Abstract
Background
Medication-related problems (MRPs) are the undesirable effects of pharmacotherapy that can potentially lead to harm. The epidemiology of MRPs in paediatric renal patients is unknown. We aimed to characterise MRPs in this population at two tertiary care hospitals in the UK.
Methods
Prescription charts for children (≤18 years) were reviewed to identify MRPs, and characterised using a specific proforma with a standard operational definition. MRP predictors were evaluated by logistic regression and severity was assessed using a validated scale.
Results
Two hundred and sixty-seven MRPs were identified from 266 prescription chart reviews. The incidence was 51.2 % (203 MRPs, 166 charts; 95 % CI 43.2–60.6 %) of hospitalised patients and 32 % (64 MRPs, 100 charts; 95 % CI 22.9–41.1 %) in outpatients. The number of prescribed medications was the only independent predictor during inpatient treatment (OR 1.06, 95 % CI 1.02–1.10, p = 0.002) with no significant predictors identified at outpatient clinics. The severity level of the MRPs was minor: 53.9 %, (144 out of 267); or moderate: 46.1 %, (123 out of 267). Sub-optimal drug effect was the predominant MRP (inpatient: 68 %; outpatient: 39 %). Prescribing error and patients' medicine-taking behaviour were the main contributory factors. The majority of the MRPs in the inpatient setting were resolved.
Conclusion
Many factors are associated with MRPs in children; the associations are cumulative and interdependent. Investment in preventive strategies and extending the support from the acute health care setting into the community are invaluable for optimising pharmacotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medications are prescribed with the intention of benefiting the patient. However, the use of medications can be undesirable and potentially lead to harm. These undesirable effects are known as medication-related problems (MRPs). A MRP is defined as an event involving pharmacotherapy that interferes with the patient experiencing an optimal outcome of medical care [1]. Medications for patients with kidney disease are specialised and complex. In those with chronic kidney disease (CKD), the relevance of optimal pharmacotherapy management is even more critical, thus putting this group of children at risk of developing MRPs. The National Kidney Foundation/Kidney Dialysis Outcome Quality Indicator (NKF/KDOQI) guideline recommends that a medication review should be performed for children and adolescents at all visits for the prevention of MRPs such as inappropriate doses, inadequate therapeutic monitoring and potentially adverse drug effects on the kidney or disease complications [2].
Medication-related problems are common in children: recent studies have reported that the incidence in the UK is 39.4 % in hospitalised children [3] and 2.7 % of children on medications were admitted to the emergency departments in the UK [4]. However, these studies did not include paediatric renal patients. Current management of MRPs in this group is based on what has been learned from adult studies [5], which may be unrepresentative of the paediatric population. We have previously reported on the paucity of data on the epidemiology of MRPs in children with kidney disease and suggested further studies for proactive strategies in medication safety [5]. This current study aimed to determine the characteristics of MRPs and potential risk factors for their occurrence in children with kidney disease at the tertiary renal centres.
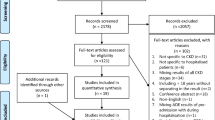
Materials and methods
Setting and study subjects
Two observational cohort studies were conducted at the renal unit of the Evelina London Children’s Hospital (ELCH) and Great Ormond Street Hospital for Children (GOSH). Study 1 was conducted in an inpatient setting at ELCH and GOSH and study 2 was conducted in the renal outpatient clinics at ELCH. Approval was obtained from the Research Ethics Committee, UK. Both hospitals are two of the largest children’s renal centres and provide tertiary care to approximately 40 % of children requiring renal replacement therapy (RRT) in the UK [6]. The renal units are led by teams of paediatric nephrologists, supported by a team of healthcare professionals including specialist renal nurses, renal pharmacists and nutritionists. The cases seen in both units include all aspects of paediatric renal disease, including RRT.
Study 1, inpatient setting
The clinical team in both hospitals conducted daily a full patient review and clinical rounds. Clinical pharmacy practice is established as standard care in the inpatient setting; this enabled the pharmacists to review prescription charts as a standard clinical routine. Prescription chart review was conducted using paper documentation in ELCH and from an electronic prescribing system (ePS) in GOSH.
