Abstract
Background
The ideal treatment of epithelial neoplastic rectal lesions involving the dentate line is a controversial issue. Piecemeal endoscopic mucosal resection (EMR) is the most commonly used resection technique, but it is associated with high recurrence rates. Endoscopic submucosal dissection (ESD) has been shown to be safe and effective for the treatment of rectal lesions, but evidence is lacking concerning its application close to the dentate line. The aim of our study is to compare ESD and EMR for the treatment of epithelial rectal lesions involving the dentate line.
Methods
We identified all cases of endoscopic resections of rectal lesions involving the dentate line performed in two German high-volume centers between 2010 and 2022. Periinterventional and follow-up data were collected and retrospectively analyzed.
Results
We identified 68 ESDs and 62 EMRs meeting our inclusion criteria. ESD showed a significant advantage in en bloc resection rates (89.7% vs. 9.7%; P = 0.001) and complete resection rates (72.1% vs. 9.7%; P = 0.001). The overall curative resection rate was similar between both groups (ESD: 92.6%, EMR: 83.9%; P = 0.324), whereas in the subgroup of low-risk adenocarcinomas ESD was curative in 100% of the cases vs. 14% in the EMR group (P = 0.002). There was one local recurrence after ESD (1,5%) vs. 16 (25.8%) after EMR (P < 0.0001), and the EMR patients required an average of three further interventions.
Conclusion
ESD is superior to EMR for the treatment of epithelial rectal lesions involving the dentate line and should be considered the treatment of choice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Endoscopic resection is the treatment of choice for colorectal adenomas and low-risk early adenocarcinomas [1]. The evolution of local resection techniques has resulted in a wide spectrum of therapeutic options. These include endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), endoscopic full-thickness resection (EFTR), and transanal endoscopic microsurgery (TEM), which alone or in combination with each other and with ablative techniques can effectively treat lesions in the entire colorectum. Nevertheless, some localizations remain challenging even for experienced endoscopists. Epithelial lesions in the lower rectum that are in close proximity to or involve the dentate line have been historically considered difficult to treat endoscopically, mainly because of the poor visualization and maneuverability of the endoscope, resulting in many patients being referred for surgery [2].
Although technical advances in EMR currently yield high success rates of the primary resection, piecemeal EMR (pmEMR) of larger lesions is associated with high recurrence rates [2, 3]. Additionally, the fragmentation of the resected specimen does not allow for an accurate evaluation of the stage and resection status in cases of occult carcinomas, thus leading to patients with potentially endoscopically curable tumors having to undergo oncologic surgery [4]. ESD enables en bloc resection of colorectal lesions regardless of their size, with recurrence rates of 0–2%, and can be curative for low-risk carcinomas. However, as ESD is time consuming and technically challenging, it is not considered first-line treatment in most centers, especially in the Western world [5,6,7]. A few retrospective studies have demonstrated the advantages of ESD for lesions in the lower rectum involving the dentate line and have shown similar results to procedures performed higher in the rectum [8,9,10]. However, no studies have directly compared ESD with EMR for the treatment of these challenging lesions. Thus, the aim of our study is to compare the periinterventional and long-term outcomes of ESD and EMR for the resection of epithelial lesions of the lower rectum involving and in close proximity to the dentate line, focusing on technical success, curative resection rates, and local recurrence.
Materials and methods
Study design and inclusion criteria
We retrospectively analyzed all patients that underwent endoscopic resection for epithelial lesions located in the lower rectum involving the dentate line at the University Medical Center Mannheim and the Marburg University Hospital between 2010 and 2022. We included all laterally spreading tumors (LST) without macroscopic signs of malignancy with a minimum size of 20 mm and all flat epithelial lesions with suspicion of low-grade malignancy regardless of their size, the anal margin of which was within 2 cm of the dentate line. In all cases the resected area included the dentate line in order to achieve a complete resection of the tumor. The distance of the anal margin of the lesion from the dentate line was measured using the markings on the flexible endoscope. Macroscopic evaluation of malignancy was based on the Japanese Narrow Band Imaging Expert Team—JNET—classification [11].
Approval of the ethics committees of both participating university hospitals was acquired (Ruprecht-Karl University of Heidelberg, file reference 2023-847; Philipps University of Marburg, file reference 23-156 RS).
Based on the type of endoscopic resection, patients were split into two groups: the ESD group and the EMR group. All procedures were performed or directly supervised by four senior endoscopists (K.K., U.D., G.K., S.B.).
