Abstract
Background
Infections are thought to be primarily responsible for triggering relapse in children with steroid-sensitive nephrotic syndrome (NS). The COVID-19 pandemic promoted physical distancing, facial mask wearing, and greater attention to infection-prevention measures resulting in decreased transmission of infections. We hypothesized there would also be a decreased rate of NS relapse during this period.
Methods
We conducted a single-center retrospective chart review of children with steroid-sensitive NS. Demographics, rate of relapses, and rate of hospitalizations were collected for a baseline pre-pandemic period (BPP) and for the social distancing period during the pandemic (SDP).
Results
One hundred twenty-two children with primary steroid-sensitive NS were identified and 109 were followed for the duration of the study period. The paired rate of relapse per subject per year was significantly lower during the SDP (0.6 relapses per subject per year ± 1 SD) compared to the BPP (1.0 relapses per subject per year ± 0.9 SD), P < 0.01. A subgroup of 32 subjects who were newly diagnosed with NS during the BPP similarly had significantly fewer relapses during the SDP (0.8 ± 1 SD) than during the BPP (1.4 ± 1 SD), P = 0.01.
Conclusions
Our results support the hypothesis of lower rates of NS relapse and hospitalizations during social distancing for all subjects in our cohort and a subgroup of those newly diagnosed. Lower relapse rates were likely attributable to decreased transmission of infections and greater attention to infection prevention.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most children with idiopathic nephrotic syndrome enter remission with corticosteroid therapy and are considered to have steroid-sensitive nephrotic syndrome (NS) [1, 2]. However, as many as 60 to 90% of those initially responsive to steroid therapy will relapse, characterized by recurrence of nephrotic-range proteinuria, and require additional courses of steroids or addition of other immunosuppressive medications to maintain a remission [3]. While the etiology and pathophysiology of relapses is unknown, there is an association with upper respiratory infections (URI) that was initially described in 1986 [4]. Since then, this has been re-demonstrated, along with an association of relapse with gastroenteritis and urinary tract infections [5, 6]. Interestingly, school events (such as examinations) and upcoming outpatient visits have also been associated with disease relapse, potentially implicating psychological stress as a trigger [7].
During the COVID-19 pandemic, institution of “social distancing” measures (such as quarantine, stay at home orders, and virtual schooling), near-universal masking, and greater public attention to hand hygiene and infection prevention have become common practice. These actions not only curbed transmission of SARS-CoV-2, but also decreased activity of other common community respiratory viruses, resulting in fewer hospital and ICU admissions for influenza, RSV, and other illnesses during the social distancing period [8,9,10,11,12,13]. Given these findings, we hypothesized that, as compared to the prior years, rates of NS relapses would similarly be lower during this period.
Methods
Study design and definitions
We performed a retrospective chart review of subjects, ages 1 to 21 years old, seen by pediatric nephrology at Rady Children’s Hospital San Diego between March 1, 2015, and March 31, 2021. Subjects were identified by ICD-9 or ICD-10 codes for proteinuria, nephrotic syndrome, minimal change disease (MCD), focal segmental glomerular sclerosis (FSGS), or membranous nephropathy (MN). Charts were reviewed, and subjects were included for analysis if their clinical course was consistent with primary idiopathic steroid-sensitive NS, defined as urine dipstick readings of negative or trace protein on three consecutive days with steroid therapy alone. Concurrent with a diagnosis of steroid-sensitive NS, subjects were only included if they entered remission during their initial steroid treatment. We included those with an initial diagnosis of NS prior to March 1, 2015, provided they had follow-up in our health system for the duration of the study period. Subjects received all pediatric nephrology care within our system, as it is the only center within a large catchment area. Any NS-related care done by local medical facilities was done in consultation with our center and documented in the medical record. A subset of patients with new-onset NS during the period of July 2017 to June 2019 were identified. Subjects were excluded if they had steroid-resistant disease or were lost to follow-up, moved to a different health system, or transitioned to adult care during the study period.
