Abstract
Clear recommendations for the management of acute varicella-zoster virus (VZV) infections for cases of significant exposure and the use of prophylactic drugs after solid-organ transplantation are missing due to the lack of evidence by prospective studies. Heterogeneity in patient groups, patient numbers, age groups, immunosuppressive regimens, timing, and dosage of aciclovir and/or varicella-zoster immunoglobulin (VZIG), pre-transplant vaccination or VZV wild-type infection and inconsistency of data make comparability of different studies impossible. Although the benefit of aciclovir and/or VZIG is uncertain in immunosuppressed children, prospective controlled double-blind studies are not feasible for ethical considerations as fatal cases with disseminating varicella disease are well known in these patient groups despite the use of aciclovir and/or VZIG, whereas severe side-effects of these drugs are rare. However, a reporting bias is likely as mainly severe or fatal cases might have been predominantly published or cases of successfully used aciclovir and/or VZIG in mild cases or in cases of breakthrough infections after vaccination. As neither VZIG prophylaxis nor treatment with intravenous aciclovir offers complete protection against severe VZV infection to immunosuppressed pediatric solid-organ transplant recipients, high priority should be given to vaccination against VZV prior to transplantation, and, most importantly, in their close contact persons. Clinical observations suggest that only assessment of humoral immunity together with cellular immunity may allow predication about protection in exposed patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although acute varicella or chickenpox caused by varicella-zoster virus (VZV) is usually a mild disease in immunocompetent hosts, it may cause disseminating infection with severe illness in immunocompromised patients [1]. Fatal cases result from pneumonitis, hepatitis, central nerval system involvement, and disseminated intravascular coagulation [2]. Acute varicella infection is still an important cause of death in pediatric solid-organ transplant recipients, despite the use of varicella-zoster-specific immunoglobulin (VZIG) and aciclovir therapy [3]. The rising number of pediatric solid-organ transplant recipients has constituted a new challenge for physicians and pediatricians to manage acute VZV infection in patients under immunosuppressive therapy. As VZV induces not only humoral immunity but also cellular immunity by specific effector T cells, it is still a matter of debate whether serological proof of VZV-specific IgG in exposed patients alone is able to give information about protection, particularly as protective levels of VZV-specific IgG are not known. Thus, no standardized recommendations exist for the use of VZIG and aciclovir administration in exposed patients who have a positive serology for VZV-specific IgG.
So far, few studies have investigated the safety and efficacy of aciclovir and/or VZIG treatment for prophylaxis of serious VZV infection in immunocompromised pediatric patients. Most reports about cases of successful use of aciclovir and VZIG provide a low evidence level. Clear recommendations for the management of acute VZV infections for cases of significant exposure and the use of prophylactic drugs after solid-organ transplantation are missing due to the lack of evidence in prospective studies. Thus, the following review is aimed to provide an educational review of published data on the safety and efficacy of aciclovir and VZIG in the case of varicella infection or exposure in immunocompromised pediatric solid-organ transplant recipients.
Methods
For data collection on aciclovir and VZIG use in immunosuppressed patients, a systematic search using MEDLINE was performed. For a comprehensive search, the following search strategy with the combination of a text-string search in titles and a Medical Subject Headings (MeSH) term search was used: “varicella”, “chickenpox”, “herpes zoster”, “aciclovir”, “varicella-zoster-immunoglobulin”, “VZIG” “immunoglobulin”, “prophylaxis” and “immunosuppression”, “immunocompromised”, and “transplantation”.
The search was restricted to English-language and German articles published between 1975 and April 2010. To specify the publication type and contents of papers, “limits” for search were applied: “review”, “human subjects”, and “children”. In MEDLINE, initial searches retrieved about 2,300 articles. The abstracts of all articles were screened for relevant information by using the following inclusion criteria: (1) original articles, reviews, case reports, tutorials, letters, editorials, and commentaries; (2) articles describing aspects of aciclovir and/or VZIG administration; (3) articles giving the age of individuals studied; (4) articles stating the type of organ transplanted. Unfortunately, not all articles give the VZV-specific immune status (VZV naive, wild-type VZV infected, vaccinated and/or breakthrough infections) of the patients, the dosage and/or application pathways of aciclovir and/or VZIG, the time point of administration and whether the patients were vaccinated or not. The following articles were excluded: (1) only epidemiological papers; (2) articles which do not give the age of individuals; (3) hypothetical content without primary data; (4) exclusively cost-effectiveness-studies.
Measurement of VZV-specific immunity
Besides the anamnestic knowledge of the varicella-typical rash and symptoms, serological tests are able to confirm former contact with VZV or successful vaccination. However, evaluation and interpretation of immunity against VZV is difficult, particularly in transplant recipients, as both VZV-specific antibodies and VZV-specific effector T cells have been shown to protect from VZV infection. These two aspects of VZV-specific immunity have demonstrated that it is impossible to define a protective antibody concentration against VZV.
Generally, VZV-specific antibodies are detected by complement fixation, latex agglutination, indirect immunofluorescence assays, neutralization tests, enzyme-linked immunosorbent assays (ELISA), and by fluorescent antibody-to-membrane antigen test [4]. A correlation between early elevated antibody titers and protection was only described for assays using gpELISA with titers equal to or greater than 5 gpELISA [5, 6]. As suggested by some studies with renal transplant recipients [7–9], early detected elevated antibody titers may not be useful as a marker of long-term protection because they reflect only the immediate response either to the vaccine or to the infection. However, the absence of VZV-specific IgG antibodies does not imply a loss of protection as cell-mediated immunity against VZV may still be intact in healthy, not otherwise immunocompromised children. Unfortunately, some serological tests also show limitations when evaluating cases of breakthrough varicella disease [10].
The knowledge about the importance of cell-mediated immunity for clearance of primary VZV infection, of the prevention of recurrent infections, or reactivation is based on data from patients with congenital or acquired immunodeficiencies involving the cellular immune system [11] who showed an increased severity of the disease. It has been demonstrated that reactivation of VZV is associated with a decline in VZV-specific T cells [12]. In transplant recipients, a marked dysfunction of the T cell system is induced by immunosuppressive therapy. VZV-specific effector T cells can be detected by their interferon-γ production after stimulation with VZV-specific antigens in vitro [13, 14]. Unfortunately, experience with assessment of cellular immunity against VZV in solid-organ transplant recipients is poor [15].