Endoscopic resection technique
ESD
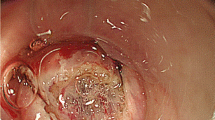
Rectal ESDs were performed using a diagnostic or therapeutic gastroscope. The resection margins were marked circumferentially (Fig. 1). Glycerol or plasma expanders with the addition of methylene blue or toluidine blue dye were used for the submucosal injection. Adrenaline 1:100,000 and lidocaine 1% were occasionally added to the solution during submucosal injection in the anal canal. After submucosal injection, the initial, superficial incision was performed using the DualKnife J® (Olympus Europa SE & Co. KG, Hamburg, Germany) starting on the oral side of the lesion, usually in the retroflex position. Circumferential incision was continued to the anal side in the squamous epithelium of the anal canal, with particular caution taken to avoid injury to the hemorrhoidal veins. These were carefully dissected and coagulated before being transected, to avoid excessive intraprocedural bleeding. After the submucosal plane was entered, submucosal dissection was performed until a stable plane was established (Fig. 2). Subsequently, submucosal dissection was continued using the flap or pocket-creation technique, depending on the morphology of the lesion and the endoscopist’s preference. In some cases of flap technique additional traction, usually with the clin-n’-line method, was utilized (Fig. 3). Once the resection was completed, the mucosal defect was carefully inspected and visible vessels were coagulated to prevent secondary bleeding. The resected specimen was stretched, pinned on a cork plate, and photodocumented before being sent for histopathological examination.
ESD of 45mm large LST granular type, homogenous. a The anal margin of the lesion grows into the squamous epithelium of the anal canal. b Visualization of the marked lesion in retroflex view. c Markings on the anal side of the lesion in the squamous epithelium of the anal canal. d Resection defect in the anal canal. e Mucosal defect after completion of the ESD in retroflex view. f ESD specimen: 45 × 40mm large tubular adenoma with high-grade dysplasia—complete en bloc resection with free deep and lateral margins
ESD of an 120mm large LST granular mixed type with occult carcinoma (pocket creation method). a Visualization of the lesion in retroflex view. b The lesion reaches the oral end of the anal canal. c Marking of the anal resection margin in the squamous epithelium of the anal canal. d Submucosal injection in the anal canal. e Epithelial incision and entering the submucosal plane at the oral part of the anal canal. The fibers of the internal anal sphincter are visible. f Visualization of the hemorrhoidal veins in the submucosal plane. g Epithelial defect in the anal canal. The hemorrhoidal veins are visible. h Visualization of the mucosal defect in retroflex view. i ESD specimen: a pT1sm1 L0 V0 G2 adenocarcinoma within a 120 × 90mm large tubulovillous adenoma with high-grade dysplasia—complete en bloc resection with free deep and lateral margins (R0)
ESD of a 180mm large LST granular mixed type (flap method) with endoscopic follow-up. a Visualization of the Lesion in forward view. b Circumferential mucosal incision on the oral side of the lesion. c Circumferential mucosal incision in the anal canal with visualization of the hemorrhoidal veins. d Use of traction (clip-n’-line technique) after initial submucosal dissection in the anal side of the lesion. e Exposure of the submucosal plane and the muscle layer with the use of traction. f Visualization of the mucosal defect in forward view after prophylactic clipping of large vessels. g Visualization of the resection defect in the anal canal. h ESD specimen: 184 × 130mm large tubulovillous adenoma with high-grade dysplasia—complete en bloc resection with free deep and lateral margins (R0). i Endoscopic follow-up 15 months after the initial procedure showing the scar without any signs of recurrence
EMR
A diagnostic or therapeutic gastroscope was also used for rectal EMR. Submucosal injection was performed with either Glycerol/Gelafundin and methylene blue or toluidine blue dye using a standard injection needle or normal saline solution through the HyrdoJet® flexible applicator (Erbe Elektromedizin GmbH, Tübingen, Germany). Adrenaline 1:100,000 and lidocaine 1% were occasionally added to the solution during submucosal injection in the anal canal. Both monofilament and braided snares measuring 15–30 mm were used for the resection, depending on the morphology of the lesion and the endoscopist’s preference. After completion of the resection, the mucosal defect was carefully inspected for remaining tumor tissue and if identified, the tumor tissue was removed with the snare or the biopsy forceps (Fig. 4). After 2018, thermal ablation of the resection margin was performed using the snare tip or argon plasma coagulation. Visible vessels were also coagulated.
EMR of a 40mm large LST granular type, homogenous (Histology: tubulovillous adenoma with low-grade dysplasia). a Visualization of the adenoma in retroflex view. b Adequate lifting after submucosal injection. c pmEMR beginning on the oral side in retroflex view. d Mucosal defect after complete resection of the lesion
Data acquisition
The periinterventional and follow-up data were extracted from the endoscopic databases and the electronic clinical records of the participating centers (Clinic WinData, E&L GmbH, Erlangen, Germany; ORBIS KIS, Dedalus Healthcare, Bonn, Germany; EPOS, SAP, Weinheim, Germany), anonymized, and retrospectively analyzed.
The following data were recorded for the included patients: basic demographic characteristics; lesion morphology and localization; procedure time; lesion size, histology, and resection status as described in the pathology report; and periprocedural and long-term complications and local recurrence. Follow-up time was defined based on the latest available endoscopic control examination.
The primary endpoints of our study were curative resection rate and local recurrence rate. Curative resection was defined as a macroscopically complete resection with no visible residual tissue for adenomas and as an R0 resection of a low-risk adenocarcinoma. Secondary endpoints included en bloc resection rate, histologically complete resection rate, procedure time, and adverse events.
