Abstract
Background
Minimal change disease (MCD) is characterized by a nephrotic syndrome usually steroid-sensitive and a high incidence of relapse of proteinuria. Previous cohort studies have reported conflicting results regarding the association between the time to remission and incidence of relapse.
Methods
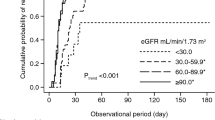
This multicenter prospective cohort study included 102 adult patients with steroid-sensitive MCD or focal segmental glomerulosclerosis from a 5-year cohort study of primary nephrotic syndrome, the Japan Nephrotic Syndrome Cohort Study, who achieved remission of proteinuria within 2 months of immunosuppressive therapy (IST). The association between the time to remission of proteinuria after immunosuppressive therapy and incidence of relapse was assessed using Cox proportional hazards models adjusted for clinically relevant factors.
Results
Remission was observed at 3–7, 8–14, 15–21, 22–28, and 30–56 days after initiation of immunosuppressive therapy in 17 (16.7%), 37 (36.3%), 21 (20.6%), 13 (12.7%), and 14 (13.7%) patients, respectively. During a median observation period of 2.3 years after the end of the 2nd month after initiation of immunosuppressive therapy, 46 (45.1%) patients relapsed. The time to remission was associated with the incidence of relapse in an inverse U-shaped pattern (multivariable-adjusted hazard ratios [95% confidence intervals] of the time to remission of 3–7, 8–14, 15–21, 22–28, 30–56 days: 1.00 [reference], 1.76 [0.56, 5.51], 6.06 [1.85, 19.80], 5.46 [1.44, 20.64], and 2.19 [0.52, 9.30], respectively).
Conclusion
The time to remission was identified as a significant predictor of relapse in steroid-sensitive patients.


Similar content being viewed by others
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available because the JNSCS data are not open to the public.
Code availability
Not applicable.
References
Vivarelli M, Massella L, Ruggiero B, Emma F (2017) Minimal change disease. Clin J Am Soc Nephrol 12:332–345. https://doi.org/10.2215/CJN.05000516
Yokoyama H, Taguchi T, Sugiyama H, Sato H (2012) Membranous nephropathy in Japan: analysis of the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol 16:557–563. https://doi.org/10.1007/s10157-012-0593-7
Lee H, Yoo KD, Oh YK et al (2016) Predictors of relapse in adult-onset nephrotic minimal change disease. Medicine 95:e3179. https://doi.org/10.1097/MD.0000000000003179
Park S, Rim SJ, Lee JH (2018) Associations between dietary behaviours and perceived physical and mental health status among Korean adolescents. Nutr Diet 75:488–493. https://doi.org/10.1111/1747-0080.12444
Nolasco F, Stewart Cameron J, Heywood EF et al (1986) Adult-onset minimal change nephrotic syndrome: a long-term follow-up. Kidney Int 29:1215–1223. https://doi.org/10.1038/ki.1986.130
Shinzawa M, Yamamoto R, Nagasawa Y et al (2013) Age and prediction of remission and relapse of proteinuria and corticosteroid-related adverse events in adult-onset minimal-change disease: a retrospective cohort study. Clin Exp Nephrol 17:839–847. https://doi.org/10.1007/s10157-013-0793-9
Han H, Wang S, Liang Y et al (2018) Respiratory tract infection: a risk factor for the onset and relapse of adult-onset minimal change disease in Southern China. Biomed Res Int 2018:1657208. https://doi.org/10.1155/2018/1657208
Fenton A, Smith SW, Hewins P (2018) Adult minimal-change disease: observation data from a UK centre on patient characteristics, therapies, and outcomes. BMC Nephrol 19:207. https://doi.org/10.1186/s12882-018-0999-x