Thus, so far, no recommendations exist of when to start anti-VZV therapy despite having VZV-specific antibody titers in immunocompromised patients as no protective IgG levels are described. However, the previously shown data suggest to measure both anti-VZV IgG and VZV-specific T cells before making any therapeutic decisions.
Treatment of acute varicella infection
In immunocompetent hosts, varicella is a self-limited disease and symptomatic treatment with antipyretics to control fever, lotions for pruritus, and fluid substitution to maintain hydration is sufficient. Because of the putative associations with Reye’s syndrome, treatment with acetyl salicylic acid is strongly discouraged in children with varicella disease [16]. Non-steroidal anti-inflammatory drugs in children with varicella might increase the risk of necrotizing soft-tissue infections and invasive infections with group A beta-hemolytic Streptococcus, although these associations are discussed controversially [17, 18]. Bacterial superinfections have to be treated with antimicrobial therapy.
The use of aciclovir is not recommended for otherwise healthy children with uncomplicated varicella [19]. However, aciclovir has been proven to be useful and well tolerated in the treatment of varicella in otherwise healthy children [20]. A randomized, placebo-controlled, double-blind trial was performed in 105 otherwise healthy children between 5 and 16 years of age with laboratory-confirmed varicella. Of the 102 children finally included into the analysis, 50 received aciclovir and 52 received placebo [20]. Aciclovir-treated patients recovered earlier and had fewer skin lesions. However, untreated patients did not show significantly higher complication rates compared to aciclovir treated patients (10% vs. 13.5% in the placebo group). Patients who were treated with aciclovir had lower geometric mean serum antibody titers to VZV than patients of the placebo group 4 weeks after disease onset, but similar antibody titers 1 year later.
Resistance to aciclovir is not common, and has so far been reported mainly in patients with underlying HIV infection. For these cases, intravenous foscarnet is recommended [21]. However, antiviral treatment is strongly recommended for immunocompromised hosts, newborns whose mothers acquired infection around the time of delivery, and for any patients with VZV-mediated complications such as ocular involvement, pneumonia, or encephalitis. In immunocompromised hosts or patients with severe disease presentation or complications, aciclovir is the therapy of choice, with best effects if given intravenously within 72 h of disease onset [22, 23]. A daily dosage of 1,500 mg/m2 per day (corresponds to 30 mg/kg) in three doses for children until 12 years of age was recommended; for adolescents and adults 15 mg/kg per day (corresponds to 750 mg/m2) in three divided doses [1]; for immunocompromised adults, as far as renal function is not impaired, 30 mg/kg in three divided doses. In patients with renal impairment, the daily dosage has to be reduced by extension of administration intervals, due to the risk of kidney damage. For a creatinine clearance of 25 to 50 ml/min, a dosage of 5 to 10 mg/kg (depending on indication) every 12 h and for a creatinine clearance of 10 to 25 ml/min every 24 h is recommended. For patients with a creatinine clearance of 0 to 10 ml/min, administration of aciclovir is dependent on the dialysis method: on peritoneal dialysis, halving of the recommended dosage (5 to 10 mg/kg) and administration every 24 h; on hemodialysis, halving of the recommended dosage (5 to 10 mg/kg) and administration every 24 h and after hemodialysis [24, 25].
Immunocompetent children
Only a few studies deal with the safety and efficacy of aciclovir and VZIG in immunocompetent children and the use and benefit from these drugs in healthy children is highly controversial.
In a multicenter, double-blind, placebo-controlled study involving 815 immunocompetent children 2 to 12 years old, treatment with oral aciclovir within 24 h of disease onset resulted in a 1-day reduction of fever and a 15–30% reduction in the severity of cutaneous and systemic signs [26]. In that study, aciclovir did not reduce the rate of complications. However, the study authors counted only 11 complications, of them, ten cases could be attributed to bacterial infections. The recommended dosage for aciclovir was 80 mg/kg per day divided into four doses for children and 4 g per day divided into five doses for adults for 5 days.
Studies revealed that the use of aciclovir prophylaxis in immunocompetent children exposed to a household contact with active varicella significantly decreased the transmission rate of VZV [27–29]. Most important for cases of re-exposure, these children developed subclinical infection with a prolonged humoral immunity against VZV [29].
Valaciclovir and ganciclovir can be used as alternatives to aciclovir. In immunocompetent individuals, valaciclovir 1 g three times per day has been shown to be superior to an oral dosage of 800 mg aciclovir five times per day, with both medications given for 7 days [30]. Regarding ganciclovir, VZV is ten times more sensitive to aciclovir than to ganciclovir, which favors the use of aciclovir [31].
Immunocompromised children
Immunosuppression and VZIG
VZIG at a dosage of 5–25 International Units per kilogram has been considered effective in susceptible immunocompromised children when used within 72 h, maximum 96 h, of significant exposure to VZV [19, 32]. VZIG should be given as early as possible, as losing time reduces protective function. Although there exists no proof for the right time frame of VZIG administration in immunocompromised patients, most of the evidence for the appropriate time window to allow a successful use of VZIG comes from experience with VZV infections in obstetrics demonstrating a reduction of severe illness for VZIG administration within 96 h [33]. However, in 18 susceptible pediatric liver transplant recipients, who were exposed, eight patients developed mild varicella disease although VZIG was given within 96 h [32].
VZIG has been shown to be safe and efficient in immunocompromised hosts after significant household exposure to varicella [34]. Despite the administration of VZIG, symptoms of acute varicella infection occurred in 60% of 81 recipients of VZIG. Doubling of the dose of VZIG administered reduced the rate of subclinical infection in immunosuppressed children, but could compromise the development of humoral immunity against VZV.
Immunosuppression and aciclovir treatment
Some experience with antiviral drugs in immunosuppressed patients comes from studies including patients with oncological or hematological disorders. As shown in studies of children having leukemia [35, 36] or HIV infection [37], the need for aciclovir is uncertain in children with leukemia.
