancy and malignancy after kidney transplant. Pediatr Nephrol. https://doi.org/10.1007/s00467-021-05172-y
Panwar B, Hanks LJ, Tanner RM, Muntner P et al (2015) Obesity, metabolic health, and the risk of end-stage renal disease. Kidney Int 87:1216–1222. https://doi.org/10.1038/ki.2014.384
Perico N, Ruggenenti P, Remuzzi G (2017) ACE and SGLT2 inhibitors: the future for non-diabetic and diabetic proteinuric renal disease. Curr Opin Pharmacol 33:34–40. https://doi.org/10.1016/j.coph.2017.03.006
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group (2021) KDIGO 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int 100:S1–S276
Trautmann A, Vivarelli M, Samuel S, Gipson D et al (2020) IPNA clinical practice recommendations for the diagnosis and management of children with steroid-resistant nephrotic syndrome. Pediatr Nephrol 35:1529–1561. https://doi.org/10.1007/s00467-020-04519-1
de Zeeuw D, Agarwal R, Amdahl M, Audhya P et al (2010) Selective vitamin D receptor activation with paricalcitol for reduction of albuminuria in patients with type 2 diabetes (VITAL study): a randomised controlled trial. Lancet 376:1543–1551. https://doi.org/10.1016/S0140-6736(10)61032-X
Mann JF, Green D, Jamerson K, Ruilope LM et al (2010) Avosentan for overt diabetic nephropathy. J Am Soc Nephrol 21:527–535. https://doi.org/10.1681/ASN.2009060593
Wenzel RR, Littke T, Kuranoff S, Jürgens C et al (2009) Avosentan reduces albumin excretion in diabetics with macroalbuminuria. J Am Soc Nephrol 20:655–664. https://doi.org/10.1681/ASN.2008050482
Bakris GL, Agarwal R, Anker SD, Pitt B et al (2020) Effect of Finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med 383:2219–2229. https://doi.org/10.1056/NEJMoa2025845
Chin MP, Bakris GL, Block GA, Chertow GM et al (2018) Bardoxolone methyl improves kidney function in patients with chronic kidney disease stage 4 and type 2 diabetes: post-hoc analyses from bardoxolone methyl evaluation in patients with chronic kidney disease and type 2 diabetes study. Am J Nephrol 47:40–47. https://doi.org/10.1159/000486398
Panchapakesan U, Pollock C (2021) Organ protection beyond glycaemic control with SGLT2 inhibitors. Nat Rev Nephrol 17:223–224. https://doi.org/10.1038/s41581-020-00373-4
Zinman B, Wanner C, Lachin JM, Fitchett D et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 373:2117–2128. https://doi.org/10.1056/NEJMoa1504720
Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, Edwards R, Agarwal R, Bakris G, Bull S, Cannon CP, Capuano G, Chu P-L, de Zeeuw D, Greene T, Levin A, Pollock C, Wheeler DC, Yavin Y, Zhang H,Zinman B, Meininger G, Brenner BM, Mahaffey KW (2019) Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med 380:2295–2306. https://doi.org/10.1056/NEJMoa1811744
Oshima M, Neuen BL, Li J, Perkovic V, Charytan DM et al (2020) Early change in albuminuria with canagliflozin predicts kidney and cardiovascular outcomes: a post hoc analysis from the CREDENCE Trial. J Am Soc Nephrol 31:2925–2936. https://doi.org/10.1681/ASN.2020050723
Heerspink HJL, Jongs N, Chertow GM, Langkilde AM et al (2021) Effect of dapagliflozin on the rate of decline in kidney function in patients with chronic kidney disease with and without type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol 9:743–754. https://doi.org/10.1016/S2213-8587(21)00242-4
Jongs N, Greene T, Chertow GM, McMurray JJV et al (2021) Effect of dapagliflozin on urinary albumin excretion in patients with chronic kidney disease with and without type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol 9:755–766. https://doi.org/10.1016/S2213-8587(21)00243-6