Stefan G, Busuioc R, Stancu S et al (2021) Adult-onset minimal change disease: the significance of histological chronic changes for clinical presentation and outcome. Clin Exp Nephrol 25:240–250. https://doi.org/10.1007/s10157-020-01985-7
Yamamoto R, Imai E, Maruyama S et al (2018) Regional variations in immunosuppressive therapy in patients with primary nephrotic syndrome: the Japan nephrotic syndrome cohort study. Clin Exp Nephrol 22:1266–1280. https://doi.org/10.1007/s10157-018-1579-x
Niihata K, Nishiwaki H, Kurita N et al (2019) Variations in actual practice patterns and their deviations from the clinical practice guidelines for nephrotic syndrome in Japan: certified nephrologists’ questionnaire survey. Clin Exp Nephrol 23:1288–1297. https://doi.org/10.1007/s10157-019-01772-z
Shinzawa M, Yamamoto R, Nagasawa Y et al (2014) Comparison of methylprednisolone plus prednisolone with prednisolone alone as initial treatment in adult-onset minimal change disease: a retrospective cohort study. Clin J Am Soc Nephrol 9:1040–1048. https://doi.org/10.2215/CJN.12331213
Mak SK, Short CD, Mallick NP (1996) Long-term outcome of adult-onset minimal-change nephropathy. Nephrol Dial Transplant 11:2192–2201. https://doi.org/10.1093/oxfordjournals.ndt.a027136
Korbet SM, Whittier WL (2019) Management of adult minimal change disease. Clin J Am Soc Nephrol 14:911–913. https://doi.org/10.2215/CJN.01920219
Arias LF, Franco-Alzate C, Rojas SL (2011) Tip variant of focal segmental glomerulosclerosis: outcome and comparison to “not otherwise specified” variant. Nephrol Dial Transplant 26:2215–2221. https://doi.org/10.1093/ndt/gfq668
Deegens JKJ, Steenbergen EJ, Borm GF, Wetzels JFM (2008) Pathological variants of focal segmental glomerulosclerosis in an adult Dutch population—epidemiology and outcome. Nephrol Dial Transplant 23:186–192. https://doi.org/10.1093/ndt/gfm523
Ahn W, Bomback AS (2020) Approach to diagnosis and management of primary glomerular diseases due to podocytopathies in adults: core curriculum 2020. Am J Kidney Dis 75:955–964. https://doi.org/10.1053/j.ajkd.2019.12.019
Yamamoto R, Imai E, Maruyama S et al (2020) Incidence of remission and relapse of proteinuria, end-stage kidney disease, mortality, and major outcomes in primary nephrotic syndrome: the Japan Nephrotic Syndrome Cohort Study (JNSCS). Clin Exp Nephrol 24:526–540. https://doi.org/10.1007/s10157-020-01864-1
D’Agati VD, Fogo AB, Bruijn JA, Jennette JC (2004) Pathologic classification of focal segmental glomerulosclerosis: a working proposal. Am J Kidney Dis 43:368–382. https://doi.org/10.1053/j.ajkd.2003.10.024
Matsuo S, Imai E, Horio M et al (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992. https://doi.org/10.1053/j.ajkd.2008.12.034
Nishi S, Ubara Y, Utsunomiya Y et al (2016) Evidence-based clinical practice guidelines for nephrotic syndrome 2014. Clin Exp Nephrol 20:342–370. https://doi.org/10.1007/s10157-015-1216-x
Rovin BH, Caster DJ, Cattran DC et al (2019) Management and treatment of glomerular diseases (part 2): conclusions from a Kidney Disease: improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int 95:281–295. https://doi.org/10.1016/j.kint.2018.11.008
Wada T, Ishimoto T, Nakaya I et al (2021) A digest of the evidence-based clinical practice guideline for nephrotic syndrome 2020. Clin Exp Nephrol 25:1277–1285. https://doi.org/10.1007/s10157-021-02098-5