Study 2, outpatient clinic setting
The renal outpatient clinics in ELCH operate daily on weekdays. Patients’ clinic notes and medication lists were documented on a multidisciplinary electronic medical record (eMR). Unlike the inpatient setting, clinical pharmacy practice is not part of the standard care and thus, prescription chart review was not routine for all patients attending the clinic.
The inclusion criteria for both studies were the same: all children aged 18 years and younger, who had received at least one long-term (non-acute) medication. Additionally, children who were included in the inpatient study had to have been hospitalised for at least 24 h.
Data collection
Study 1, inpatient study
Data were collected for hospitalised patients at ELCH and GOSH from 1 December 2011 to 1 September 2012. At each site, one pharmacist was responsible for the detection of MRPs using a structured tool and prospective prescription chart review method during routine clinical practice. Recommendations on the resolution of the MRPs were discussed with the clinical team during clinical rounds; this method has been used in previous paediatric MRP studies [3, 4, 7, 8].
Study 2, outpatient clinic study
Data were collected at ELCH from 18 February to 18 September 2013. As clinical pharmacy practice was not a standard care at the outpatient clinic and in order to ensure the consistency of data, one researcher was responsible for identifying MRPs from the eMR, using a structured approach. In the event that an MRP with potential harm to the patient was identified, the researcher would alert the clinical team.
The two pharmacists who were involved in collecting the data in the inpatient setting had received similar professional training and each had more than 10 years’ experience in tertiary paediatric renal pharmacy practice. The researcher is also a qualified pharmacist trained in renal pharmacy, but not working in the capacity of a pharmacist within the Trusts. The pharmacists and the researcher received training on the definition and characteristics of MRPs before initiation of the research. All MRPs were recorded onto a proforma using a standard code and operational definition (Appendix 1). All prescribed medications associated with MRPs were classified according to the World Health Organisation Anatomical Therapeutic Chemical (WHO-ATC) system.
All different medications prescribed throughout the patients’ hospital stay (in study 1) and all medications listed in the patient’s clinic notes (in study 2) were recorded.
Incidence and risk factors
The incidence of MRPs in the study cohort was defined as the number of patients with at least one MRP identified during prescription chart review, divided by the total number of patients reviewed multiplied by 100. For MRP incidence and risk factor calculations, only the first event of MRP identified during review was considered for investigating the association between MRP incidence and potential risk factors.
Analysis of MRP severity
Similar to previously published paediatric MRP studies [3, 9] this project adopted a validated severity scoring tool for medication errors [10]. The MRPs were independently assessed by four health care professionals comprising a paediatric nephrology consultant, paediatric consultant pharmacist, medication safety pharmacist and a specialist renal nurse. The MRPs were assessed in terms of clinical significance, with scores ranging from 0 to 10 using a visual analogue scale, where 0 represented a case with no potential harm and 10 represented a case that would result in death. An MRP was considered minor (unlikely to have any adverse effects) if the score was < 3, moderate (likely to cause some adverse effects or interfere with therapeutic goals) if the score was between 3 and 7, or severe (likely to cause lasting impairment or death) if the score was > 7. The mean severity score (μScore) from all assessors was the final score assigned to each MRP.
Classification of medications and MRPs
The medications that were associated with MRPs were classified according to the WHO-ATC system. The identified MRPs were documented in a specified proforma adapted from the Pharmaceutical Care Network Europe (PCNE) MRP Classification Scheme [11]. The operational definition of the types and contributory factors of MRPs is available in Appendix 1.
MRP resolution
Prescription review was not standard clinical practice in the outpatient clinic; thus, corrective measures and resolution rates could only feasibly be evaluated for MRPs identified during study 1, in the inpatient setting. A MRP was defined as “solved” on occasions when actions were taken before causing any harm to patients or actions were taken to solve an ongoing MRP.