Heerspink HJL, Stefánsson BV, Correa-Rotter R, Chertow GM et al (2020) Dapagliflozin in patients with chronic kidney disease. N Engl J Med 383:1436–1446. https://doi.org/10.1056/NEJMoa2024816
Heerspink HJL, Stefansson BV, Chertow GM, Correa-Rotter R et al (2020) Rationale and protocol of the Dapagliflozin And Prevention of Adverse outcomes in Chronic Kidney Disease (DAPA-CKD) randomized controlled trial. Nephrol Dial Transplant 35:274–282. https://doi.org/10.1093/ndt/gfz290
Wheeler DC, Stefansson BV, Batiushin M, Bilchenko O et al (2020) The dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) trial: baseline characteristics. Nephrol Dial Transplant 35:1700–1711. https://doi.org/10.1093/ndt/gfaa234
Wheeler DC, Toto RD, Stefánsson BV, Jongs N et al (2021) A pre-specified analysis of the DAPA-CKD trial demonstrates the effects of dapagliflozin on major adverse kidney events in patients with IgA nephropathy. Kidney Int 100:215–224. https://doi.org/10.1016/j.kint.2021.03.033
Rauen T, Eitner F, Fitzner C, Sommerer C, Zeier M, Otte B, Panzer U, Peters H, Benck U, Mertens PR, Kuhlmann U, Witzke O, Gross O, Vielhauer V, Mann JFE, Hilgers R-D, Floege J (2015) Intensive supportive care plus immunosuppression in IgA nephropathy. N Engl J Med 373:2225–2236. https://doi.org/10.1056/NEJMoa1415463
Lv J, Zhang H, Wong MG, Jardine MJ et al (2017) Effect of oral methylprednisolone on clinical outcomes in patients with IgA nephropathy: the TESTING randomized clinical trial. JAMA 318:432–442. https://doi.org/10.1001/jama.2017.9362
Rajasekeran H, Reich HN, Hladunewich MA, Cattran D et al (2018) Dapagliflozin in focal segmental glomerulosclerosis: a combined human-rodent pilot study. Am J Physiol Renal Physiol 314:F412–F422. https://doi.org/10.1152/ajprenal.00445.2017
Cherney DZI, Dekkers CCJ, Barbour SJ, Cattran D et al (2020) Effects of the SGLT2 inhibitor dapagliflozin on proteinuria in non-diabetic patients with chronic kidney disease (DIAMOND): a randomised, double-blind, crossover trial. Lancet Diabetes Endocrinol 8:582–593. https://doi.org/10.1016/S2213-8587(20)30162-5
Anker SD, Butler J, Filippatos G, Ferreira JP et al (2021) Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 385:1451–1461. https://doi.org/10.1056/NEJMoa2107038
Herrington WG, Preiss D, Haynes R, von Eynatten M et al (2018) The potential for improving cardio-renal outcomes by sodium-glucose co-transporter-2 inhibition in people with chronic kidney disease: a rationale for the EMPA-KIDNEY study. Clin Kidney J 11:749–761. https://doi.org/10.1093/ckj/sfy090
Miyata N, Zhang SL, Chan JSD (2021) The rationale and evidence for SGLT2 inhibitors as a treatment for nondiabetic glomerular disease. Glomerular Dis 1:21–33. https://doi.org/10.1159/000513659
Srinivasan Sridhar V, Ambinathan JPN, Kretzler M, Pyle LL, Bjornstad P et al (2019) NephRenal SGLT mRNA expression in human health and disease: a study in two cohorts. Am J Physiol Renal Physiol 317:F1224–F1230. https://doi.org/10.1152/ajprenal.00370.2019
Sen T, Heerspink HJL (2021) A kidney perspective on the mechanism of action of sodium glucose co-transporter 2 inhibitors. Cell Metab 33:732–739. https://doi.org/10.1016/j.cmet.2021.02.016
Brown RD, Turner AJ, Carlström M, Persson AE, Gibson KJ (2011) Tubuloglomerular feedback response in the prenatal and postnatal ovine kidney. Am J Physiol Renal Physiol 300:F1368–F1374. https://doi.org/10.1152/ajprenal.00019.2011