In a Canadian experience with aciclovir therapy from 11 pediatric hospitals in the province Quebec, 706 children under age of 18 years and 179 adults needed 909 hospitalizations [38]. Of them, 583 were hospitalized to receive therapy for one or several complications of varicella disease, 127 had to be treated with intravenous aciclovir, and 199 received supportive care. Among 644 hospitalizations in healthy people, treatment of complications counted for 473 (73.4%) hospitalizations, administration of intravenous aciclovir for 30 (4.7%), and supportive care for 141 (21.9%) compared to 46 (33.8%), 85 (62.5%) and five (3.7%), respectively, among 136 hospitalizations in immunocompromised patients. Five deaths, one child (not immunosuppressed) and four adults (three immunosuppressed), were reported due to varicella-associated complications despite aciclovir therapy.
Regarding the preference of oral or intravenous aciclovir therapy, again, some experience comes from oncology, with a favorable outcome in 14 bone marrow transplant recipients receiving oral and 13 bone marrow transplant recipients receiving intravenous aciclovir treatment to treat localized herpes zoster [39]. In this study, oral and intravenous aciclovir were equally effective.
Interruption or reduction of immunosuppressive therapy such as azathioprine was suggested as supportive treatment to aciclovir administration and/or VZIG in the case of acute varicella infection [40, 41]. Although mycophenolate mofetil has been associated with an increased susceptibility to VZV infection [8, 42], some groups support its maintenance because it may enhance the antiviral activity of aciclovir at least in vitro [43]. The use of aciclovir was also safe in cases of renal transplant patients on cyclosporine A therapy [44]. According to other authors, no immunosuppressive drug is significantly associated with a higher risk of disseminated VZV infection [45]. Early therapy with high-dose aciclovir has a key role in decreasing the mortality due to VZV infection [45]. Treatment with aciclovir can be either started immediately after exposure to varicella and continued for 5–7 days or can be continued to day 14 after exposure [28, 29].
Immunosuppression and aciclovir prophylaxis
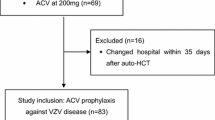
Some experience for aciclovir treatment as low-dose long-term prophylaxis for prevention of VZV disease exists from studies with hematological patients [46–48]. In 77 hematopoietic cell transplant recipients at risk for VZV reactivation, long-term aciclovir therapy effectively and safely prevented VZV disease during the first year after transplantation, but was not significant anymore in the second year after transplantation [46]. In a study with 242 Japanese adult patients who underwent allogeneic hematopoietic stem cell transplantation, aciclovir prophylaxis was continued until the end of immunosuppressive therapy and at least 1 year after transplantation. The cumulative incidence of VZV reactivation was 34.7%. The use of long-term aciclovir was the only independent determinant that significantly decreased the overall incidence of VZV reactivation (20% vs. 50%) [47]. Long-term aciclovir was also proven to be an independent protective factor for VZV infection in a study with 99 adult patients who had allogeneic peripheral blood stem cell transplantation and received aciclovir in comparison with 173 patients who were not on prophylaxis [48]. Unfortunately, so far, no experience exists with low-dose prophylaxis in the first months after solid-organ transplantation.
Immunosuppression and ganciclovir or valaciclovir treatment
Ganciclovir and valaciclovir are also discussed as alternatives to treat VZV disease in immunocompromised patients. A reduction of the viral load of VZV was investigated in a renal transplant recipient with disseminating zoster and simultaneously occurring cytomegalovirus (CMV) disease under the use of ganciclovir [49]. In a trial with 151 patients undergoing allogeneic bone marrow transplantation, no patient who was treated either with aciclovir or ganciclovir developed VZV disease, but there was a rapid onset of VZV disease following cessation of antiviral treatment [50].
Valaciclovir was used in a survey of 28 VZV seronegative children who were younger than 10 years of age at heart transplantation. Of them, 14 patients developed acute varicella. Seven patients out of the 14 VZV-afflicted patients were admitted for intravenous aciclovir for 3 days followed by oral aciclovir for 7 days. Six patients were treated with valaciclovir for 7 days and one patient with oral aciclovir for 10 days. All patients recovered and 12 of the 14 VZV-afflicted patients maintained detectable antibody titers in long-term follow-up [51].
In a double-blind study, comparing two dosages of valaciclovir hydrochloride for therapy of uncomplicated herpes zoster in immunocompromised adults was shown to be a safe and efficient therapy at a dosage of 1 g three times per day [30].
Renal transplant recipients
Aciclovir was suggested as an adjunctive preventive therapy to VZIG administration in patients with nephrotic syndrome or renal transplantation [52]. Some studies have demonstrated that VZV infection in patients with renal transplantation can be treated effectively with aciclovir [40, 53]. However, a subset of these children has a serious sequelae from VZV infection, especially under treatment with corticosteroids [3, 7, 54–56]. Thus, a more aggressive treatment with prophylactic VZIG and high-dose intravenous aciclovir was discussed for primary VZV infection in immunosuppressed renal transplant recipients, as protection against VZV is a function of both humoral immunity consisting of VZV-specific IgG concentrations and antibody avidity, as well as cellular immunity accomplished by VZV-specific cytotoxic T cells (Table 1). Particularly the latter may be compromised by immunosuppressive therapy in transplant recipients, which was confirmed by a case of chronic varicella in a liver-transplanted child who successfully received specific autologous cytotoxic T cells when antiviral therapy with aciclovir and VZIG failed [56].
In an important observational study including 704 children and adolescents who received renal transplantation, patients were divided into three groups: 49 VZV naive patients (of which 22 developed varicella and three died) (group A); 415 patients with a history of varicella (of which four developed another episode of VZV disease after transplantation) (group B); 212 vaccinated patients (of which 75 demonstrated persisting humoral immunity) (group C1); and 103 patients showed no humoral immunity at transplantation plus 19 patients who lost VZV-specific antibodies after transplantation (group C2) [41]. In group C2, 26 patients developed varicella and 21 had asymptomatic seroconversion. Fortunately, no deaths were reported. Regarding treatment, on first symptoms of varicella, azathioprine was stopped in all patients for a mean duration of 10 days in group A and for 6 days in group C2. Hyperimmune gamma globulins were administered in ten patients (one of whom died), and intravenous aciclovir in 22 other patients (half of them received also hyperimmune globulins, with one patient who died in this group). Two patients of group C2 were treated with oral aciclovir only. One patient of group A who did not receive any specific therapy died. In three patients (all of group C), a rejection episode was reported after varicella disease and stopping azathioprine. Fortunately, all three patients completely recovered. The reported data confirm the vital risk of varicella after renal transplantation in children who had no history of the disease or VZV vaccination or even a poor antibody response after vaccination. Overall, the study teaches us that VZV vaccination is useful in prevention of severe sequelae and deaths, even though not all patients developed VZV-specific antibodies in the vaccinated group. Also, the appropriateness of administration of another dose of the vaccine to patients who did not develop detectable antibodies was discussed in that study.