Statistics
Data were analysed using the Statistical Package for Social Science (SPSS) version 21 and presented as percentages (%), mean with standard deviation (SD) or median with interquartile range (IQR 1–3) and odds ratios (OR) with 95 % confidence interval (CI). For the descriptive analysis of patient and MRP characteristics, Chi-squared (χ 2), Kruskal–Wallis, Rank and Mann–Whitney tests were used as appropriate. In all statistical tests p values of less than 0.05 were considered statistically significant.
Multivariate logistic regression was performed to assess the impact of predictors on the likelihood MRPs would occur among the study population. The regression worked around one binary outcome (at least one MRP identified: yes/no) and six independent variables: age (years), gender, number of medications prescribed (Rx) and types of RRT (dialysis, post-transplant and non-RRT). The variable Rx refers to the number of different medications that were prescribed during the data collection period. Additional independent variables analysed in the inpatient study were length of hospital stay in days (LOS) and types of ward admission (elective or non-elective). Elective admission refers to scheduled admission to the ward for inpatient treatment or procedure. Non-elective admission refers to cases transferred from other wards or hospitals for continuation of care. The factors that were analysed in the regression analyses included those found to be relevant in the literature and of pathophysiological significance [3, 12–14].
Results
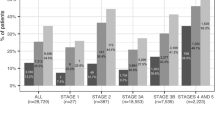
A total of 227 patients fulfilled the inclusion criteria and 267 MRPs were identified (Inpatient, n = 127 patients, 203 MRPs (mean 1.2 MRPs per patient (SD 2); Outpatient, n = 100 patients, 64 MRPs (mean 0.6 MRPs per patient (SD 1.4)). All MRPs were included for analyses. The incidence of MRPs in the inpatient cohort was 19.2 % higher than the Outpatient cohort (51.2 %, 95 % CI 43.2 – 60.6 % vs. 32 %, 95 % CI 22.9 – 41.1 %, p = 0.04). The study results are summarised in Table 1.
Characteristics of the study population
The majority of patients were male. Inpatients were younger than the outpatient cohort (inpatient: median 6.6 years [IQR 1.8–12.5]; outpatient: median 9.7 (IQR 5.7–14.2), p = <0.001). Inpatients who developed MRPs, compared with those who did not, had a longer length of hospital stay (median 9 vs 4 days, p < 0.001), were on dialysis or had kidney transplant (p = 0.001) and more medications prescribed (p < 0.001; Table 2). Of the 127 inpatients, 6 were diagnosed with acute kidney injury (AKI). Of the 6 AKI cases, 1 was secondary to sepsis and another was due to the use of radio-contrast agent. The remaining 4 cases could not be confirmed to have any association with the use of medications as they had unknown causes.
Risk factors for MRPs
The number of medications prescribed per child was the single significant predictor for MRPs at the inpatient setting (OR 1.06, 95 % CI 1.02–1.10, p = 0.002). The odds ratio of 1.06 indicates that the chance of having an MRP is 6 % higher with every additional medication. There was a trend toward a higher prediction of MRPs in patients on dialysis compared with those not on dialysis, but this finding was not statistically significant. None of the predictors analysed here was statistically significant for the outpatient cohort.
MRP severity assessment
The 64 MRPs identified from the outpatient clinic scored higher on the severity scale compared with the 203 MRPs identified in the inpatient setting (μScore range: outpatient clinic: 2.1–5.8; inpatient 0.1–6.8).
Medications associated with MRPs
The groups of medicines most often associated with MRPs were those used for “alimentary tract and metabolism”, “systemic anti-infective” and “blood and blood forming organs” (Table 3). MRPs in inpatients were commonly reported with the use of nystatin 7.9 %, 16 out of 203), paracetamol (7.4 %, 15 out of 203) and ranitidine (5.4 %, 11 out of 203), whereas MRPs in outpatients were associated with prednisolone (15.6 %, 10 out of 64), sodium bicarbonate (9.4 %, 6 out of 64) and alfacalcidol (7.8 %, 5 out of 64).