Hoyer PF, Brodehl J (2006) Initial treatment of idiopathic nephrotic syndrome in children: prednisone versus prednisone plus cyclosporine A: a prospective, randomized trial. J Am Soc Nephrol 17:1151–1157. https://doi.org/10.1681/ASN.2005090922
Shirai S, Imai N, Sueki S et al (2018) Combined cyclosporine and prednisolone therapy using cyclosporine blood concentration monitoring for adult patients with new-onset minimal change nephrotic syndrome: a single-center pilot randomized trial. Clin Exp Nephrol 22:283–290. https://doi.org/10.1007/s10157-017-1443-4
Eguchi A, Takei T, Yoshida T et al (2010) Combined cyclosporine and prednisolone therapy in adult patients with the first relapse of minimal-change nephrotic syndrome. Nephrol Dial Transplant 25:124–129. https://doi.org/10.1093/ndt/gfp422
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerular Diseases Work Group (2021) KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int 100:S1–S276. https://doi.org/10.1016/j.kint.2021.05.021
Teeninga N, Guan Z, Stevens J et al (2016) Population pharmacokinetics of prednisolone in relation to clinical outcome in children with nephrotic syndrome. Ther Drug Monit 38:534–545. https://doi.org/10.1097/FTD.0000000000000308
Schijvens AM, ter Heine R, de Wildt SN, Schreuder MF (2019) Pharmacology and pharmacogenetics of prednisone and prednisolone in patients with nephrotic syndrome. Pediatr Nephrol 34:389–403. https://doi.org/10.1007/s00467-018-3929-z
Acknowledgements
JNSCS was supported by a Grant-in-Aid for intractable Renal Diseases Research, Research on rare and intractable diseases, Health and Labour Sciences Research Grants for the Ministry of Health, Labor, and Welfare of Japan. JNSCS has been supported by a large number of investigators in 56 participating facilities; Hokkaido University Hospital, Sapporo, Hokkaido (Saori Nishio, Yasunobu Ishikawa, Daigo Nakazawa, and Tasuku Nakagaki); JCHO Sendai Hospital, Sendai, Miyagi (Toshinobu Sato, Mitsuhiro Sato, and Satoru Sanada); Tohoku University Hospital, Sendai, Miyagi (Hiroshi Sato, Mariko Miyazaki, Takashi Nakamichi, Tae Yamamoto, Kaori Narumi, and Gen Yamada); Yamagata University Hospital, Yamagata, Yamagata (Tsuneo Konta, and Kazunobu Ichikawa); Fukushima Medical University Hospital, Fukushima, Fukushima (Junichiro James Kazama, Tsuyoshi Watanabe, Koichi Asahi, Yuki Kusano, and Kimio Watanabe); University of Tsukuba Hospital, Tsukuba, Ibaraki (Kunihiro Yamagata, Joichi Usui, Shuzo Kaneko, and Tetsuya Kawamura); Gunma University Hospital, Maebashi, Gunma (Keiju Hiromura, Akito Maeshima, Yoriaki Kaneko, Hidekazu Ikeuchi, Toru Sakairi, and Masao Nakasatomi); Saitama Medical Center, Saitama Medical University, Kawagoe, Saitama (Hajime Hasegawa, Takatsugu Iwashita, Taisuke Shimizu, Koichi Kanozawa, Tomonari Ogawa, Kaori Takayanagi, and Tetsuya Mitarai); Department of Nephrology, Saitama Medical University, Irumagun, Saitama (Hirokazu Okada, Tsutomu Inoue, Hiromichi Suzuki, and Kouji Tomori); Tokyo Women’s Medical University, Shinjuku-ku, Tokyo (Kosaku Nitta, Takahito Moriyama, Akemi Ino, and Masayo Sato); Teikyo University School of Medicine, Itabashi-ku, Tokyo (Shunya Uchida, Hideaki Nakajima, Hitoshi Homma, Nichito Nagura, Yoshifuru Tamura, Shigeru Shibata, and Yoshihide Fujigaki); Juntendo Faculty of Medicine, Bunkyo-ku, Tokyo (Yusuke Suzuki, Yukihiko Takeda, Isao Osawa, and Teruo Hidaka); St. Marianna University, Kawasaki, Kanagawa (Daisuke Ichikawa, Yugo Shibagaki, Sayuri