In a study from Zurich, Switzerland, four cases of disseminating VZV infection in a population of around 1,000 adult renal transplant recipients were reported [45]. In 38 published cases of disseminated VZV infection in adult renal allograft recipients from 1981 to 2000, the main complications of acute varicella infection were pneumonitis, hepatitis, and disseminated intravascular coagulation with an overall mortality of 34% [45]. Among these patients, 82% suffered from primary varicella infection and 18% had a VZV reactivation. High-dose aciclovir and reduction of immunosuppression led to a fall in mortality from 53% before 1990 to 22% after 1990. However, studies in children with chronic kidney disease showed that the risk of symptomatic varicella (and in particular fulminating varicella) is not always prevented by VZIG prophylaxis or treatment with intravenous aciclovir, but it can be reduced substantially by vaccination [57, 58].
Investigating 69 cases of VZV infection in pediatric renal transplant recipients between 1984 and 1996 showed that VZV in children with renal transplantation can be successfully treated with intravenous aciclovir and temporary withdrawal of azathioprine [40]. Allograft rejection was uncommon with this approach and appeared only in three patients who responded successfully to prednisone treatment. Intravenous aciclovir was administered in 62 of 69 cases, and one patient died from complications.
In a study with 83 pediatric renal transplant recipients, eight children had a cutaneous manifestation of the disease. Of them, four had evidence of visceral disease [3]. Three of these eight children received VZIG after exposure, and all eight children were treated with high-dose intravenous aciclovir. Two children died of complications of VZV infection, including one child who received VZIG on the day of exposure to varicella.
A single-center experience with 812 adult renal transplant recipients revealed eight patients with VZV infection (four cases primary infection, four cases disseminated VZV reactivations) [59]. Treatment consisted of reduced immunosuppression and aciclovir, and in six patients, a VZIG dose. There was no statistically significant difference of recipient demographic characteristics, immunosuppressive treatment or the use of VZIG on the clinical spectrum of the disease. One initially negative patient for VZV who had delayed diagnosis and chronic infection with hepatitis B virus died despite high-dose aciclovir treatment and VZIG. The authors suggested that VZIG is useless once the disease is established, a finding that agrees with others [3, 45, 60].
In a multicenter study, 16 VZV exposures in 12 pediatric patients (seven nephrotic syndrome, five renal allograft transplantation) had been registered [52]. Ten patients received aciclovir prophylaxis, and six patients served as controls. None of the eight patients (ten exposures) who received aciclovir prophylaxis developed clinical varicella. One patient who received aciclovir therapy developed humoral immunity. No adverse effects such as renal dysfunction under aciclovir therapy were detected. One of the four controls (six exposures) developed clinical VZV infection and was treated with aciclovir. He was the only patient in the control group developing humoral immunity to VZV. There was no difference between treated and untreated group concerning the rate of clinical varicella.
In 19 children with renal transplantation, in three children with serologically documented immunity to VZV acute VZV infection occurred. All cases were managed with oral aciclovir, and had an uncomplicated recovery without neuralgia [8]. In contrast, of 74 patients transplanted before the use of mycophenolate mofetil, only one patient had varicella, which led the authors to conclude that mycophenolate mofetil may be associated with higher risk of VZV infection or reinfection [8].
Between 1969 and 1998, in 476 renal transplant patients, four patients developed varicella, all patients received aciclovir therapy, but unfortunately two of them died [60].
Most of the other published reports document cases of successful or unsuccessful use of aciclovir and/or VZIG prophylaxis. An outbreak of acute VZV infection was reported in three adult renal transplant recipients [61]. All patients were treated with intravenous aciclovir under reduction of immunosuppressive therapy (cyclosporine was discontinued, prednisolone continued at its prior dosage, prescribed mycophenolate mofetil at half of its prior dosage) and survived without complications. A fulminating VZV infection despite prophylactic VZIG and intravenous aciclovir was described in a 30-year-old renal transplant recipient, who died from complications [62]. In another case report, two adult patients with renal transplantation presented with disseminated VZV infection, but were successfully treated with aciclovir alone in one case, and with both aciclovir and VZIG in the second case [63].
Liver transplantation
Some cases support the use of aciclovir in liver transplant recipients (Table 2). A case of a varicella infection following VZV vaccination in a liver transplant recipient was mild under aciclovir therapy [64].
In a retrospective chart review based on the discharge diagnoses of orthotopic liver transplantation and varicella among pediatric patients in California between 1985 and 2001, 22 patients of 556 liver transplant recipients were admitted to the hospital because of varicella infection [65]. None of the patients were vaccinated, and five patients received VZIG. All patients were treated with intravenous aciclovir and discharged with oral aciclovir to complete a 10-day course (including the intravenous treatment). No patient had VZV-associated complications. One patient had elevated serum creatinine levels under intravenous aciclovir treatment, which resolved to normal within 2 weeks. Another report analyzed 20 pediatric liver transplant recipients with acute VZV infection, and nine of them received intravenous aciclovir. None of the children had complications [66]. In a study with 67 children with liver transplantation, 32 patients were exposed, 14 cases of varicella were reported, again despite prophylaxis with VZIG and intravenous aciclovir, and two of them died because of varicella-related complications [32].
In a post-liver transplantation vaccination study with VZV vaccine (Varivax) of 16 children, five children were exposed to varicella, one received aciclovir, one VZIG, both stayed asymptomatic as well as the other three untreated subjects [15].
