Abstract
Background
Outcomes for severe hyperammonemia treated with renal replacement therapy (RRT) reported in the literature vary widely. This has created differing recommendations regarding when RRT is beneficial for hyperammonemic patients.
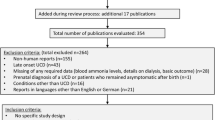
Methods
To evaluate our institution’s experience with RRT in pediatric patients with inborn errors of metabolism (IEMs) and potential prognostic indicators of a better or worse outcome, we performed a retrospective chart review of patients who received RRT for hyperammonemia. Our cohort included 19 patients with confirmed IEMs who received RRT between 2000 and 2017. Descriptive statistics are presented as medians with interquartile ranges with appropriate statistical testing assuming unequal variance.
Results
There were 16 males (84%) and 3 females (16%) identified for inclusion in this study. There were 9 survivors (47%) and 10 non-survivors (53%). The average age of survivors was 67 months (age range from 3 days to 15.6 years). The average age of non-survivors was 1.8 months (age range from 2 days to 18.7 months). Peak ammonia, ammonia on admission, and at RRT initiation were higher in non-survivors compared with survivors. Higher ammonia levels and no change in ammonia between admission and RRT initiation were associated with an increased risk of mortality.
Conclusions
Hyperammonemia affects two distinct patient populations; neonates with markedly elevated ammonia levels on presentation and older children who often have established IEM diagnoses and require RRT after failing nitrogen-scavenging therapy. Our experience demonstrates no significant change in mortality associated with neonatal hyperammonemia, which remains high despite improvements in RRT and intensive care.


Similar content being viewed by others
Data availability
The data presented in this submission is available upon request after de-identification beginning 3 months and ending 5 years following article publication. Proposals should be directed to corresponding author. To gain access, data requestors will need to sign a data access agreement and provide a methodologically sound proposal.
Abbreviations
- RRT:
-
Renal replacement therapy
- PD:
-
Peritoneal dialysis
- HD:
-
Hemodialysis
- CRRT:
-
Continuous renal replacement therapy
- IEM:
-
Inborn error of metabolism
- UCD:
-
Urea cycle disorder
- OA:
-
Organic acidemia
- GFR:
-
Glomerular filtration rate
References
Bachmann C (2003) Outcome and survival of 88 patients with urea cycle disorders: a retrospective evaluation. Eur J Pediatr 162(6):410–416
Nassogne MC, Héron B, Touati G, Rabier D, Saudubray JM (2005) Urea cycle defects: management and outcome. J Inherit Metab Dis 28(3):407–414
Msall M, Batshaw M, Suss R, Brusilow S, Mellits ED (1984) Neurologic outcome in children with inborn error of urea synthesis. N Engl J Med 310:1500–1505
Maestri NE, Hauser ER, Bartholomew D, Brusilow SW (1991) Prospective treatment of urea cycle disorders. J Pediatr 119(6):923–928
Unsinn C, Das A, Valayannopoulos V, Thimm E, Beblo S, Burlina A et al (2016) Clinical course of 63 patients with neonatal onset urea cycle disorders in the years 2001-2013. Orphanet J Rare Dis 11(1):1–11
Burgard P, Kölker S, Haege G, Lindner M, Hoffmann GF (2016) Neonatal mortality and outcome at the end of the first year of life in early onset urea cycle disorders—review and meta-analysis of observational studies published over more than 35 years. J Inherit Metab Dis 39(2):219–229
Kido J, Nakamura K, Mitsubuchi H, Ohura T, Takayanagi M, Matsuo M et al (2012) Long-term outcome and intervention of urea cycle disorders in Japan. J Inherit Metab Dis 35(5):777–785
Krivitzky L, Babikian T, Lee HS, Thomas NH, Burk-Paull KLBM (2009) Intellectual, adaptive, and behavioral functioning in children with urea cycle disorders. Pediatr Res 66(1):96–101
Surtees RA, Matthews EE, Leonard JV (1992) Neurologic outcome of propionic acidemia. Pediatr Neurol 8(5):333–337
McBryde KD, Kershaw DB, Bunchman TE, Maxvold NJ, Mottes TA, Kudelka TL et al (2006) Renal replacement therapy in the treatment of confirmed or suspected inborn errors of metabolism. J Pediatr 148(6):770–778
