Abstract
Background
Although many pediatric nephrologists consider focal segmental glomerulosclerosis (FSGS) and minimal change disease (MCD) as separate clinical entities, whether the initial histology could affect clinical courses in children with steroid-resistant nephrotic syndrome (SRNS) suspected of having an immune-based etiology remains unknown, especially for long-term outcomes.
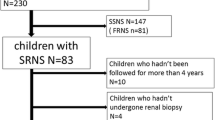
Methods
We retrospectively reviewed long-term outcomes (> 3 years; median follow-up, 9.1 years) of 21 children with initial SRNS (FSGS, N = 9; MCD, N = 12) who achieved complete remission with immunosuppressive agents, including cyclosporine.
Results
At NS onset, incidence of acute kidney injury (67% vs. 8%, P < 0.05) and proportion of patients with non-selective proteinuria (56% vs. 0%, P < 0.01) were significantly higher in the FSGS group than the MCD group. Furthermore, median days until complete remission after treatment was significantly longer in the FSGS group than the MCD group (116 days vs. 45 days, P < 0.001). Although subsequent biopsy histology of the 12 patients in the MCD group was still identical in all MCD, three of nine patients in the FSGS group were reclassified from FSGS to MCD at second biopsy. At last visit, all patients maintained complete remission, and none developed chronic kidney disease.
Conclusions
Initial presentation in the FSGS group was characterized by more severe clinical manifestations than the MCD group. If complete remission is achieved, FSGS and MCD in children with immune-mediated SRNS may constitute a single disease spectrum because the long-term outcomes are favorable, irrespective of initial histology.
Similar content being viewed by others
References
Lee JM, Kronbichler A, Shin JI, Oh J (2020) Current understandings in treating children with steroid-resistant nephrotic syndrome. Pediatr Nephrol. https://doi.org/10.1007/s00467-020-04476-9
Paik KH, Lee BH, Cho HY, Kang HG, Ha IS, Cheong HI, Jin DK, Moon KC, Choi Y (2007) Primary focal segmental glomerular sclerosis in children: clinical course and prognosis. Pediatr Nephrol 22:389–395
Gipson DS, Chin H, Presler TP, Jennette C, Ferris ME, Massengill S, Gibson K, Thomas DB (2006) Differential risk of remission and ESRD in childhood FSGS. Pediatr Nephrol 21:344–349
Abrantes MM, Cardoso LS, Lima EM, Penido Silva JM, Diniz JS, Bambirra EA, Oliveira EA (2006) Predictive factors of chronic kidney disease in primary focal segmental glomerulosclerosis. Pediatr Nephrol 21:1003–1012
Kamei K, Ishikura K, Sako M, Ito S, Nozu K, Iijima K (2020) Rituximab therapy for refractory steroid-resistant nephrotic syndrome in children. Pediatr Nephrol 35:17–24
Ishikura K, Matsumoto S, Sako M, Tsuruga K, Nakanishi K, Kamei K, Saito H, Fujinaga S, Hamasaki Y, Chikamoto H, Ohtsuka Y, Komatsu Y, Ohta T, Nagai T, Kaito H, Kondo S, Ikezumi Y, Tanaka S, Kaku Y, Iijima K, Japanese Society for Pediatric Nephrology; Japanese Society for Pediatric Nephrology (2015) Clinical practice guideline for pediatric idiopathic nephrotic syndrome 2013: medical therapy. Clin Exp Nephrol 19:6–33
Khwaja A (2012) KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120:c179–c184
Fujinaga S, Nishino T, Umeda C, Tomii Y, Watanabe Y, Sakuraya K (2019) Long-term outcomes after early treatment with rituximab for Japanese children with cyclosporine- and steroid-resistant nephrotic syndrome. Pediatr Nephrol 34:353–357
Fujinaga S, Ohtomo Y, Umino D, Takemoto M, Shimizu T, Yamashiro Y, Kaneko K (2007) A prospective study on the use of mycophenolate mofetil in children with cyclosporine-dependent nephrotic syndrome. Pediatr Nephrol 22:71–76
Maas RJ, Deegens JK, Smeets B, Moeller MJ, Wetzels JF (2016) Minimal change disease and idiopathic FSGS: manifestations of the same disease. Nat Rev Nephrol 12:768–776
Rheault MN, Zhang L, Selewski DT, Kallash M, Tran CL, Seamon M, Katsoufis C, Ashoor I, Hernandez J, Supe-Markovina K, D’Alessandri-Silva C, DeJesus-Gonzalez N, Vasylyeva TL, Formeck C, Woll C, Gbadegesin R, Geier P, Devarajan P, Carpenter SL, Kerlin BA, Smoyer WE, Midwest Pediatric Nephrology Consortium (2015) AKI in children hospitalized with nephrotic syndrome. Clin J Am Soc Nephrol 10:2110–2118
Sato M, Ishikura K, Ando T, Kikunaga K, Terano C, Hamada R, Ishimori S, Hamasaki Y, Araki Y, Gotoh Y, Nakanishi K, Nakazato H, Matsuyama T, Iijima K, Yoshikawa N, Ito S, Honda M (2019) Prognosis and acute complications at the first onset of idiopathic nephrotic syndrome in children: a nationwide survey in Japan (JP-SHINE study). Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfz185
Fujinaga S, Kusaba K (2019) Impact of acute kidney injury at the onset of idiopathic nephrotic syndrome in Japanese children. Clin Exp Nephrol 23:1171–1172
Joachim GR, Cameron JS, Schwartz M, Becker EL (1964) Selectivity of protein excretion in patients with the nephrotic syndrome. J Clin Invest 43:2332–2346
Cameron JS, White RH (1965) Selectivity of proteinuria in children with the nephrotic syndrome. Lancet 1:463–465
Bazzi C, Petrini C, Rizza V, Arrigo G, D'Amico G (2000) A modern approach to selectivity of proteinuria and tubulointerstitial damage in nephrotic syndrome. Kidney Int 58:1732–1741
Corwin HL, Schwartz MM, Lewis EJ (1988) The importance of sample size in the interpretation of the renal biopsy. Am J Nephrol 8:85–89
Acknowledgments
The authors wish to thank Dr. Hitohiko Murakami (Division of Pathology, Saitama Children’s Medical Center) for his great contributions to this study.
Funding
SF has received clinical research funding B at Saitama Children’s Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Research Committee and/or National Research Committee at which the study was conducted (approval number 2019-03-009) with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Watanabe, Y., Fujinaga, S., Endo, A. et al. Baseline characteristics and long-term outcomes of steroid-resistant nephrotic syndrome in children: impact of initial kidney histology. Pediatr Nephrol 35, 2377–2381 (2020). https://doi.org/10.1007/s00467-020-04760-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04760-8