Abstract.
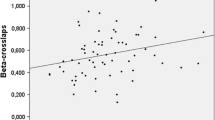
Some children with idiopathic hypercalciuria (IH) develop bone alterations at some stage of the disease. The aims of this study were to evaluate bone mass in 88 children with IH (G1) at the time of diagnosis and to compare the findings with data for a control group of 29 normal children (G2). Kidney and bone metabolism markers were measured in both groups, and bone densitometry was performed. Serum alkaline phosphatase, intact parathyroid hormone, urinary calcium and uric acid were significantly higher in G1, whereas urinary volume and urinary citrate excretion were lower. The following densitometric parameters were significantly lower in G1: (1) lumbar spine (L2-L4) bone mineral density (BMD), bone mineral content (BMC), BMC corrected for height and for width of the vertebra, volumetric BMD (BMDvol), and Z score; (2) whole-body BMD; (3) femoral neck BMD. Lumbar spine BMDvol was reduced (osteopenia) in 35% of the patients compared with G2. N telopeptide, a urinary marker of bone resorption, was significantly higher in G1 than in G2, and was negatively correlated with lumbar spine BMD and BMDvol. Children with urinary lithiasis or idiopathic hyperuricosuria associated with IH showed no significant differences in bone metabolism compared with children without these associations. We conclude that (1) there is an altered bone metabolism in IH, with osteopenia already present at diagnosis in 35% of the patients; (2) N telopeptide is one of the most useful markers of bone alterations in IH, especially at an early stage of the disease; (3) investigation of bone metabolism is necessary in IH to prevent future serious consequences such as osteoporosis and bone fractures.


Similar content being viewed by others
References
Heilberg IP, Martini LA, Szejnfeld VL, Carvalho AB, Draibe SA, Ajzen H, Ramos OL, Schor N (1994) Bone disease in calcium stone forming patients. Clin Nephrol 42:175–182
García-Nieto V, Ferrández C, Monge M, Sequera M, Rodrigo MD (1997) Bone mineral density in pediatric patients with idiopathic hypercalciuria. Pediatr Nephrol 11:578–583
Perrone HC, Marone MMS, Bianco AC, Toporovski J, Malvestiti LF, Schor N (1995) Bone mineral density in hypercalciuric children: a 5-year follow-up (abstract), The 10th Congress of the International Pediatric Nephrology Association, Santiago, Chile, 27 Aug to 1 Sept
Fässler ALC, Bonjour JP (1995) Osteoporosis as a pediatric problem. Pediatr Clin North Am 42:811–824
Carrascosa A, Gussynié M, Yeste D, Del Rio L, Audí L (1995) Bone mass acquisition during infancy, childhood and adolescence. Acta Paediatr [Suppl] 411:18–23
Pacifici R, Rothstein M, Rifas L, Lau KH, Baylink DJ, Avioli LV, Hruska K (1990) Increased monocyte interleukin-1 activity and decreased vertebral bone density in patients with fasting idiopathic hypercalciuria. J Clin Endocrinol Metab 71:138–145
Weisinger JR, Alonzo E, Carlini RG, Paz-Martinez V, Martinis R, Bellorin-Font E (1998) Bone disease in hypercalciuria: a new form of osteodystrophy? Nephrol Dial Transplant 13 [Suppl 3]:88–90
Filipponi P, Mannarelli C, Pacifici R, Grassi E, Moertti I, Tint S, Carlone C, Blass A, Morucci P, Hruska KA, Avioli LV (1988) Evidence for a prostaglandin-mediated bone resorptive mechanism in subjects with fasting hypercalciuria. Calcif Tissue Int 43:61–66
Trinchieri A, Nespoli R, Rovera F, Ostini F, Vezzoli G, Zerbi S, Rubinacci A, Moro GL, Curro A (1995) Diet and bone mineral content in idiopathic calcium renal stone formers. Proceedings of Sixth European synposium on urolithiasis. 8–10 June, Stockholm. Tiselius, Stockholm 1:160
Bataille P, Achard JM, Fournier A, Boudailliez B, Westeel PF, el Esper N, Bergot C, Jans I, Lalau JD, Petit J (1991) Diet, vitamin D and vertebral mineral density in hypercalciuric calcium stone formers. Kidney Int 39:1193–1205