The baseline pre-pandemic period (BPP) was defined as March 1, 2015, to February 29, 2020. The social distancing period (SDP) was defined as March 1, 2020, to March 1, 2021. The dates of the SDP were chosen to coincide with the height of social distancing and stay-at-home orders in Southern California. All subjects received initial treatment with a standardized protocol of prednisone 60 mg/m2/day for 6 weeks, followed by 40 mg/m2/day every other day for 6 weeks, followed by a 4-week steroid taper. Relapses and hospitalizations were counted starting after subjects completed an initial course of steroid treatment. NS relapse was defined as 3 + proteinuria for at least 3 days on home urine dipstick after a period of remission. Relapses were treated with a standardized protocol of prednisone 60 mg/m2/day until remission followed by a 4-week steroid taper. If subjects relapsed during the steroid taper, they were biopsied and steroid-sparing therapy was started. Hospitalizations were counted only if occurring for diuresis or other NS-related complications while subjects were actively in relapse. If subjects were hospitalized at the time of their initial diagnosis, this was not included in count of hospitalizations. If kidney biopsy was done, the etiology of nephrotic syndrome (MCD, FSGS, or MN) was noted and those without a biopsy were presumed to have MCD.
Data collection and outcomes
Demographic information collected included age, sex, diagnosis (including biopsy results), steroid-sparing immunosuppressive medications, diagnosis and treatment of hypertension, episodes of acute kidney injury, use of renin–angiotensin–aldosterone system (RAAS) blockers, and COVID-19 infection. Outcomes included the rate of relapses and rate of hospitalizations per subject per year in those paired during the BPP and in the SDP. Secondary outcomes included total cases of new-onset NS and seasonality of either initial diagnosis or relapses of NS.
Statistical analysis
Continuous variables are reported as mean and standard deviations (SD) or as median and interquartile range (IQR). Categorical variables are described as frequency and percentages. Differences between rates of relapse and hospitalizations for subjects paired pre- and post-pandemic were compared with a related samples Wilcoxon signed-rank test comparing the mean relapses and hospitalizations per subject for the BPP with the relapses and hospitalizations per subject during the SDP. Differences in characteristics of subjects pre- and post-pandemic including immunosuppressive medications, use of RAAS blockers, and episodes of AKI were compared using McNemar’s test. Mean numbers of relapses and cases of new-onset NS during each season were compared with one-way ANOVA. Two-sided P < 0.05 was considered statistically significant. Statistical analysis was performed with IBM SSPS v27 (Armonk, NY).
Ethics
The institutional review boards at the University of California, San Diego and Rady Children’s Hospital San Diego approved this study.
Results
Demographics
A total of 588 subjects were initially identified with a diagnosis of proteinuria, NS, MCD, FSGS, or MN. Following initial review, 122 subjects were identified as having steroid-sensitive NS and were included in this study. Demographics of all 122 subjects are reported in Table 1. There were 109 subjects (89%) who had complete follow-up during the BPP through the SDP and the remaining 13 (11%) were cases of new-onset NS during the SDP (Fig. 1). The median age at time of review was 10 years (interquartile range (IQR) 7–13 years), and 80 (66%) were male. Median age at time of diagnosis was 3 years (IQR 2–6 years). Kidney biopsy was performed in 92 subjects (75%). Biopsies were obtained prior to escalation to steroid-sparing therapy, after the third relapse, or for an atypical presentation (i.e., acute kidney injury or presence of hematuria), as suggested by KDIGO guidelines [2]. Most biopsies demonstrated MCD (n = 83), six showed FSGS, and three revealed MN. Biopsies were not performed in 30 subjects (25%) who had presumed MCD (Table 1). Nine subjects (7%) tested positive for COVID-19 infection over the course of the SDP. Thirty-two patients were newly diagnosed with NS during the second half of the BPP.
Outcomes
The paired rate of relapse per subject per year for the 109 individuals followed for the duration of the study period was significantly lower during the SDP (0.6 mean relapses per subject per year ± 1 SD) compared to the BPP (1.0 mean relapses per subject per year ± 0.9 SD), P < 0.01 (Table 2). Similar to relapse rates, the paired rate of hospitalization per subject per year was significantly lower during the SDP (0.1 mean hospitalizations per subject per year ± 0.2 SD) compared to the BPP (0.5 mean hospitalizations per subject per year ± 0.7 SD), P < 0.01 (Table 2). When comparing the paired relapse rate between the final year of the BPP and SDP by different time intervals since initial diagnosis, there were no significant differences but a trend towards a lower relapse rate in those who have had a longer disease course (Table 3).