Shirai, Tsutomu Sakurada, Tomo Suzuki, and Mikako Hisamichi); Niigata University Medical and Dental Hospital, Niigata, Niigata (Ichiei Narita, Naohumi Imai, Yumi Ito, Shin Goto, Yoshikatsu Kaneko, and Rhohei Kaseda); Kanazawa Medical University, Uchinada, Ishikawa (Hitoshi Yokoyama, Keiji Fujimoto, and Norifumi Hayashi); Kanazawa University Hospital, Kanazawa, Ishikawa (Takashi Wada, Miho Shimizu, Kengo Furuichi, Norihiko Sakai, Yasunori Iwata, Tadashi Toyama, and Shinji Kitajima); National Hospital Organization Kanazawa Medical Center, Kanazawa, Ishikawa (Kiyoki Kitagawa); Ogaki Municipal Hospital, Ogaki, Gifu (Hiroshi Sobajima, Norimi Ohashi, So Oshitani, and Kiyohito Kawashima); Gifu Prefectural Tajimi Hospital, Tajimi, Gifu (Tetsushi Mimura); Hamamatsu University Hospital, Hamamatsu, Shizuoka (Hideo Yasuda, Akira Hishida, and Yoshihide Fujigaki); Shizuoka General Hospital, Shizuoka, Shizuoka (Satoshi Tanaka, and Noriko Mori); Chutoen General Medical Center, Kakegawa, Shizuoka (Toshiyuki Akahori, and Yutaka Fujita); Nagoya University Graduate School of Medicine, Nagoya, Aichi (Shoichi Maruyama, Naotake Tsuboi, Tomoki Kosugi, Takuji Ishimoto, Takayuki Katsuno, Noritoshi Kato, and Waichi Sato); Japanese Red Cross Nagoya Daini Hospital, Nagoya, Aichi (Asami Takeda, Kunio Morozumi, Yasuhiro Ohtsuka, Hibiki Shinjo, and Akihito Tanaka); Fujita Health University School of Medicine, Toyoake, Aichi (Hiroki Hayashi, Yukio Yuzawa, Midori Hasegawa, Daijo Inaguma, Shigehisa Koide, and Kazuo Takahashi); Konan Kosei Hospital, Konan, Aichi (Takeyuki Hiramatsu, Shinji Furuta, and Hideaki Ishikawa); Anjo Kosei Hospital, Anjo, Aichi (Hirofumi Tamai, and Takatoshi Morinaga); Ichinomiya Municipal Hospital, Ichinomiya, Aichi (Arimasa Shirasaki, Toshiki Kimura, and Mina Kato); Japanese Red Cross Nagoya Daiichi Hospital, Nagoya, Aichi (Shizunori Ichida, and Nobuhide Endo); Kasugai Municipal Hospital, Kasugai, Aichi (Tomohiko Naruse, Yuzo Watanabe, and Yosuke Saka); Kainan Hospital, Yatomi, Aichi (Satashi Suzuki, Michiko Yamazaki, and Rieko Morita); Masuko Memorial Hospital, Nagoya, Aichi (Kunio Morozumi, Kunio Morozumi, Kaoru Yasuda, Chika Kondo, Takahiro Morohiro, Rho Sato, and Yuichi Shirasawa); Chubu Rosai Hospital, Nagoya, Aichi (Yoshiro Fujita, Hideaki Shimizu, and Tatsuhito Tomino); Handa City Hospital, Handa, Aichi (Makoto Mizutani); Yokkaichi Municipal Hospital, Yokkaichi, Mie (Yosuke Saka, Hiroshi Nagaya, and Makoto Yamaguchi); Kitano Hospital, Osaka, Osaka (Tatsuo Tsukamoto, Eri Muso, Hiroyuki Suzuki, Tomomi Endo, and Hiroko Kakita); Toyonaka Municipal Hospital, Toyonaka, Osaka (Megumu Fukunaga); Osaka General Medical Center, Osaka, Osaka (Tatsuya Shoji, and Terumasa Hayashi); Osaka City University Hospital, Osaka, Osaka (Eiji Ishimura, Akihiro Tsuda, Shinya Nakatani, Ikue Kobayashi, Mitsuru Ichii, Akinobu Ochi, and Yoshiteru Ohno); Osaka University Hospital, Suita, Osaka (Yoshitaka Isaka, Enyu Imai, Yasuyuki Nagasawa, Hirotsugu Iwatani, Ryohei Yamamoto, and Tomoko Namba); Kobe University Hospital, Kobe, Hyogo (Shunsuke Goto MD, and Shinichi Nishi); Nara Medical University Hospital, Kashihara, Nara (Yasuhiro Akai, Ken-ichi Samejima, Masaru Matsui, Miho Tagawa, Kaori Tanabe, and Hideo Tsushima); Wakayama Medical University Hospital, Wakayama, Wakayama (Takashi Shigematsu MD, Masaki Ohya, Shigeo Negi, and Toru Mima); Shimane University Hospital, Izumo, Shimane (Takafumi Ito); Okayama University Hospital, Okayama, Okayama (Hitoshi