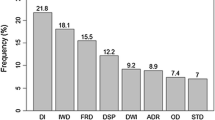
The types and contributory factors of MRPs
Sub-optimal drug effect was the predominant MRP identified in both clinical settings; however, their contributory factors were distinct. The characteristics of the MRPs are presented in Table 4.
Inpatient setting
The predominant MRPs were “sub-optimal drug effect” (21.7 %, 44 out of 203), “unnecessary treatment” (20.2 %, 41 out of 203) and “toxic adverse reaction” (19.2 %, 39 out of 203). The majority of the MRPs were identified and resolved before they caused any harm (55.1 %, 112 out of 203). Prescribing errors in the selection of medications and doses were the main contributory factors for the occurrence of MRPs. The following are examples of cases:
-
MRP1
Valganciclovir 400 mg once a day was prescribed post-transplant; the dose should have been optimised to 500 mg according to renal function (μScore 2.8).
-
MRP2
50 mcg stat dose of intravenous prazosin was prescribed to a neonate, but 500 mcg was administered (μScore 5.5).
-
MRP3
Intravenous gentamicin for septicaemia was prescribed for a patient with acute renal dysfunction; daily doses of gentamicin were continued for 2 weeks without the serum drug level being monitored (μScore 7.4).
Outpatient clinic
The predominant MRPs were “sub-optimal drug effect” (39.1 %, 25 out of 64), “drug administration problems” (29.7 %, 19 out of 64) and “non-allergic adverse drug events” (17.2 %, 11 out of 64). The contributory factors for MRPs were associated with patients’ medicine-taking behaviour and other factors (e.g. unwanted side effects and dependency on feeding tubes for the administration of medications). The following are examples of cases:
-
MRP1
A patient with vesicoureteric reflux was dependent on the enteral feeding tube. The family struggled to administer iron supplement (and other oral medications) as prescribed (μScore 2.1).
-
MRP2
Activated vitamin D for the prevention of hyperparathyroidism was prescribed to a patient with advanced kidney failure. The family had problems in obtaining a continuous supply in the community setting (μScore 3.9).
-
MRP3
A patient had on-going proteinuria, but had been non-compliant with treatment for the past 6 months (μScore 5.8).
MRP resolution
Of the 203 MRPs identified from the inpatient setting, 96 % (195 out of 203) were resolved as a result of multidisciplinary care. Most MRPs were resolved by changes to the medication selection, doses and dosing frequency. The pharmacists played an important role in providing consultations on medication regimens and 99.5 % of the recommendations (227 out of 228) were accepted by the clinical team.
Discussion
To our knowledge this is the first study investigating MRPs systematically in children with kidney disease in the UK. We observed that whilst not all predictors for MRPs were significant, our results are particularly important, not only in understanding the characteristics of MRPs in this population, but also in enabling the development of preventive strategies in clinical practice.
It is worth discussing further the differences in the demographic characteristics between study subjects in the inpatient and outpatient setting in the current research. Even though all subjects were children with kidney disease, the majority of those seen at the outpatient clinics were in the pre-dialysis stage. Our study shows that those receiving inpatient treatments require three times the numbers of medications than the outpatient cohort (median 17 vs 5 medications per child). Children receiving inpatient treatment were by definition more ill and this was likely due to more advanced disease or complications of RRT. Many studies in adults with CKD have previously demonstrated that patients at the late stage of CKD and on RRT require more complex pharmacotherapy and are exposed to increased chances of MRPs [15, 16]. There was an association between the occurrence of MRP and the length of hospital stay; however, further research is required to assess causality.