In another study with 11 children vaccinated with a single dose of Varilrix before liver transplantation, four children with low antibody titers who were exposed to VZV required VZIG prophylaxis, of whom two children developed mild varicella whereas the other two stayed asymptomatic. In that study, it was unclear whether the mild nature of the varicella infection resulted from protecting T cell function by the VZV vaccine, or from an effect by VZIG prophylaxis or therapy with aciclovir. Protection against severe varicella may be maintained after the loss of vaccine-induced antibodies, as cell-mediated immunity stimulated by VZV infection or immunization is believed to be the more important part of protection against and for the recovery from the disease. However, it is thought that assessment of immunity and targeted prophylaxis is the safest option in immunocompromised patients regardless of immunization history [67].
Heart and lung transplantation
In a report including 28 pediatric heart transplant recipients on nonsteroid maintenance immunosuppression, 14 developed acute varicella infection at a median time of 3.3 years post-transplantation [51]. Seven patients were admitted for intravenous aciclovir for 3 days, followed by oral aciclovir for 7 days. Six patients were treated as outpatients with oral valaciclcovir for 7 days, one with oral aciclovir for 10 days. Both regimens, intravenous and/or oral, were well tolerated and without complications or episodes of rejections. All patients seroconverted despite aciclovir treatment. However, two patients under enhanced immunosuppression lost detectable VZV-specific antibodies.
A 10-year single-center experience was reported for 13 cases of VZV disease in heart and lung transplantation. Four patients showed a resolution of VZV infection with combination of intravenous aciclovir and polyspecific intravenous immunoglobulin [68].
Eleven patients among 175 adult cardiac transplant patients developed clinical zoster and recovered under intravenous aciclovir (five patients) or oral therapy (six patients) [69].
Discussion
Generally, several uncertainties exist when evaluating the proposed benefit of aciclovir and/or VZIG in pediatric solid-organ transplant recipients: First, most of the published literature consists of case reports and retrospective chart reviews; second, heterogeneity in patient groups, patient numbers, age groups, immunosuppressive regimens, timing and dosage of aciclovir and/or VZIG, pre-transplant vaccination or VZV wild-type infection and inconsistency of data make comparability of different studies impossible. Although the benefit of aciclovir and/or VZIG is uncertain in immunosuppressed children, prospective controlled double-blind studies are not feasible for ethical considerations as fatal cases with disseminating varicella disease are well known in these patient groups despite the use of aciclovir and/or VZIG, whereas severe side-effects of these drugs are rare. However, a reporting bias in case reports and retrospective studies cannot be neglected as mainly severe or fatal cases might have been predominantly published or cases of successfully used aciclovir and/or VZIG in mild cases or in cases of breakthrough infection after vaccination. However, despite these concerns, it appears from most reviewed studies that early intravenous aciclovir administration may prevent severe courses of varicella infection in immunosuppressed children.
One of the major questions for clinicians taking care of immunocompromised pediatric transplant recipients is how to approach the therapeutic management of these patients after significant exposure to VZV. No doubt, to prevent a serious sequelae, seronegative patients have to be treated with aciclovir and VZIG immediately. For prophylactic use, the orally administered aciclovir seems appropriate. In cases of moderate to severe presentation of manifest VZV disease in immunocompromised patients, intravenous aciclovir should be preferred. Seropositive patients who show positive cellular responses to VZV-antigen stimulation by interferon-γ production in vitro may usually expect a mild course of varicella, thus prophylactic aciclovir or VZIG treatment may be deferred to await the clinical presentation. In seropositive cases in which laboratory investigation of cellular immunity is not available, aciclovir alone may be sufficient to prevent serious complications. However, so far, the role of cellular immunity against VZV is not clearly understood, as most data are based on small patient numbers and heterogeneous groups. VZV-specific memory CD4+ T cell response has been shown to largely resemble the primary immune response to VZV with VZV-specific memory CD4+ T cells producing interferon-γ [70]. In individuals with VZV vaccination following a two-dose regimen, a significant in vitro proliferative response of VZV-specific lymphocytes was reported [71, 72] with maintenance of the cellular immune response in 90% of 29 children after 1 year and in 87% of 60 children 5 years after vaccination [72, 73], although detailed data about clinical correlates of protection are missing in these studies. Overall, in the future, measurement of VZV-specific cellular immunity may provide an additional tool to assess immunity against VZV disease [74].
Despite uncertainties in assessment of immunity against VZV, clinical observations teach us that primary prevention of serious varicella disease by vaccination against VZV is effective in most cases. Thus, most importantly, vaccination is strongly recommended in candidates listed for solid-organ transplantation and their close contact persons. Breakthrough varicella and herpes zoster by the vaccine virus are rare and have a usually mild presentation.
Generally, VZV vaccination in patients with chronic kidney or liver impairment listed for transplantation appears to be safe and in most cases efficient [75]. Experience with VZV vaccination after renal [76] or liver transplantation [77, 78] is poor. In the described cases, VZV vaccination was immunogenic and safe. Thus, it appears reasonable to think about post-transplant VZV vaccination in cases of waning immunity after pre-transplant VZV vaccination or wild-type VZV infection as suggested by some authors [78].
Beside the individual tragedy of fulminant varicella infection in each patient who is not vaccinated or does not have sufficient humoral and cellular protection from acute VZV infection or reactivation, a two-dose vaccination program has also demonstrated that vaccination against VZV proved to be a cost-effective strategy in immunosuppressed patients [79, 80]. An economic evaluation of varicella vaccine for pediatric liver and kidney transplant recipients revealed that varicella vaccination should be recommended also to save costs from aciclovir and VZIG treatment [81]. A decision-analysis model was calculated to evaluate the cost-effectiveness of vaccinating patients with chronic renal failure against VZV prior to transplantation [81]. Under baseline assumptions, compared to aciclovir treatment, VZIG or hospital admission due to complications or for the purpose of parenteral therapy, VZV vaccination pre-transplant was a cost-effective strategy, with a cost of $211 per patient vaccinated compared with $1,828 per patient not vaccinated.