Picca S, Dionisi-Vici C, Abeni D, Pastore A, Rizzo C, Orzalesi M et al (2001) Extracorporeal dialysis in neonatal hyperammonemia: modalities and prognostic indicators. Pediatr Nephrol 16(11):862–867
Hediger N, Landolt MA, Diez-Fernandez C, Huemer M, Häberle J (2018) The impact of ammonia levels and dialysis on outcome in 202 patients with neonatal onset urea cycle disorders. J Inherit Metab Dis 41(4):689–698
Donn SM, Swartz RD, Thoene JG (1979) Comparison of exchange transfusion, peritoneal dialysis, and hemodialysis for the treatment of hyperammonemia in an anuric newborn infant. J Pediatr 95(1):67–70
Wong KY, Wong SN, Lam SY, Tam S, Tsoi NS (1998) Ammonia clearance by peritoneal dialysis and continuous arteriovenous hemodiafiltration. Pediatr Nephrol 12(7):589–591
Picca S, Dionisi-Vici C, Bartuli A, De Palo T, Papadia F, Montini G et al (2015) Short-term survival of hyperammonemic neonates treated with dialysis. Pediatr Nephrol 30(5)
Pela I, Seracini D, Donati MA, Lavoratti G, Pasquini E, Materassi M (2008) Peritoneal dialysis in neonates with inborn errors of metabolism: is it really out of date? Pediatr Nephrol 23(1):163–168
Häberle J, Burlina A, Chakrapani A, Dixon M, Karall D, Lindner M et al (2019) Suggested guidelines for the diagnosis and management of urea cycle disorders: first revision. J Inherit Metab Dis 42(6):1192–1230
Cho H (2019) Renal replacement therapy in neonates with an inborn error of metabolism. Korean J Pediatr 62(2):43–47
Demirkol D, Aktuğlu Zeybek Ç, Karacabey BN, Cesur Y, Ataman Y, Soysal E (2019) The role of supportive treatment in the management of hyperammonemia in neonates and infants. Blood Purif:1–8
Schwartz GJ, Haycock GB, Edelmann CM, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics. 58(2):259–263
Su SW, Stonestreet BS (2010) Core concepts: neonatal glomerular filtration rate. Neoreviews. 11(12):e714–e721
Ripley B, Venables B, Bates D, Hornik K, Gebhardt A, Firth D. MASS: Modern Applied Statistics with S [Internet]. R package version 3.5.1. 2019. Available from: https://cran.r-project.org/package=MASS
Aragon T, Fay M, Wollschlaeger D, Omidpanah A. Epitools: Epidemiology Tools [Internet]. R package version 3.5.1. 2017. Available from: https://cran.r-project.org/package=epitools
Wickham H, Chang W, Henry L, Pedersen T, Takahashi K, Wilke C, et al. ggplot2: Create elegant data visualisations using the grammar of graphics [Internet]. R package version 3.5.1. 2019. Available from: https://cran.r-project.org/package=ggplot2
Porta F, Peruzzi L, Bonaudo R, Pieretti S, Busso M, Cocchi E et al (2018) Differential response to renal replacement therapy in neonatal-onset inborn errors of metabolism. Nephrol. 23(10):957–961
Held PK, Haynes CA, De Jesús VR, Baker MW (2014) Development of an assay to simultaneously measure orotic acid, amino acids, and acylcarnitines in dried blood spots. Clin Chim Acta 436:149–154
Janzen N, Terhardt M, Sander S, Demirkol M, Gökçay G, Peter M et al (2014) Towards newborn screening for ornithine transcarbamylase deficiency: fast non-chromatographic orotic acid quantification from dried blood spots by tandem mass spectrometry. Clin Chim Acta 430:28–32
Vergano SA, Crossette JM, Cusick FC, Desai BR, Deardorff MA, Sondheimer N (2013) Improving surveillance for hyperammonemia in the newborn. Mol Genet Metab 110(1–2):102–105
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest for the authors.
Prior presentation of data
Subsets of the data reported in this manuscript have been presented at annual meetings of the Pediatric Academic Society in 2015 and the American College of Medical Genetics in 2018.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ames, E.G., Luckritz, K.E. & Ahmad, A. A retrospective review of outcomes in the treatment of hyperammonemia with renal replacement therapy due to inborn errors of metabolism. Pediatr Nephrol 35, 1761–1769 (2020). https://doi.org/10.1007/s00467-020-04533-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-020-04533-3