Deng A, Hammes JS, Thomson SC (2002) Hemodynamics of early tubuloglomerular feedback resetting during reduced proximal reabsorption. Kidney Int 62:2136–2143. https://doi.org/10.1046/j.1523-1755.2002.00682.x
Brenner BM, Mackenzie HS (1997) Nephron mass as a risk factor for progression of renal disease. Kidney Int Suppl 63:S124–S127
Cherney DZ, Perkins BA, Soleymanlou N, Maione M et al (2014) Renal hemodynamic effect of sodium-glucose cotransporter 2 inhibition in patients with type 1 diabetes mellitus. Circulation 129:587–597. https://doi.org/10.1161/CIRCULATIONAHA.113.005081
Kidokoro K, Cherney DZI, Bozovic A, Nagasu H et al (2019) Evaluation of glomerular hemodynamic function by empagliflozin in diabetic mice using in vivo imaging. Circulation 140:303–315. https://doi.org/10.1161/CIRCULATIONAHA.118.037418
Rajasekeran H, Lytvyn Y, Bozovic A, Lovshin JA et al (2017) Urinary adenosine excretion in type 1 diabetes. Am J Physiol Renal Physiol 313:F184–F191. https://doi.org/10.1152/ajprenal.00043.2017
Nosadini R, Semplicini A, Fioretto P, Lusiani L et al (1991) Sodium-lithium countertransport and cardiorenal abnormalities in essential hypertension. Hypertension 18:191–198. https://doi.org/10.1161/01.hyp.18.2.191
Chagnac A, Herman M, Zingerman B, Erman A et al (2008) Obesity-induced glomerular hyperfiltration: its involvement in the pathogenesis of tubular sodium reabsorption. Nephrol Dial Transplant 23:3946–3952. https://doi.org/10.1093/ndt/gfn379
Zingerman B, Herman-Edelstein M, Erman A, Bar Sheshet Itach S, Ori Y, Rozen-Zvi B, Gafter U, Chagnac A (2015) Effect of acetazolamide on obesity-induced glomerular hyperfiltration: a randomized controlled trial. PLoS One 10:e0137163. https://doi.org/10.1371/journal.pone.0137163
Onishi A, Fu Y, Patel R, Darshi M, Crespo-Masip M et al (2020) A role for tubular Na+/H+ exchanger NHE3 in the natriuretic effect of the SGLT2 inhibitor empagliflozin. Am J Physiol Renal Physiol 319:F712–F728. https://doi.org/10.1152/ajprenal.00264.2020
Wanner C, Heerspink HJL, Zinman B, Inzucchi SE et al (2018) Empagliflozin and kidney function decline in patients with type 2 diabetes: a slope analysis from the EMPA-REG OUTCOME trial. J Am Soc Nephrol 29:2755–2769. https://doi.org/10.1681/ASN.2018010103
Mulder S, Heerspink HJL, Darshi M, Kim JJ et al (2019) Effects of dapagliflozin on urinary metabolites in people with type 2 diabetes. Diabetes Obes Metab 21:2422–2428. https://doi.org/10.1111/dom.13823
Neuen BL, Young T, Heerspink HJL, Neal B et al (2019) SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 7:845–854. https://doi.org/10.1016/S2213-8587(19)30256-6
Oshima M, Neuen BL, Jardine MJ, Bakris G et al (2020) Effects of canagliflozin on anaemia in patients with type 2 diabetes and chronic kidney disease: a post-hoc analysis from the CREDENCE trial. Lancet Diabetes Endocrinol 8:903–914. https://doi.org/10.1016/S2213-8587(20)30300-4
Qiu H, Novikov A, Vallon V (2017) Ketosis and diabetic ketoacidosis in response to SGLT2 inhibitors: basic mechanisms and therapeutic perspectives. Diabetes Metab Res Rev 33(5). https://doi.org/10.1002/dmrr.2886
Youm YH, Nguyen KY, Grant RW, Goldberg EL et al (2019) The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat Med 21:263–269. https://doi.org/10.1038/nm.3804
Mazidi M, Rezaie P, Gao HK, Kengne AP (2017) Effect of sodium-glucose cotransport-2 inhibitors on blood pressure in people with type 2 diabetes mellitus: a systematic review and meta-analysis of 43 randomized control trials with 22 528 patients. J Am Heart Assoc 6:e004007. https://doi.org/10.1161/JAHA.116.004007
