Abstract
Background
With adult patients, the measurement of [TIMP-2]*[IGFBP7] can predict the risk of moderate to severe AKI within 12 h of testing. In pediatrics, however, the performance of [TIMP-2]*[IGFBP7] as a predictor of AKI was less studied and yet to be widely utilized in clinical practice. This study was conducted to validate the utility of [TIMP-2]*[IGFBP7] as an earlier biomarker for AKI prediction in Chinese infants and small children.
Methods
We measured urinary [TIMP-2]*[IGFBP7] using NEPHROCHECK® at eight perioperative time points in 230 patients undergoing complex cardiac surgery and evaluated the performance of [TIMP-2]*[IGFBP7] for predicting severe AKI within 72 h of surgery.
Results
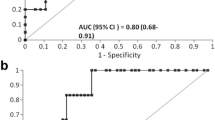
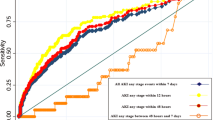
A total of 50 (22%) of 230 developed AKI stages 2–3 within 72 h after CPB initiation. In the AKI stage 2–3 patients, two patterns of serum creatinine (SCr) elevations were observed. The patients with only a transient increase in SCr within 24 h (< 24 h, early AKI 2–3) did not experience a worse outcome than patients in AKI stage 0–1. AKI stage 2–3 patients with SCr elevation after 24 h (24–72 h, late AKI 2–3), as well as AKI dialysis patients (together designated severe AKI), did experience worse outcomes. Compared to AKI stages 0–1, significant elevations of [TIMP-2]*[IGFBP7] values were observed in severe AKI patients at hours T2, T4, T12, and T24 following CPB initiation. The AUC for predicting severe AKI with [TIMP-2]*[IGFBP7] at T2 (AUC = 0.76) and maximum T2/T24 (AUC = 0.80) are higher than other time points. The addition of the NEPHROCHECK® test to the postoperative parameters improved the risk assessment of severe AKI.
Conclusions
Multiple AKI phenotypes (early versus late AKI) were identified after pediatric complex cardiac surgery according to SCr-based AKI definition. Urinary [TIMP-2]*[IGFBP7] predicts late severe AKI (but not early AKI) as early as 2 h following CPB initiation.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information





Similar content being viewed by others
Data availability
All datasets underlying the manuscript results are available upon request to the corresponding author (XZM).
Abbreviations
- AKI:
-
Acute kidney injury
- CPB:
-
Cardiopulmonary bypass
- SCr:
-
Serum creatinine
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- TIMP-2:
-
Tissue inhibitor metalloproteinases-2
- IGFBP7:
-
Insulin-like growth factor-binding protein 7
- RACHS:
-
Risk adjusted classification for congenital heart surgery
- RACHS-1:
-
Risk adjustment for congenital heart surgery score version 1
- IQR:
-
Inter-quantile range
- ROC:
-
Receiver operating curve
- AUC:
-
Area under curve
- CI:
-
Confidence intervals
- MVIS:
-
Maximal vasoactive inotrope scores
- CSA-AKI:
-
Cardiac surgery-associated acute kidney injury
References
Aydin SI, Seiden HS, Blaufox AD, Parnell VA, Choudhury T, Punnoose A, Schneider J (2012) Acute kidney injury after surgery for congenital heart disease. Ann Thorac Surg 94:1589–1595
Li S, Krawczeski CD, Zappitelli M, Devarajan P, Thiessen-Philbrook H, Coca SG, Kim RW, Parikh CR, TRIBE-AKI Consortium (2011) Incidence, risk factors, and outcomes of acute kidney injury after pediatric cardiac surgery: a prospective multicenter study. Crit Care Med 39:1499
Morgan CJ, Zappitelli M, Robertson CM, Alton GY, Sauve RS, Joffe AR, Ross DB, Rebeyka IM, Western Canadian Complex Pediatric Therapies Follow-Up Group (2013) Risk factors for and outcomes of acute kidney injury in neonates undergoing complex cardiac surgery. J Pediatr 162:127.e121