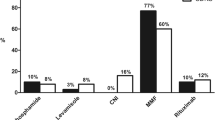
Among all subjects receiving steroid-sparing immunosuppression, calcineurin inhibitors (CNI) were most commonly used. Many subjects were also treated with mycophenolate mofetil (MMF), cyclophosphamide, or anti-CD20 agents. There was significantly more use of CNI and MMF use during the BPP compared to the SDP (Table 4). The number of steroid-sparing immunosuppressants used by subjects paired during the final year of the BPP and SDP was similar, each with a mean of 0.6 medications per patient (P = 0.8). Rates of those with hypertension requiring treatment, having at least one acute kidney injury episode, and use of renin–angiotensin–aldosterone system blockers were similar between both groups.
In a subgroup of subjects newly presenting with NS during the second half the BPP, paired rate of relapse during the SDP (0.8 relapses per subject per year ± 1 SD) was significantly lower than that of the BPP (1.4 relapses per subject per year ± 1 SD), P = 0.01 (Table 2). Similarly, the rate of hospitalizations was significantly lower during the SDP (0.1 hospitalizations per subject per year ± 0.3 SD) compared to the BPP (0.4 hospitalizations per subject per year ± 0.7 SD), P = 0.01 (Table 2). In this subgroup, 3 subjects (9%) had an escalation in their steroid-sparing immunosuppressant regimen, 3 subjects (9%) had a deescalated immunosuppressant regimen, and there were no substantial changes in immunosuppressants in 26 subjects (81%) (Table 5).
There were a similar number of cases of new-onset NS during the BPP and the SDP. The SDP saw a total of 13 new cases per year versus 12 cases per year during the BPP. When stratified by time of year throughout all years of the study period, there was a trend towards more new cases of NS during the spring and summer seasons with an average of 3.8 and 3.3 cases per year versus the autumn and winter months 2.8 and 2.7 cases per year, respectively, P = 0.7. This differed from the seasonality of NS relapses. There was also a trend toward more relapses occurring in the winter and spring (21 and 19 relapses per year) when compared to the autumn and summer seasons, having 17 and 18 relapses per year, respectively, P = 0.3.
Discussion
Our results support the hypothesis of lower rates of NS relapse and hospitalizations during the COVID-19 pandemic social distancing period. The significantly lower rates of relapse are most likely due to the decreased incidence and transmission of viral infections occurring as a result of social distancing. Consistent with this, it has been shown that social distancing and greater attention to infection prevention had the intended effect of curbing COVID-19 spread, yet also reduced the frequency of viruses in the community [8]. Other conditions with infection-related triggers, such as asthma exacerbations and recurrent tonsillitis, also saw lower rates of exacerbations and resultant lower rates of hospitalization during this period [11,12,13].
It is important to acknowledge that rates of relapse also decrease with a longer duration from the time of initial NS diagnosis [14,15,16,17] and this was redemonstrated in our study (Table 3). This may reflect the intended effect of steroid-sparing immunosuppressive medications or simply be demonstrating the natural course of MCD, as it is common that relapses become less frequent with increasing age [15, 17]. To address this, we separately analyzed the paired rate of relapse and hospitalization for a group of subjects within 2 years of initial NS diagnosis in the latter half the BPP compared to the SDP. This subgroup of 32 subjects was isolated to better characterize the early phase of the disease and to minimize the confounding of intensified steroid-sparing immunosuppression used later in the disease course. The finding of significantly lower rates of relapse and hospitalization in this subgroup provides additional evidence for our hypothesis and suggests social distancing may be particularly impactful in the initial years after NS diagnosis, as the number of relapses early in the course of the disease has been shown to be predictive of subsequent relapse frequency and disease severity [14].
Less hospitalizations for NS relapse during the SDP also suggest a trend of decreased severity of relapse and fewer significant infectious complications of NS. During the height of the early pandemic, there was an environment of hyper-awareness regarding infection and health-related complications. In this setting, caregivers may have been more likely to regularly test urine to detect relapses sooner and prompt initiation of steroid therapy and fluid and sodium restriction that may have allowed some subjects to avoid hospitalization, particularly in those with a more recent diagnosis who may be closer to the initial treatment course and education. Lower rates of hospitalization during the SDP could also be attributed to caregiver reluctance to visit hospitals, loss of contact due to less in-person visits, or travel restrictions. However, the contribution of these factors in our cohort is likely minimal and we do not believe pandemic-related practice variation contributed to attempts at avoiding hospitalization. Throughout the SDP, we had frequent contact with patients and caregivers via telemedicine at a volume similar to pre-pandemic in-person visits. Providers and staff had close contact with caregivers who actively continued relapse surveillance and relapse treatment, including the use of an outpatient infusion center that maintained normal operations.