Neither VZIG prophylaxis nor treatment with intravenous aciclovir offers complete protection against severe VZV infection to immunosuppressed pediatric solid-organ transplant recipients, although this age group has the highest risk of exposure to VZV. Thus, in conclusion, high priority should be given to vaccination against VZV, which should be administered in susceptible transplant candidates, preferably prior to transplantation and, most important, in their close contact persons. Although data on the development and maintenance of the immune response against VZV after wild-type infection or vaccination are limited, clinical observations suggest that only assessment of humoral immunity together with cellular immunity may allow predication about protection in exposed patients.
References
Slifkin M, Doron S, Snydham DR (2004) Viral prophylaxis in organ transplant patients. Drugs 64:2763–2792
Heininger U, Seward JF (2006) Varicella. Lancet 368:1365–1376
Lynfield R, Herrin JT, Rubin RH (1992) Varicella in pediatric renal-transplant recipients. Pediatrics 90:216–220
Sauerbrei A, Farber I, Brandstadt A, Schake M, Wutzler P (2004) Immunofluorescence test for sensitive detection of varicella-zoster virus-specific IgG: an alternative to fluorescent antibody to membrane antigen test. J Virol Methods 119:25–30
White CJ, Kuter BJ, Ngai A, Hildebrand CS, Isganitis KL, Patterson CM, Capra A, Miller WJ, Krah DL, Provost PJ (1992) Modified cases of chickenpox after varicella vaccination: correlation of protection with antibody disease. Pediatr Infect Dis J 11:19–23
Li S, Chan IS, Matthews H, Heyse JF, Chan CY, Kuter BJ, Kaplan KM, Vessey SJ, Sadoff JC (2002) Inverse relationship between six-week postvaccination varicella antibody response to vaccine and likelihood of long-term breakthrough infection. Pediatr Infect Dis J 21:338–342
Feldhoff CM, Balfour HH, Simmons RL, Najarian JS, Maurer SM (1981) Varicella in children with renal transplants. J Pediatr 98:25–31
Rothwell WS, Gloor JM, Morgenstern BZ, Milliner DS (1999) Disseminated varicella infection in pediatric renal transplant recipients treated with mycophenolate mofetil. Transplantation 68:158–161
Laube GF, Berger C, Goetschel P, Leumann E, Neuhaus TJ (2002) Immunization in children with chronic renal failure. Pediatr Nephrol 17:638–642
Breuer J, Schmid DS, Gerson AA (2008) Use and limitations of varicella-zoster virus-specific serological testing to evaluate breakthrough disease in vaccinees and to screen for susceptibility to varicella. J Infect Dis 197:S147–S151
Feldman S, Hughes WT, Daniel CB (1975) Varicella in children with cancer: seventy-seven cases. Pediatrics 56:388–397
Izurieta HS, Strebel PM, Blake PA (1997) Postlicensure effectiveness of varicella vaccine during an outbreak in a child care center. JAMA 278:1495–1499
Smith JG, Liu X, Kaufhold RM, Clair J, Caulfield MJ (2001) Development and validation of a gamma interferon ELISPOT assay for quantitation of cellular immune responses to varicella-zoster virus. Clin Diagn Lab Immunol 8:871–879
Vossen MT, Gent MR, Weel JF, de Jong MD, van Lier RA, Kuijpers TW (2004) Development of virus-specific CD4+ T cells on reexposure to varicella-zoster virus. J Infect Dis 190:72–82
Weinberg A, Horslen SP, Kaufman SS, Jesser R, Devoll-Zabrocki A, Fleckten BL, Kochanowicz S, Seipel KR, Levin MJ (2006) Safety and immunogenicity of varicella-zoster virus vaccine in pediatric liver and intestine transplant recipients. Am J Transplant 6:565–568
Starko KM, Ray CG, Dominguez LB, Stromberg WL, Woodall DF (1980) Reyes syndrome and salicylate use. Pediatrics 66:859–864
Lesko SM, O'Brien KL, Schwartz B, Vezina R, Mitchell AA (2001) Invasive group A streptococcal infection and nonsteroidal antiinflammatory drug use among children with primary varicella. Pediatrics 107:1108–1115
Zerr DM, Alexander ER, Duchin JS, Koutsky LA, Rubens CE (1999) A case-control study of necrotizing fasciitis during primary varicella. Pediatrics 103:783–790
Academy of Pediatrics Committee on Infectious Diseases (1993) The use of oral aciclovir in otherwise healthy children with varicella. Pediatrics 91:858
Balfour HH, Kelly JM, Suarez CS, Heussner RC, Englund JA, Crane DD, McGuirt PV, Clemmer AF, Aeppli DM (1990) Aciclovir treatment of varicella in otherwise healthy children. J Pediatr 116:633–639
Enright AM, Prober CG (2003) Antiviral therapy in children with varicella zoster virus and herpes simplex virus infections. Herpes 10:32–37
Shepp DH, Dandliker PS, Meyers JD (1986) Treatment of varicella zoster virus-infection in severely immunocompromised patients - A randomized comparison of aciclovir and vidarabine. N Engl J Med 314:208–212
Fishman JA, Rubin RH (1998) Infection in organ-transplant recipients - Reply. N Engl J Med 339:1246
Zeng L, Nath CE, Blair EY, Shaw PJ, Stephen K, Earl JW, Coakley JC, McLAchlan AJ (2009) Population pharmacokinetics of acyclovir in children and young people with malignancy after administration of intravenous acyclovir or oral valacyclovir. Antimicrob Agents Chemother 53:2918–2927
Brigden D, Bye A, Fowle AS, Rogers H (1981) Human pharmacokinetics of acyclovir (an antiviral agent) following rapid intravenous injection. J Antimicrob Chemother 7:399–404
Dunkle LM, Arvin AM, Whitley RJ, Rotbart HA, Feder HM Jr, Feldman S, Gershon AA, Levy ML, Hayden GF, McGuirt PV (1991) A controlled trial of aciclovir for chickenpox in normal children. N Engl J Med 325:1539–1544