Interestingly, despite having more serious clinical conditions in hospitalised patients, the majority of MRPs were scored as minor (68 %, 138 out of 203) compared with the MRPs identified at the outpatient clinic in which 90.6 % (58 out of 64) were scored as moderate. The possible reason for this lies in the difference of care between tertiary care centres and the community. Problems in the use of medications occurring in inpatients are “active errors” [17]. Similar to previous paediatric medication error research [7, 8, 18, 19] the majority of the “active errors” in the current study were caused by prescribing errors. These errors could rapidly be rectified by the healthcare professionals and were less likely to cause harm as a result of the interventions. As an example, sub-optimal tacrolimus dose in the management of post-kidney transplantation on the ward could be adjusted from post-12-h tacrolimus serum drug levels. Changes to drug regimens are directly monitored and patients receiving inpatient treatment are likely to adhere to the prescribed therapy.
In contrast, drug problems occurring in the community are “latent errors”, most of which are caused by exogenous factors that are beyond the control of healthcare professionals [20]. An example of exogenous factors in the current research was difficulties in obtaining unlicensed and off-label medications from the community.
The types of medications associated with MRPs in our study portrayed the common prescribing pattern in the paediatric population [3, 21, 22]. However, medicines of the “blood and blood forming agents” are unique to MRPs in renal patients [12, 13, 23, 24]. The medications that were more often associated with MRPs were also those more often prescribed. It is also important to note that there are limited data available for the safe and effective doses of most medications used in children [3, 25]. This may contributed to the observed tendency for higher numbers of adverse drug events and other MRPs in this cohort.
It is a challenging task to determine an optimal and safe dose for children with kidney disease owing to their physiology and the altered pharmacokinetic properties of medications [21, 26]. The management of MRPs should be a shared responsibility of all healthcare providers. The MRP classifications and the MRP screening tool used in the present research could also be integrated into the physician’s practice.
Other strategies to reduce the occurrence of MRPs are to integrate medication reconciliation into patients’ medicine management program. This program was also recently highlighted for the care of adult renal patients [27, 28]. In the UK, a survey among paediatric pharmacists found that only 34 % had full medication reconciliation in place [29]. A policy on medication reconciliation on hospital admission and at discharge, including routine outpatient clinic appointments, minimises discrepancies in the transfer of information [3].
In the inpatient setting, we found that most MRPs are largely attributed to prescribing errors. Prescribing errors have been reported to be preventable; thus, having continuous awareness programmes on medication safety in paediatrics remains essential in practice [8, 29–32].
This study reported the rate of MRP occurrence in children who attended the renal outpatient clinic as less than one MRP per patient. Nevertheless, the potential harm as a consequence of these MRPs should not be underestimated. The latent effect of MRPs in this patient group has not been studied. We identified cases of poor treatment outcome due to patient non-adherence. An example of these cases that was highlighted earlier involved a patient with glomerulonephritis leading to persistent proteinuria.
Difficulties in obtaining medication supplies and poor understanding about medications among parents and children are among the factors causing low adherence in CKD [15, 33]. Thus, proper coordination of supplies of medication in the community is also vitally important and should be anticipated when unlicensed and/or off-label medications are prescribed for children. Continuous assessment on changing patients’ cognitive behaviour towards medicines and/or specific clinical outcomes is also important to empower patients’ involvement in managing their medications [15, 32, 34]. As caring for children with kidney disease is a life-long commitment, parents/carers would benefit from a support system to facilitate them in the monitoring, prevention and resolution of MRPs.
The strengths of this research lie in using multiple approaches to identifying MRPs, i.e. a prospective chart review in the inpatient setting and a retrospective chart review in the outpatient clinic. We were aware that the characteristics of MRPs identified in both studies reflect the types of methods used. Thus, appropriate measures had been taken to minimise the variability of data that include the use of a structured proforma with a standard operational definition and training to those involved in collecting the data. This research included two main referral centres for paediatric nephrology in London. Thus, the results may not necessarily be generalisable to other countries with different care settings.
Conclusion
Medication-related problems in children with kidney disease necessitate a comprehensive approach to their identification and resolution. The MRPs in different clinical settings are unique in their characteristics and levels of severity. Investment in preventive strategies and extending the support from the health care setting into the community are invaluable for optimising pharmacotherapy.