Our results highlight the role infections can play in NS relapse and suggest counseling patients and caregivers about the importance of hand hygiene and other methods to avoid infection can potentially mitigate the frequency and severity of relapses. Quality improvement initiatives to enhance patient and caregiver education about the NS disease process have been shown to reduce hospital admissions for relapse [18]. While reducing peer interaction is another possible mechanism by which to curb infection transmission, we do not advocate for routinely restricting activities or home schooling for children with NS. Rather, we suggest integration of simple infection-prevention measures into a standardized educational program that may have the potential to decrease severity of relapses and complications, particularly in the initial years following diagnosis.
Strategies to avoid infection in children with NS may reduce the number of relapses but also might have implications on the progression of the disease. Prior work has demonstrated that some initially steroid-responsive NS patients can progress to steroid-resistant disease requiring steroid-sparing immunosuppressants and are classified as patients with “late steroid resistance” [19, 20]. Patients with late steroid resistance typically have more frequent relapses and a shorter interval from initial diagnosis to first relapse [21]. Our data support that avoidance of infection can reduce relapses, and the potential this may have on preventing some children from developing late steroid resistance is a hypothesis that merits further study. A standardized approach to counseling patients about infection prevention could limit NS severity and spare exposure to additional immunosuppressive medications and potential complications.
Strengths of our study include a robust sample size representative of various etiologies of steroid-sensitive NS and the completeness of follow-up throughout the study period. There are important limitations including its retrospective and observational nature, where selection bias may play a role, as less complicated NS cases may have been lost to follow-up or managed by pediatricians outside of our system. Additionally, the chart review did not include identification of relapse triggers, as this information was rarely recorded, and there is no standardized documentation for NS relapses. This is a potential area for quality improvement at our center. Future efforts will be focused on standardizing the approach to NS documentation to allow for identification of relapse triggers and determine associations with steroid responsiveness and other demographic characteristics.
In conclusion, we demonstrate that rates of NS relapse were lower during the COVID-19 pandemic, likely due to reduced transmission of infectious triggers. Social distancing and related infection-prevention measures have an important role early in the disease course but may be less important in children with frequent relapses or already on steroid-sparing therapy. These findings have important implications for patient and family counseling, relapse severity, and disease prognosis. Future studies are needed to confirm these findings and directly evaluate the impact of documented infections, vaccinations, family counseling, hand hygiene, masking, and in-person versus virtual school attendance on rates of NS relapse.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Eddy AA, Symons JM (2003) Nephrotic syndrome in childhood. Lancet 362:629–639. https://doi.org/10.1016/S0140-6736(03)14184-0
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group (2021) Chapter 4: nephrotic syndrome in children. Kidney Int Suppl 100:163–171. https://doi.org/10.1016/j.kint.2021.05.021
Dossier C, Delbet JD, Boyer O, Daoud P, Mesple B, Pellegrino B et al (2019) Five-year outcome of children with idiopathic nephrotic syndrome: the NEPHROVIR population-based cohort study. Pediatr Nephrol 34:671–678. https://doi.org/10.1007/s00467-018-4149-2
MacDonald NE, Wolfish N, McLaine P, Phipps P, Rossier E (1986) Role of respiratory viruses in exacerbations of primary nephrotic syndrome. J Pediatr 108:378–382. https://doi.org/10.1016/s0022-3476(86)80876-9
Uwaezuoke SN (2015) Steroid-sensitive nephrotic syndrome in children: triggers of relapse and evolving hypotheses on pathogenesis. Italian J Pediatr 41:19. https://doi.org/10.1186/s13052-015-0123-9
Gulati S, Kher V, Gupta A, Arora P, Rai PK, Sharma RK (1995) Spectrum of infections in Indian children with nephrotic syndrome. Pediatr Nephrol 9:431–434. https://doi.org/10.1007/BF00866719