Yoshikawa T, Suga S, Kozawa T, Kawaguchi S, Asano Y (1998) Persistence of protective immunity after postexposure prophylaxis of varicella with oral aciclovir in the family setting. Arch Dis Child 78:61–63
Huang YC, Lin TY, Chiu CH (1995) Aciclovir prophylaxis of varicella after household exposure. Pediatr Infect Dis J 14:152–154
Asano Y, Yoshikawa T, Suga S, Kobayashi I, Nakashima T, Yazaki T, Ozaki T, Yamada A, Imanishi J (1993) Postexposure prophylaxis of varicella in family contact by oral aciclovir. Pediatrics 92:219–222
Beutner KR, Friedman DJ, Forszpaniak C, Andersen PL, Wood MJ (1995) Valaciclovir compared with aciclovir for improved therapy for herpes zoster in immunocompetent adults. Antimicrob Agents Chemother 39:1546–1553
Faulds D, Heel RC (1990) Ganciclovir - A review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy in cytomegalovirus infections. Drugs 39:597–638
McGregor RS, Zitelli BJ, Urbach AH, Malatack JJ, Gartner JC (1989) Varicella in pediatric orthotopic liver-transplant recipients. Pediatrics 83:256–261
Van Der Zwet EC, Vandenbroucke-Grauls CM, van Elburg RM, Cranedonk A, Zaaijer HL (2002) Neonatal antibody titers against varicella-zoster virus in relation to gestational age, birth weight, and maternal titer. Pediatrics 109:79–85
Zaia JA, Levin MJ, Preblud SR, Leszczynski J, Wright GG, Ellis RJ, Curtis AC, Valerio MA, LeGore J (1983) Evaluation of varicella-zoster immune globulin - protection of immunosuppressed children after household exposure to varicella. J Infect Dis 147:737–743
Arbeter AM, Granowetter L, Starr SE, Lange B, Wimmer R, Plotkin SA (1990) Immunization of children with acute lymphoblastic-leukemia with live attenuated varicella vaccine without complete suspension of chemotherapy. Pediatrics 85:338–344
Brunell PA, Shehab Z, Geiser C, Waugh JE (1982) Administration of live varicella vaccine to children with leukemia. Lancet 2:1069–1073
Levin MJ, Gershon AA, Weinberg A, Blanchard S, Nowak B, Palumbo B, Chan CY (2001) Immunization of HIV-infected children with varicella vaccine. J Pediatr 139:305–310
Rivest P, Bedard L, Valiquette L, Mills E, Lebel MH, Lavoie G, Carsley J (2001) Severe complications associated with varicella: province of Quebec, April 1994 to March 1996. Can J Infect Dis 12:21–26
Ljungman P, Lönnqvist B, Ringdén O, Skinhöj P, Gahrton G (1989) A randomized trial of oral versus intravenous aciclovir for treatment of herpes zoster in bone marrow transplant recipients. Nordic Bone Marrow Transplant Group. Bone Marrow Transplant 4:613–615
Kashtan CE, Cook M, Chavers BM, Mauer SM, Nevins TE (1997) Outcome of chickenpox in 66 pediatric renal transplant recipients. J Pediatr 131:874–877
Broyer M, Tete MJ, Guest G, Gagnadoux MF, Rouzioux C (1997) Varicella and zoster in children after kidney transplantation: long-term results of vaccination. Pediatrics 99:35–39
Lauzurica R, Bayes B, Frias C, Fontseré N, Hernandez A, Matas L, Jimenez A, Bonet J, Romero R (2003) Disseminated varicella infection in adult renal allograft recipients: Role of mycophenolate mofetil. Transplant Proc 35:1758–1759
Jose MD, Roake JA, Robson RA (2000) The role of mycophenolate mofetil in chickenpox after renal transplantation. Transplantation 70:242–243
Hayes K, Shakuntala V, Pingle A, Dhawan IK, Masri MA (1992) Safe use of aciclovir (Zovirax) in renal-transplant patients on cyclosporine-A therapy – case reports. Transplant Proc 24:1926
Fehr T, Bossart W, Wahl C, Binswanger U (2002) Disseminated varicella infection in adult renal allograft recipients: four cases and a review of the literature. Transplantation 73:608–611
Boeckh M, Kim HW, Flowers MED, Meyers JD, Bowden RA (2006) Long-term aciclovir for prevention of varicella zoster virus disease after allogeneic hematopoietic cell transplantation—a randomized double-blind placebo-controlled study. Blood 107:1800–1805
Asano-Mori Y, Kanda Y, Oshima K, Kako S, Shinohara A, Nakasone H, Sato H, Watanabe T, Hosoya N, Izutsu K, Asai T, Hangaishi A, Motokura T, Chiba S, Kurokawa M (2008) Long-term ultra-low-dose aciclovir against varicella-zoster virus reactivation after allogeneic hematopoietic stem cell transplantation. Am J Hematol 83:472–476
Kim DH, Kumar D, Messner HA, Minden M, Gupta V, Kuruvilla J, Chae YS, Sohn SK, Lipton JH (2008) Clinical efficacy of prophylactic strategy of long-term low-dose aciclovir for varicella-zoster virus infection after allogeneic peripheral blood stem cell transplantation. Clin Transplant 22:770–779
Aitken C, Hawrami K, Miller C, Muir WB, Yaqoob M, Breuer J (1999) Simultaneous treatment of cytomegalovirus and varicella zoster infections in a renal transplant recipient with ganciclovir: use of viral load to monitor response to treatment. J Med Virol 59:412–414
Steer CB, Szer J, Sasadeusz J, Matthews JP, Beresford JA, Grigg A (2000) Varicella-zoster infection after allogeneic bone marrow transplantation: incidence, risk factors and prevention with low-dose aciclovir and ganciclovir. Bone Marrow Transplant 25:657–664
Dodd DA, Burger J, Edwards KM, Dummer JS (2001) Varicella in a pediatric heart transplant population on nonsteroid maintenance immunosuppression. Pediatrics 108:e80
Goldstein SL, Somers MJG, Lande MB, Brewer ED, Jabs KL (2000) Aciclovir prophylaxis of varicella in children with renal disease receiving steroids. Pediatr Nephrol 14:305–308
Gershon A, Brunell PA, Claps AA, Doyle EF (1972) Steroid-therapy and varicella. J Pediatr 81:1034