References
Hepler CD, Strand LM (1990) Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 47:533–543
Hogg RJ, Furth S, Lemley KV, Portman R, Schwartz GJ, Coresh J, Balk E, Lau J, Levin A, Kausz AT, Eknoyan G, Levey AS (2003) National Kidney Foundation's Kidney Disease Outcomes Quality Initiative clinical practice guidelines for chronic kidney disease in children and adolescents: evaluation, classification, and stratification. Pediatrics 111:1416–1421
Rashed AN, Neubert A, Tomlin S, Jackman J, Alhamdan H, AlShaikh A, Attar A, Aseeri M, Wilton L, Wong I (2012) Epidemiology and potential associated risk factors of drug-related problems in hospitalised children in the United Kingdom and Saudi Arabia. Eur J Clin Pharmacol 68(12):1657–1666
Rashed AN, Neubert A, Tomlin S, Jackman J, Alhamdan H, AlShaikh A, Attar A, Aseeri M, Wilton L, Wong I (2013) Drug-related problems found in children attending an emergency department in Saudi Arabia and in the United Kingdom. Int J Clin Pharm 35(3):327–331
Ibrahim N, Wong IC, Patey S, Tomlin S, Sinha MD, Jani Y (2013) Drug-related problem in children with chronic kidney disease. Pediatr Nephrol 28:25–31
Pruthi R, O'Brien C, Braddon F, Lewis M, Maxwell H, Stojanovic J, Tse Y, Inward C (2012) Chapter 7: demography of the UK paediatric renal replacement therapy population in 2012. UK Renal Registry 16th Annual Report 2012. Available at: http://www.renalreg.com/Report-Area/Report%202013/07-Chap-07.pdf. Accessed 28 January 2014
Jani YH, Barber N, Wong IC (2010) Paediatric dosing errors before and after electronic prescribing. Qual Saf Health Care 19(4):337–340
Ghaleb MA, Barber N, Franklin BD, Wong IC (2010) The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Child 95(2):113–118
Rashed AN, Wilton L, Lo CCH, Kwong BYS, Leung S, Wong ICK (2014) Epidemiology and potential risk factors of drug-related problems in Hong Kong Paediatric wards. Br J Clin Pharmacol 77(5):873–879
Dean BS, Barber ND (1999) A validated, reliable method of scoring the severity of medication errors. Am J Health Syst Pharm 56(1):57–62
Pharmaceutical Care Network Europe Foundation (PCNE) DRP Classification Scheme version 6.2. Available at: http://www.pcne.org/sig/drp/documents/PCNE%20classification%20V6–2.pdf. Accessed 1 March 2011
Kaplan B, Mason NA, Shimp LA, Ascione FJ (1994) Chronic hemodialysis patients. I. Characterization and drug-related problems. Ann Pharmacother 28(3):316–319
Grabe DW, Low CL, Bailie GR, Eisele G (1997) Evaluation of drug-related problems in an outpatient hemodialysis unit and the impact of a clinical pharmacist. Clin Nephrol 47(2):117–121
Manley HJ, Drayer DK, Muther RS (2003) Medication-related problem type and appearance rate in ambulatory hemodialysis patients. BMC Nephrol 4:1–7
Cardone KE, Bacchus S, Assinom MM, Pai AB, Manley HJ (2010) Medication-related problems in CKD. Adv Chronic Kidney Dis 17(5):404–412
Salgado TM, Moles R, Benrimoj SI, Fernandez-Llimos F (2012) Pharmacists' interventions in the management of patients with chronic kidney disease: a systematic review. Nephrol Dial Transplant 27(1):276–292
Brown C, Hofer T, Johal A, Thomson R, Nicholl R, Franklin BD, Lilford RL (2008) An epistemology of patient safety research: a framework for study design and interpretation. III. End points and measurement. Qual Saf Health Care 7(3):170–177
Wong IC, Ghaleb MA, Franklin BD, Barber N (2004) Incidence and nature of dosing errors in paediatric medications: a systematic review. Drug Saf 27(9):661–670
Ghaleb MA, Barber N, Frankin BD, Yeung VW, Khaki ZF, Wong IC (2006) Systematic review of medication errors in pediatric patients. Ann Pharmacother 40(10):1766–1776