Sugiyama, Keiko Tanaka, Toshio Yamanari, Masashi Kitagawa, Akifumi Onishi, and Koki Mise); Kawasaki Medical School, Kurashiki, Okayama (Naoki Kashihara, Tamaki Sasaki, Sohachi Fujimoto, and Hajime Nagasu); Graduate School of Medicine, The University of Tokushima,Tokushima,Tokushima (Kojiro Nagai, and Toshio Doi); Kagawa University, Miki-cho, Takamatsu, Japan (Tadashi Sofue, Hideyasu Kiyomoto, Kumiko Moriwaki, Taiga Hara, Yoko Nishijima, Yoshio Kushida, and Tetsuo Minamino); Kochi Medical School, Kochi University, Nankoku, Kochi (Yoshio Terada, Taro Horino, Yoshinori Taniguchi, Kosuke Inoue, Yoshiko Shimamura, and Tatsuki Matsumoto); Kyushu University Hospital, Fukuoka, Fukuoka (Kazuhiko Tsuruya, Hisako Yoshida, Naoki Haruyama, Shunsuke Yamada, Akihiro Tsuchimoto, and Yuta Matsukuma); Fukuoka University Hospital, Fukuoka, Fukuoka (Kosuke Masutani, Yasuhiro Abe, Aki Hamauchi, Tetsuhiko Yasuno, and Kenji Ito); Kurume University Hospital, Kurume, Fukuoka (Kei Fukami, Junko Yano, Chika Yoshida, Yuka Kurokawa, and Nao Nakamura); National Hospital Organization Fukuokahigashi Medical Center, Koga, Fukuoka (Ritsuko Katafuchi, Hiroshi Nagae, Shumei Matsueda, and Kazuto Abe); Nagasaki University Hospital, Nagasaki, Nagasaki (Tomoya Nishino, Tadashi Uramatsu, and Yoko Obata); Miyazaki University Hospital, Miyazaki, Miyazaki (Shouichi Fujimoto, Yuji Sato, Masao Kikuchi, Ryuzo Nishizono, Takashi Iwakiri, and Hiroyuki Komatsu).
Funding
The JNSCS was supported by a Grant-in-Aid for Intractable Renal Diseases Research, Research on Rare and Intractable Diseases, Health and Labor Sciences Research Grants for the Ministry of Health, Labor, and Welfare of Japan.
Author information
Authors and Affiliations
Consortia
Contributions
Research idea and study design: IE, MS, and IY; data acquisition: all authors; data analysis/interpretation: YR; statistical analysis: YR; supervision or mentorship: IE, MS, and IY. Each author contributed important intellectual content during manuscript drafting and agrees to be personally accountable for the individual’s own contributions and to ensure that questions pertaining to the accuracy or integrity of any portion of the work, even one in which the author was not directly involved, are appropriately investigated and resolved, including with documentation in the literature if appropriate.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no relevant financial interests.
Ethics approval
The study protocol of the JNSCS was approved by the ethics committee of Osaka University Hospital (approval number 17035-4) and the institutional review board of each participating hospital.
Consent to participate
Informed consent was obtained from the participants from all hospitals, except one with an opt-out approach to obtain informed consent, according to the Japanese Ethical Guidelines for Medical and Health Research Involving Human Subjects.
Consent to publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Japan Nephrotic Syndrome Cohort Study investigators are listed in acknowledgements.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamamoto, R., Imai, E., Maruyama, S. et al. Time to remission of proteinuria and incidence of relapse in patients with steroid-sensitive minimal change disease and focal segmental glomerulosclerosis: the Japan Nephrotic Syndrome Cohort Study. J Nephrol 35, 1135–1144 (2022). https://doi.org/10.1007/s40620-022-01279-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-022-01279-z