Marcondes E, Machado DVM, Setian N, Carrazza FR (1991) Crescimento e desenvolvimento. In: Marcondes E (ed) Pediatria Básica, 8th edn. Savier, São Paulo, pp 35–63
Simkin PA, Hoover PL, Paxson CS, Wilson WF (1979) Uric acid excretion: quantitative assessment from spot, midmorning serum and urine samples. Ann Intern Med 91:44–47
Shimizu T, Nishikawa M, Matsushige H (1990) The solubility of uric acid and monosodium urate in urine. Adv Exp Med Biol 253A:215–218
Tiselius HG (1980) Practical aspects of the handling of samples and evaluation of laboratory data. Scand J Urol Nephrol 53:105–108
Husain SM, Mughal Z, Williams G, Ward K, Smith CS, Dutton J, Fraser WD (1999) Urinary excretion of pyridinium crosslinks in healthy 4–10 year olds. Arch Dis Child 80:370–373
Jacobs DS, Kasten BL, Demott WR (ed) (1990) Laboratory test handbook, 2nd edn. Williams and Wilkins, Baltimore
Henry JB (1991) Clinical diagnosis and management by laboratory methods, 18th edn. Saunders, Philadelphia
Dacie JV, Lewis SM (1991) Practical haematology, 7th edn. Churchill Livingstone, London
Scariano JK, Walter EA, Glew RH, Hollis BW, Henry A, Ocheke I, Isichei CO (1995) Serum levels of the pyridinoline crosslinked carboxyterminal telopeptide of type I collagen (ICTP) and osteocalcin in rachitic children in Nigeria. Clin Biochem 28:541–545
Rauch FR, Stabrey A, Schönau E (1996) Appendix: reference values in pediatric osteology. In: Schönau E (ed) Paediatric osteology: new developments in diagnostics and therapy. Elsevier Science, Amsterdam, pp 295–300
Greulich WW, Pyle SI (1993) The rationale and technique of assessing the developmental status of children from roentgenograms of hand and wrist. In: Radiographic atlas of skeletal development of hand and wrist, 2nd edn. Stanford University Press, Stanford
Laursen EM, Molgaard C, Michaelsen KF, Koch C, Muller J (1999) Bone mineral status in 134 patients with cystic fibrosis. Arch Dis Child 81:235–240
Kröger HPJ (1996) Measurement of bone mass and density in children. In: Schönau E (ed) Paediatric osteology: new developments in diagnostics and therapy. Elsevier Science, Amsterdam, pp 103–108
Del Rio L, Carrascosa A, Pons F, Gussynié M, Yeste D, Domenech FM (1994) Bone mineral density of the lumbar spine in Caucasian Mediterranean Spanish children and adolescents: changes related to age, sex and puberty. Pediatr Res 35:362–366
Thomas KA, Cook SD, Bennett JT, Whitecoud III TS, Rice JC (1991) Femoral neck and lumbar spine bone mineral densities in a normal population 3–20 years of age. J Pediatr Orthop 11:48–58
Perrone HC, Ajzen H, Toporovski J, Schor N (1991) Metabolic disturbance as a cause of recurrent hematuria in children. Kidney Int 39:807–811
Heilberg IP, Schor N (1994) Litíase renal: fisiopatogenia e tratamento. J Bras Nefrol 16:125–133
Pak CY, Oata M, Lawrence EC, Snyder W (1974) The hypercalciurias. Causes, parathyroid functions, and diagnostic criteria. J Clin Invest 54:387–400
Broadus AE, Lang R, Kliger AS (1981) The influence of calcium intake and the status of intestinal calcium absorption on the diagnostic utility of measurements of 24-hour cyclic adenosine 3',5'-monophosphate excretion. J Clin Endocrinol Metab 52:1085–1089
Sutton RA, Walker VR (1980) Responses to hydrochlorothiazide and acetazolamide in patients with calcium stones. N Engl J Med 302:709–713
Barros EJ, Santos DR dos, Boim MA, Pinheiro ME, Ajzen H, Ramos OL, Schor N (1986) Calciúria, sobrecarga de cálcio e AMP cíclico urinário na avaliação de pacientes com litíase cálcica. AMB Rev Assoc Med Bras 32:96–100
Ejersted C, Andreassen TT, Hauge EM, Melsen F, Oxlund H (1995) Parathyroid hormone (1–34) increases vertebral bone mass, compressive strength, and quality in old rats. Bone 17:507–511