Kellum J, Lameire N, Aspelin P, Barsoum R, Burdmann E, Goldstein S, Herzog C, Joannidis M, Kribben A, Levey A, MacLeod A, Mehta R, Murray P, Naicker S, Opal S, Schaefer F, Schetz M, Uchino S (2012) Kidney disease: Improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl 2:1–138
Schneider A, Ostermann M (2017) The AKI glossary. Intensive Care Med 43:893–897
Delanaye P, Mariat C, Cavalier E, Maillard N, Krzesinski JM, White CA (2011) Trimethoprim, creatinine and creatinine-based equations. Nephron Clin Pract 119:c187–c194
Heymsfield SB, Arteaga C, McManus C, Smith J, Moffitt S (1983) Measurement of muscle mass in humans: validity of the 24-hour urinary creatinine method. Am J Clin Nutr 37:478–494
Preiss DJ, Godber IM, Lamb EJ, Dalton RN, Gunn IR (2007) The influence of a cooked-meat meal on estimated glomerular filtration rate. Ann Clin Biochem 44:35–42
Liu KD, Thompson BT, Ancukiewicz M, Steingrub JS, Douglas IS, Matthay MA, Wright P, Peterson MW, Rock P, Hyzy RC et al (2011) Acute kidney injury in patients with acute lung injury: impact of fluid accumulation on classification of acute kidney injury and associated outcomes. Crit Care Med 39:2665–2671
Alten JA, Cooper DS, Blinder JJ, Selewski DT, Tabbutt S, Sasaki J, Gaies MG, Bertrandt RA, Smith AH, Reichle G et al (2021) Epidemiology of acute kidney injury after neonatal cardiac surgery: a report from the multicenter neonatal and pediatric heart and renal outcomes network. Crit Care Med 49:e941–e951
Maciel AT, Nassar AP Jr, Vitorio D (2016) Very transient cases of acute kidney injury in the early postoperative period after cardiac surgery: the relevance of more frequent serum creatinine assessment and concomitant urinary biochemistry evaluation. J Cardiothorac Vasc Anesth 30:56–63
Basu RK, Wong HR, Krawczeski CD, Wheeler DS, Manning PB, Chawla LS, Devarajan P, Goldstein SL (2014) Combining functional and tubular damage biomarkers improves diagnostic precision for acute kidney injury after cardiac surgery. J Am Coll Cardiol 64:2753–2762
Waikar SS, Bonventre JV (2009) Creatinine kinetics and the definition of acute kidney injury. J Am Soc Nephrol 20:672–679
Bihorac A, Chawla LS, Shaw AD, Al-Khafaji A, Davison DL, DeMuth GE, Fitzgerald R, Gong MN, Graham DD, Gunnerson K et al (2014) Validation of cell-cycle arrest biomarkers for acute kidney injury using clinical adjudication. Am J Respir Crit Care Med 189:932–939
Kashani K, Al-Khafaji A, Ardiles T, Artigas A, Bagshaw SM, Bell M, Bihorac A, Birkhahn R, Cely CM, Chawla LS et al (2013) Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care 17:R25
Meersch M, Schmidt C, Van Aken H, Rossaint J, Gorlich D, Stege D, Malec E, Januszewska K, Zarbock A (2014) Validation of cell-cycle arrest biomarkers for acute kidney injury after pediatric cardiac surgery. PLoS One 9:e110865
Wetz AJ, Richardt EM, Wand S, Kunze N, Schotola H, Quintel M, Brauer A, Moerer O (2015) Quantification of urinary TIMP-2 and IGFBP-7: an adequate diagnostic test to predict acute kidney injury after cardiac surgery? Crit Care 19:3
Boonstra J, Post JA (2004) Molecular events associated with reactive oxygen species and cell cycle progression in mammalian cells. Gene 337:1–13
Gist KM, Goldstein SL, Wrona J, Alten JA, Basu RK, Cooper DS, Soranno DE, Duplantis J, Altmann C, Gao Z et al (2017) Kinetics of the cell cycle arrest biomarkers (TIMP-2*IGFBP-7) for prediction of acute kidney injury in infants after cardiac surgery. Pediatr Nephrol 32:1611–1619