Kasper WJ, Howe PM (1990) Fatal varicella after a single course of corticosteroids. Pediatr Infect Dis J 9:729–732
Harmon WE (1991) Opportunistic infections in children following renal-transplantation. Pediatr Nephrol 5:118–125
Melzi ML, Sonzogni A, Comoli P, Stroppa P, Riva S, Altobelli M, Casati A, Torre G, Alberti D, Guizzetti M, Furione M, Spada M, Colledan M, Gridelli B (2006) Specific autologous cytotoxic T lymphocytes for chronic varicella in a liver transplanted child. Pediatr Transplant 10:240–243
Gershon AA, LaRussa P, Hardy I, Steinberg S, Silverstein S (1992) Varicella vaccine—the American experience. J Infect Dis 166:S63–S68
Krause PR, Klinman DM (1995) Efficacy, immunogenicity, safety, and use of live attenuated chickenpox vaccine. J Pediatr 127:518–525
Rodriguez-Moreno A, Sanchez-Fructuoso AI, Calvo N, Ridao N, Conesa J, Marquez M, Prats D, Barrientos A (2006) Varicella infection in adult renal allograft recipients: experience at one center. Transplant Proc 38:2416–2418
Errasti P, Alvarez ML, Gomez G, Lavilla FJ, Garcia N, Ballester B, García I, Purroy A (1999) Chickenpox in four adult renal transplant recipients. Transplant Proc 31:2341–2342
Shahbazian H, Ehsanpour A (2007) An outbreak of chickenpox in adult renal transplant recipients. Exp Clin Transplant 5:604–606
Robertson S, Newbigging K, Carman W, Jones G, Isles C (2006) Fulminating varicella despite prophylactic immune globulin and intravenous aciclovir in a renal transplant recipient: should renal patients be vaccinated against VZV before transplantation? Clin Transplant 20:136–138
Ishikawa N, Tanabe K, Shimmura H, Tokumoto T, Toma H (2000) Primary varicella virus in adult renal transplant recipients: case reports. Transplant Proc 32:1952–1953
Levitsky J, Te HS, Faust TW, Cohen SM (2002) Varicella infection following varicella vaccination in a liver transplant recipient. Am J Transplant 2:880–882
Pacini-Edelstein SJ, Mehra M, Ament ME, Vargas JH, Martin MG, McDiarmid TV (2003) Varicella in pediatric liver transplant patients: a retrospective analysis of treatment and outcome. J Pediatr Gastroenterol Nutr 37:183–186
Levitsky J, Kalil AC, Meza JL, Hurst GE, Freifeld A (2005) Chicken pox after pediatric liver transplantation. Liver Transplant 11:1563–1566
Donati M, Zuckerman M, Dhawan A, Hadzic N, Heaton N, North-Lewis P, Mieli-Vergani G (2000) Response to varicella immunization in pediatric liver transplant recipients. Transplantation 70:1401–1404
Carby M, Jones A, Burke M, Hall A, Banner N (2007) Varicella infection after heart and lung transplantation: a single-center experience. J Heart Lung Transplant 26:399–402
Cabezón Ruiz SC, Cisneros JM, Lage Galle EL, Ordónez A, Hinojosa RF, Moràn Risco JE, Hernández A (2003) Characteristics and repercussion of varicella-zoster virus infection in cardiac transplant. Transplant Proc 35:2004–2005
Vossen MTM, Gent MR, Weel JFL, de Jong MD, van Lier RAW, Kuijpers TW (2004) Development of virus-specific CD4+ T cells on reexposure to varicella-zoster virus. J Infect Dis 190:72–82
Watson B, Rothstein E, Bernstein H, Arbeter A, Arvin A, Chartrand S, Clements D, Kumar ML, Reisinger K, Blatter M, Starr SE, Staehle B, Ngai A, White CJ (1995) Safety and cellular and humoral immune responses of a booster dose of varicella vaccine 6 years after primary immunization. J Infect Dis 172:217–219
Zerboni L, Nader S, Aoki K, Arvin AM (1998) Analysis of the persistence of humoral and cellular immunity in children and adults immunized with varicella vaccine. J Infect Dis 177:1701–1704
Watson B (2008) Humoral and cell-mediated immune responses in children and adults after 1 and 2 doses of varicella. J Infect Dis 197:S143–S146
Weinberg A, Levin MJ (2010) VZV T cell-mediated immunity. Curr Top Microbiol Immunol 342:341–357
Prelog M, Zimmerhackl LB (2010) Varicella vaccination in pediatric kidney and liver transplantation. Pediatr Transplant 14:41–47
Zamora I, Simon JM, Da Silva ME, Piqueras AI (1994) Attenuated varicella virus vaccine in children with renal transplants. Pediatr Nephrol 8:190–192
Weinberg A, Horslen SP, Kaufman SS, Jesser R, Devoll-Zabrocki A, Fleckten BL, Kochanowicz S, Seipel KR, Levin MJ (2006) Safety and immunogenicity of varicella-zoster virus vaccine in pediatric liver and intestine transplant recipients. Am J Transplant 6:565–568
Kano H, Mizuta K, Sakakihara Y, Kato H, Miki Y, Shibuya N, Saito M, Norita M, Kawarasaki H, Igarashi T, Hashizume K, Iwata T (2002) Efficacy and safety of immunization for pre- and post-liver transplant children. Transplantation 74:543–550
Olson AD, Shope TC, Flynn JT (2001) Pretransplant varicella vaccination is cost-effective in pediatric renal transplantation. Pediatr Transplant 5:44–50
Fadrowski JJ, Furth SL (2004) Varicella zoster virus: vaccination and implications in children with renal failure. Expert Rev Vaccines 3:291–298
Kitai IC, King S, Gafni A (1993) An economic-evaluation of varicella vaccine for pediatric liver and kidney-transplant recipients. Clin Infect Dis 17:441–447
Author information
Authors and Affiliations
Corresponding author
Additional information
Lothar Bernd Zimmerhackl is deceased.
Rights and permissions
About this article
Cite this article
Prelog, M., Schönlaub, J. & Zimmerhackl, L.B. Aciclovir and Varicella-zoster-immunoglobulin in solid-organ transplant recipients. Pediatr Nephrol 26, 663–673 (2011). https://doi.org/10.1007/s00467-010-1666-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-010-1666-z