Boechat MI, Westra SJ, Van Dop C, Kaufman F, Gilzanz V, Roe TF (1996) Decreased cortical and increased cancellous bone in two children with primary hyperparathyroidism. Metabolism 45:76–81
Gabay C, Ruedin P, Slosman D, Bonjour JP, Leski M, Rizzoli R (1993) Bone mineral density in patients with end-stage renal failure. Am J Nephrol 13:115–123
Kruse K, Kracht U (1986) Evaluation of serum osteocalcin as an index of altered bone metabolism. Eur J Pediatr 145:27–33
Hosking DH, Erickson SB, Van den Berg CJ, Wilson DM, Smith LH (1983) The stone clinic effect in patients with idiopathic calcium urolithiasis. J Urol 130:1115–1118
Weaver CM, Peacock M, Martin BR, McCabe GP, Zhao J, Smith DL, Wastney ME (1997) Quantification of biochemical markers of bone turnover by kinetic measures of bone formation and resorption in young healthy females. J Bone Miner Res 12:1714–1720
Kikushi T, Hashimoto N, Kawasaki T, Kataoka S, Takahashi H, Uchiyama M (1998) Plasma levels of carboxy terminal propeptide of type I procollagen and pyridinoline cross-linked telopeptide of type I collagen in healthy school children. Acta Paediatr 87:825–829
Kyd PA, De Vooght K, Kerkhoff F, Thomas E, Fairney A (1999) Clinical usefulness of biochemical resorption markers in osteoporosis. Ann Clin Biochem 36:483–491
Longobardi S, Di Rella F, Pivonello R, Di Somma C, Klain M, Maurelli L, Scarpa R, Colao A, Merola B, Lombardi G (1999) Effects of two years of growth hormone (GH) replacement therapy on bone metabolism and mineral density in childhood and adulthood onset GH deficient patients. J Endocrinol Invest 22:333–339
Taga M, Uemura T, Minaguchi H (1998) The effect of hormone replacement therapy in postmenopausal women on urinary C-telopeptide and N-telopeptide of type I collagen, new markers of bone resorption. J Endocrinol Invest 21:154–159
Perrone HC, Lewin S, Langman CB, Toporovski J, Marone M, Schor N (1992) Bone effects of the treatment of children with absorptive hypercalciuria. Pediatr Nephrol 6:C115
Perrone HC, Marone MMS, Bianco AC, Toporovski J, Malvestiti LF, Schor N (1995) Bone mineral density in hypercalciuric children: a 5 year follow-up (abstract). The 10th Congress of the International Pediatric Nephrology Association, Santiago, Chile, 27 Aug to 1 Sept
Silva AMM (1995) Avaliação metabólica, histomorfométrica e do conteúdo mineral ósseo de pacientes portadores de nefrolitíase cálcica recorrente e hipercalciúria idiopática. Faculdade de Medicina da Universidade Federal de São Paulo, São Paulo, 101p (Tese de Doutorado)
García-Nieto V, Navarro JF, Ferrández C (1998) Bone loss in children with idiopathic hypercalciuria. Nephron 78:341–342
Freundlich J, Haimberg E, Bellorín-Font E, Weisinger JR (1999) Osteopenia in asymptomatic premenopausal mothers of children with idiopathic hypercalciuria (abstract). XXth International Congress of Nephrology, Buenos Aires, Argentina, 2–6 May, p 280
Acknowledgements.
This study was presented at the International Pediatric Nephrology Association Meeting in September 2001 at Seattle, USA. We thank Dr. José-Silvério Diniz for scientific support. This work was supported by the Pediatric Nephrology Unit, Faculty of Medicine (UFMG), Brazil. We also thank the following groups that played an important role in the development and performance of this study: (1) Pós-graduação UFMG; (2) CNPq; (3) Instituto de Patologia Clínica Hermes Pardini; (4) ECOAR Medicina Diagnóstica.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Penido, MG.M.G., Lima, E.M., Marino, V.S.P. et al. Bone alterations in children with idiopathic hypercalciuria at the time of diagnosis. Pediatr Nephrol 18, 133–139 (2003). https://doi.org/10.1007/s00467-002-1036-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-002-1036-6