Baumgartner H, De Backer J, Babu-Narayan SV, Budts W, Chessa M, Diller GP, Lung B, Kluin J, Lang IM, Meijboom F et al (2021) 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J 42:563–645
Jenkins KJ (2004) Risk adjustment for congenital heart surgery: the RACHS-1 method. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 7:180–184
Wernovsky G, Wypij D, Jonas RA, Mayer JE Jr, Hanley FL, Hickey PR, Walsh AZ, Chang AC, Castaneda AR, Newburger JW et al (1995) Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants. A comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation 92:2226–2235
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, Muller M (2011) pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics 12:77
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Gocze I, Koch M, Renner P, Zeman F, Graf BM, Dahlke MH, Nerlich M, Schlitt HJ, Kellum JA, Bein T (2015) Urinary biomarkers TIMP-2 and IGFBP7 early predict acute kidney injury after major surgery. PLoS One 10:e0120863
Pilarczyk K, Edayadiyil-Dudasova M, Wendt D, Demircioglu E, Benedik J, Dohle DS, Jakob H, Dusse F (2015) Urinary [TIMP-2]*[IGFBP7] for early prediction of acute kidney injury after coronary artery bypass surgery. Ann Intensive Care 5:50
Beitland S, Waldum-Grevbo BE, Nakstad ER, Berg JP, Troseid AS, Brusletto BS, Brunborg C, Andersen GO, Sunde K (2016) Urine biomarkers give early prediction of acute kidney injury and outcome after out-of-hospital cardiac arrest. Crit Care 20:314
Guzzi LM, Bergler T, Binnall B, Engelman DT, Forni L, Germain MJ, Gluck E, Gocze I, Joannidis M, Koyner JL et al (2019) Clinical use of [TIMP-2]*[IGFBP7] biomarker testing to assess risk of acute kidney injury in critical care: guidance from an expert panel. Crit Care 23:225
Godi I, De Rosa S, Martino F, Bazzano S, Martin M, Boni E, Carta MR, Tamayo Diaz C, Mari G, Lorenzin A et al (2020) Urinary [TIMP-2] x [IGFBP7] and serum procalcitonin to predict and assess the risk for short-term outcomes in septic and non-septic critically ill patients. Ann Intensive Care 10:46
Tai Q, Yi H, Wei X, Xie W, Zeng O, Zheng D, Sun J, Wang G, Wang S, Liu G (2020) The accuracy of urinary TIMP-2 and IGFBP7 for the diagnosis of cardiac surgery-associated acute kidney injury: a systematic review and meta-analysis. J Intensive Care Med 35:1013–1025
Zaouter C, Potvin J, Bats ML, Beauvieux MC, Remy A, Ouattara A (2018) A combined approach for the early recognition of acute kidney injury after adult cardiac surgery. Anaesth Crit Care Pain Med 37:335–341
Vandenberghe W, De Loor J, Hoste EA (2017) Diagnosis of cardiac surgery-associated acute kidney injury from functional to damage biomarkers. Curr Opin Anaesthesiol 30:66–75
Cummings JJ, Shaw AD, Shi J, Lopez MG, O’Neal JB, Billings FT 4th (2019) Intraoperative prediction of cardiac surgery-associated acute kidney injury using urinary biomarkers of cell cycle arrest. J Thorac Cardiovasc Surg 157:1545-1553.e5
Su LJ, Li YM, Kellum JA, Peng ZY (2018) Predictive value of cell cycle arrest biomarkers for cardiac surgery-associated acute kidney injury: a meta-analysis. Br J Anaesth 121:350–357
Esmeijer K, Schoe A, Ruhaak LR, Hoogeveen EK, Soonawala D, Romijn F, Shirzada MR, van Dissel JT, Cobbaert CM, de Fijter JW (2021) The predictive value of TIMP-2 and IGFBP7 for kidney failure and 30-day mortality after elective cardiac surgery. Sci Rep 11:1071