Takahashi S, Wada N, Murakami H, Funaki S, Inagaki T, Harada K, Nagata M (2007) Triggers of relapse in steroid-dependent and frequently relapsing nephrotic syndrome. Pediatr Nephrol 22:232–236. https://doi.org/10.1007/s00467-006-0316-y
Partridge E, McCleery E, Cheema R, Nakra N, Lakshminrusimha S, Tancredi DJ, Blumberg DA (2021) Evaluation of seasonal respiratory virus activity before and after the statewide COVID-19 shelter-in-place order in Northern California. JAMA Netw Open 4:e2035281. https://doi.org/10.1001/jamanetworkopen.2020.35281
Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, Cohen C, Fry AM (2020) Decreased Influenza Activity During the COVID-19 Pandemic - United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep 69:1305–1309. https://doi.org/10.15585/mmwr.mm6937a6
Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M (2020) Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr Infect Dis J 39:e423–e427. https://doi.org/10.1097/INF.0000000000002845
Krivec U, Kofol Seliger A, Tursic J (2020) COVID-19 lockdown dropped the rate of paediatric asthma admissions. Arch Dis Child 10:809–810. https://doi.org/10.1136/archdischild-2020-31952211
Vásquez-Hoyos P, Diaz-Rubio F, Monteverde-Fernandez N, Jaramillo-Bustamante JC, Carvajal C, Serra A, Karsies T, Rotta AT, González-Dambrauskas S, LARed Network (2020) Reduced PICU respiratory admissions during COVID-19. Arch Dis Child. https://doi.org/10.1136/archdischild-2020-320469
Heward E, Rocke J, Kumar N, Izzat S (2020) Recurrent tonsillitis and parental perceptions of tonsillectomy during the COVID-19 pandemic. Int J Pediatr Otorhinolaryngol 139:110463. https://doi.org/10.1016/j.ijporl.2020.110463
Tarshish P, Tobin JN, Bernstein J, Edelmann CM (1997) Prognostic significance of the early course of minimal change nephrotic syndrome: report of the International Study of Kidney Disease in Children. J Am Soc Nephrol 8:769–776. https://doi.org/10.1681/ASN.V85769
Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS (1985) Long-term outcome for children with minimal-change nephrotic syndrome. Lancet 1:368–370. https://doi.org/10.1016/s0140-6736(85)91387-x
Carter SA, Mistry S, Fitzpatrick J, Banh T, Hebert D, Langlois V et al (2019) Prediction of short- and long-term outcomes in childhood nephrotic syndrome. Kidney Int Rep 5:426–434. https://doi.org/10.1016/j.ekir.2019.12.015
Fakhouri F, Bocquet N, Taupin P, Presne C, Gagnadoux MF et al (2003) Steroid-sensitive nephrotic syndrome: from childhood to adulthood. Am J Kidney Dis 41:550–557. https://doi.org/10.1053/ajkd.2003.50116
Charnaya O, Ahn SY (2019) Quality improvement initiative to reduce admissions for nephrotic syndrome relapse in pediatric patients. Front Pediatr 7:112. https://doi.org/10.3389/fped.2019.00112
Srivastava RN, Agarwal RK, Moudgil A, Bhuyan UN (1986) Late resistance to corticosteroids in nephrotic syndrome. J Pediatr 108:66–70. https://doi.org/10.1016/s0022-3476(86)80770-3
Straatmann C, Ayoob R, Gbadegesin R, Gibson K, Rheault MN, Srivastava T et al (2013) Treatment outcome of late steroid-resistant nephrotic syndrome: a study by the Midwest Pediatric Nephrology Consortium. Pediatr Nephrol 28:1235–1241. https://doi.org/10.1007/s00467-013-2483-y
Kim JS, Bellew CA, Silverstein DM, Aviles DH, Boineau FG, Vehaskari VM (2005) High incidence of initial and late steroid resistance in childhood nephrotic syndrome. Kidney Int 68:1275–1281. https://doi.org/10.1111/j.1523-1755.2005.00524.x
Acknowledgements
Study data were collected and managed using REDCap electronic data capture tools hosted at University of California, San Diego (CTRI grant support UL1TR001442).
Funding
CYB is funded by NIDDK 1K23DK129836-01 and AHA Award 857722.
Author information
Authors and Affiliations
Contributions
CC and EI contributed to the study conception and design. Material preparation, data collection, and analysis were performed by CC. Additional data analysis was performed by CB. The first draft of the manuscript was written by CC. All authors commented on previous versions of the manuscript. EI supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of the University of California San Diego and Rady Children’s Hospital approved this study.
Consent to participate
Need for consent was waived by IRB due to minimal risk to participants.
Consent for publication
Need for consent was waived by IRB due to minimal risk to participants.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Crane, C., Bakhoum, C. & Ingulli, E. Rates of idiopathic childhood nephrotic syndrome relapse are lower during the COVID-19 pandemic. Pediatr Nephrol 37, 2679–2685 (2022). https://doi.org/10.1007/s00467-022-05483-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05483-8