Scholtes RA, Muskiet MHA, van Baar MJB, Hesp AC et al (2021) Natriuretic effect of two weeks of dapagliflozin treatment in patients with type 2 diabetes and preserved kidney function during standardized sodium intake: results of the DAPASALT Trial. Diabetes Care 44:440–447. https://doi.org/10.2337/dc20-2604
Schork A, Saynisch J, Vosseler A, Jaghutriz BA et al (2019) Effect of SGLT2 inhibitors on body composition, fluid status and renin-angiotensin-aldosterone system in type 2 diabetes: a prospective study using bioimpedance spectroscopy. Cardiovasc Diabetol 18:46. https://doi.org/10.1186/s12933-019-0852-y
Striepe K, Jumar A, Ott C, Karg MV et al (2017) Effects of the selective sodium-glucose cotransporter 2 inhibitor empagliflozin on vascular function and central hemodynamics in patients with type 2 diabetes mellitus. Circulation 136:1167–1169. https://doi.org/10.1161/CIRCULATIONAHA.117.029529
Herat LY, Magno AL, Rudnicka C, Hricova J et al (2020) GLT2 inhibitor-induced sympathoinhibition: a novel mechanism for cardiorenal protection. JACC Basic Transl Sci 5:169–179. https://doi.org/10.1016/j.jacbts.2019.11.007
Novikov A, Fu Y, Huang W, Freeman B et al (2019) SGLT2 inhibition and renal urate excretion: role of luminal glucose, GLUT9, and URAT1. Am J Physiol Renal Physiol 316:F173–F185. https://doi.org/10.1152/ajprenal.00462.2018
Stack AG, Han D, Goldwater R, Johansson S et al (2021) Dapagliflozin added to verinurad plus febuxostat further reduces serum uric acid in hyperuricemia: the QUARTZ study. J Clin Endocrinol Metab 106:e2347–e2356. https://doi.org/10.1210/clinem/dgaa748
Neuen BL, Oshima M, Perkovic V, Agarwal R et al (2021) Effects of canagliflozin on serum potassium in people with diabetes and chronic kidney disease: the CREDENCE trial. Eur Heart J 42:4891–4901. https://doi.org/10.1093/eurheartj/ehab497
Toyama T, Neuen BL, Jun M, Ohkuma T et al (2019) Effect of SGLT2 inhibitors on cardiovascular, renal and safety outcomes in patients with type 2 diabetes mellitus and chronic kidney disease: A systematic review and meta-analysis. Diabetes Obes Metab 21:1237–1250. https://doi.org/10.1111/dom.13648
Centers for Disease Control and Prevention (2021) https://www.cdc.gov/. Accessed 30 Sept 2021
Bjornstad P, Drews KL, Caprio S, Gubitosi-Klug R, Nathan DM, Tesfaldet B, Tryggestad J, White NH, Zeitler P (2021) Long-term complications in youth-onset type 2 diabetes. N Engl J Med 385:416–426. https://doi.org/10.1056/NEJMoa2100165
Zeitler P, Hirst K, Pyle L, Linder B et al (2012) A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med 366:2247–2256. https://doi.org/10.1056/NEJMoa1109333
Paik J, Blair HA (2019) Dapagliflozin: a review in type 1 diabetes. Drugs 79:1877–1884. https://doi.org/10.1007/s40265-019-01213-x
Taylor SI, Blau JE, Rother KI, Beitelshees AL (2019) SGLT2 inhibitors as adjunctive therapy for type 1 diabetes: balancing benefits and risks. Lancet Diabetes Endocrinol 7:949–958. https://doi.org/10.1016/S2213-8587(19)30154-8
Coppo R, Peruzzi L, Amore A, Piccoli A et al (2007) IgACE: a placebo-controlled, randomized trial of angiotensin-converting enzyme inhibitors in children and young people with IgA nephropathy and moderate proteinuria. J Am Soc Nephrol 18:1880–1888. https://doi.org/10.1681/ASN.2006040347
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cirillo, L., Ravaglia, F., Errichiello, C. et al. Expectations in children with glomerular diseases from SGLT2 inhibitors. Pediatr Nephrol 37, 2997–3008 (2022). https://doi.org/10.1007/s00467-022-05504-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05504-6