Dong L, Ma Q, Bennett M, Devarajan P (2017) Urinary biomarkers of cell cycle arrest are delayed predictors of acute kidney injury after pediatric cardiopulmonary bypass. Pediatr Nephrol 32:2351–2360
Bojan M, Pieroni L, Semeraro M, Froissart M (2020) Cell-cycle arrest biomarkers: usefulness for cardiac surgery-related acute kidney injury in neonates and infants. Pediatr Crit Care Med 21:563–570
Blinder JJ, Goldstein SL, Lee VV, Baycroft A, Fraser CD, Nelson D, Jefferies JL (2012) Congenital heart surgery in infants: effects of acute kidney injury on outcomes. J Thorac Cardiovasc Surg 143:368–374
Perinel S, Vincent F, Lautrette A, Dellamonica J, Mariat C, Zeni F, Cohen Y, Tardy B, Souweine B, Darmon M (2015) Transient and persistent acute kidney injury and the risk of hospital mortality in critically ill patients: results of a multicenter cohort study. Crit Care Med 43:e269-275
Brown JR, Kramer RS, Coca SG, Parikh CR (2010) Duration of acute kidney injury impacts long-term survival after cardiac surgery. Ann Thorac Surg 90:1142–1148
Desanti De Oliveira B, Xu K, Shen TH, Callahan M, Kiryluk K, D’Agati VD, Tatonetti NP, Barasch J, Devarajan P (2019) Molecular nephrology: types of acute tubular injury. Nat Rev Nephrol 15:599–612
Makris K, Spanou L (2016) Acute kidney injury: diagnostic approaches and controversies. Clin Biochem Rev 37:153–175
Noto A, Cortegiani A, David A (2019) NephroCheck: should we consider urine osmolality? Crit Care 23:48
Mayer T, Bolliger D, Scholz M, Reuthebuch O, Gregor M, Meier P, Grapow M, Seeberger MD, Fassl J (2017) Urine biomarkers of tubular renal cell damage for the prediction of acute kidney injury after cardiac surgery-a pilot study. J Cardiothorac Vasc Anesth 31:2072–2079
Acknowledgements
Zhuoming Xu, Wei Wang, and Ji Liang are co-corresponding authors for this study. We would like to thank the patients and their parents for their support and participation in this study. This work was supported by the Shanghai Key Laboratory of Clinical Molecular Diagnostics for Pediatrics (20dz2260900).
Funding
This work was supported by the Shanghai Key Laboratory of Clinical Molecular Diagnostics for Pediatrics (20dz2260900).
Author information
Authors and Affiliations
Contributions
Y Tao, F Heskia, JH Huang, J Liang, W Wang, and ZM Xu designed the study. R Qin, Y Tao, MJ Zhang, LQ Chen, and F Wu collected patient data and samples. LQ Chen and F Wu performed NEPHROCHECK® tests. B Kang, Y Tao, F Heskia, HW Chen, J Liang, and ZM Xu analyzed the data. Y Tao, F Heskia, MJ Zhang, K Brengel-Pesce, X Mo, J Liang, W Wang, and ZM Xu discussed the results and performed additional analyses. The first draft of the manuscript was written by Y Tao, F Heskia, B Kang, LQ Chen, J Liang, and ZM Xu, and all authors commented on previous versions of the manuscript. ZM Xu, W Wang, and J Liang take responsibility for the content of the manuscript and the accuracy of the reported data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board and the Ethics Committee of Shanghai Children’s Medical Center (SCMCIRB-K2019009). Written informed consent was obtained from all participating patients and/or their parents. Clinical Trial Registry Number: NCT03963284.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tao, Y., Heskia, F., Zhang, M. et al. Evaluation of acute kidney injury by urinary tissue inhibitor metalloproteinases-2 and insulin-like growth factor-binding protein 7 after pediatric cardiac surgery. Pediatr Nephrol 37, 2743–2753 (2022). https://doi.org/10.1007/s00467-022-05477-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-022-05477-6