Wong IC, Basra N, Yeung VW, Cope J (2006) Supply problems of unlicensed and off-label medicines after discharge. Arch Dis Child 91(8):686–688
Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Fedrico F, Goldmann DA (2001) Medication errors and adverse drug events in pediatric inpatients. JAMA 285(16):2114–2120
Kunac DL, Reith DM (2008) Preventable medication-related events in hospitalised children in New Zealand. N Z Med J 121(1272):17–32
Belaiche S, Romanet T, Allenet B, Calop J, Zaoul P (2012) Identification of drug-related problems in ambulatory chronic kidney disease patients: a 6-month prospective study. J Nephrol 25(5):782–788
Castelino RL, Sathvik BS, Parthasarathi G, Gurudev KC, Shetty MS, Narahari MG (2011) Prevalence of medication-related problems among patients with renal compromise in an Indian hospital. J Clin Pharm Ther 36(4):481–487
Impicciatore P, Choonara I, Clarkson A, Provasi D, Pandolfini C, Bonati M (2001) Incidence of adverse drug reactions in paediatric in/out-patients: a systematic review and meta-analysis of prospective studies. Br J Clin Pharmacol 52(1):77–83
Brandt JR, Wong CS, Hanrahan JD, Qualls C, McAfee N, Watkins SL (2006) Estimating absolute glomerular filtration rate in children. Pediatr Nephrol 21(12):1865–1872
Pai AB, Cardone KE, Manley HJ, St Peter WL, Shaffer R, Somers M, Mehrotra R (2013) Medication reconciliation and therapy management in dialysis-dependent patients: need for a systematic approach. Clin J Am Soc Nephrol 18(11):1988–1999
St Peter WL, Wazny LD, Patel UD (2013) New models of chronic kidney disease care including pharmacists: improving medication reconciliation and medication management. Curr Opin Nephrol Hypertens 22(6):656–662
Huynh C, Jani Y, Wong IC, Dewchand B, Tomlin S (2013) What is the current practice of medicines reconciliation in children nationally in the UK? Int J Pharm Pract 21(1):62–65
Conroy S, Carroll WD (2009) Prescribing in paediatrics. Arch Dis Child Educ Pract Ed 94(2):55–59
Dean AJ, Walters J, Hall A (2010) A systematic review of interventions to enhance medication adherence in children and adolescents with chronic illness. Arch Dis Child 95(5):717–723
Wong IC, Wong LY, Cranswick NE (2009) Minimising medication errors in children. Arch Dis Child 94(2):161–164
So TY, Layton JB, Bozik K, Farrington E, Gipson PE, Gibson K, Primack W, Conley W, Gipson DS, Ferris M (2011) Cognitive pharmacy services at a pediatric nephrology and hypertension clinic. Ren Fail 33(1):19–25
Stemer G, Lemmens-Gruber R (2011) Clinical pharmacy activities in chronic kidney disease and end-stage renal disease patients: a systematic literature review. BMC Nephrol 12:35. doi:10.1186/1471-2369-12-35
Acknowledgement
The authors wish to thank the Ministry of Health Malaysia for funding Norkasihan Ibrahim in this PhD research, Deborah Riddout and Monalis Bagkeris of UCL Institute of Child Health for their statistical advice, the Renal and Pharmacy team of ELCH and GOSH, especially William Thornhill, Susan Patey, Christine Booth, Nikesh Gudka and Iek Leng Cheng for their professional cooperation.
Ethics approval
This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki; approved by the National Research Ethics Committee, London, UK (11/LO/0879; 12/LO/0709) and informed consent was given to all subjects before inclusion.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1
Appendix 2
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Ibrahim, N., Wong, I.C.K., Tomlin, S. et al. Epidemiology of medication-related problems in children with kidney disease. Pediatr Nephrol 30, 623–633 (2015). https://doi.org/10.1007/s00467-014-2982-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-014-2982-5