The collected parameters were compared between the ESD group and the EMR group.
A subgroup analysis was undertaken comparing the curative resection rate between adenomas and carcinomas. In the latter, low-risk carcinomas were defined as well and moderately differentiated (G1-G2) T1 carcinomas with a maximum submucosal infiltration of 2000 µm (T1sm2) without signs of venous or lymphovascular invasion (V0 and L0).
Statistical analysis
The statistical analysis was performed using IBM SPSS Statistics 28.0. Categorical variables were compared using a chi-square test or Fischer’s exact test, and continuous variables were compared using Student’s t-test or a Mann–Whitney test. Statistical significance was defined as P < 0.05.
Results
We identified 130 patients who fulfilled our inclusion criteria, of whom 68 were in the ESD group and 62 in the EMR group. Age (ESD group: 67 years vs. EMR group: 66 years; P = 0.714) and sex distribution (ESD group: 43 male/25 female, EMR group: 33 male/29 female; P = 0.247) were similar between the two groups. In the initial study period, between 2010 and 2018, we identified 4 ESD cases and 45 EMR cases, whereas in the later study period, between 2019 and 2020, ESD was more common with 64 ESD cases and 17 EMR cases (P < 0.00001). The median size of the resected lesions was similar between both groups (ESD group 36 mm, EMR group 33 mm; P = 0.363).
The median distance of the lesions from the dentate line was 1 cm in both groups (P = 0.815), and the resection area included the dentate line in all cases. Five lesions in each group were recurrent adenomas after previous pmEMR or TEM (P = 0.879). The histological distribution of the resected lesions is depicted in Table 1.
In the ESD group there were nine hybrid procedures, combining ESD with EMR or EFTR. Since our analysis was based on an intention to treat model and hybrid procedures were started as ESD and converted to hybrid, we included these cases in the ESD group. The average procedure time was 145 min in the ESD group and 69 min in the EMR group.
(P < 0.0001). A macroscopically complete resection was possible in most cases (ESD group: 67/68, EMR group: 58/62; P = 0.140); however, the en bloc resection rate was 89.7% (61/67) in the ESD group in comparison to 9.7% (6/62) in the EMR group (P < 0.0001).
The rate of histologically complete resection was significantly higher in the ESD group (72.1%) than in the EMR group (9.7%; P < 0.0001). Curative resection rates were similar between both groups considering all tumors (89.7% in the ESD group vs. 83.9% in the EMR group; P = 0.324), but ESD showed a significant advantage in the curative resection of adenocarcinomas (62.5% in the ESD group vs. 14.3% in the EMR group; P = 0.033). The distribution of resection status and curative resections between the two groups is depicted on Table 2.
Postinterventional bleeding occurred in 10 cases (14.7%) after ESD and 4 cases (6.5%) after EMR (P = 0.129) and could be successfully treated endoscopically, without the need for transfusions or surgical interventions. There were no perforations in either group. Mild anal pain or discomfort was treated with standard analgesics according to the analgetic algorithm of each unit, the use of opioids was not necessary. Two patients in the EMR group presented with a stricture in the lower rectum after EMR, which was able to be successfully treated with endoscopic balloon dilation. There were no strictures in the ESD group (Table 2).
The median follow-up interval was 18 months in the ESD group and 34 months in the EMR group (P < 0.0001). There was only one recurrent adenoma in the ESD group vs. 16 cases in the EMR group (25.8%; P < 0.0001). There were no recurrent carcinomas. The recurrent adenoma after ESD was identified 12 months after the initial procedure and was treated endoscopically by EMR and avulsion with no further recurrence in the follow-up. The median interval to recurrence after EMR was 6 months (range: 2–18 months) and their further treatment required an average of 3 additional procedures: 11 patients were treated only endoscopically with repeated EMRs and argon plasma ablation, 2 patients were primarily referred for TEM, and 3 patients initially underwent additional EMRs and were finally referred for TEM.
Discussion
Epithelial lesions in the lower rectum involving the dentate line pose a particular challenge for the endoscopist, and several resection techniques have been suggested for their treatment. We have presented the findings of a bicentral, retrospective study comparing ESD and EMR for the resection of these lesions. To the best of our knowledge, this is the first study to directly compare the two methods. Our data show that ESD can achieve an en bloc resection of the tumors in most cases and is associated with a significantly lower local recurrence rate and a high curative resection rate for locally resectable, low-risk adenocarcinomas, while having a similar safety profile to that of EMR.
The anatomy of the lower rectum and the anal canal is the main reason that interventions in this area are technically difficult. The narrow anal canal with the contracted anal sphincter is followed by the abrupt widening of the rectal ampulla, forming an almost 90° angle. This geometry restricts the view and maneuverability of the endoscope, and some parts of the anorectal junction can only be reached in the retroflex position, which often restricts the function of endoscopic instruments [12]. The presence of the hemorrhoidal veins also increases the risk of intraprocedural and postprocedural bleedings and the complexity of the resection [13]. The direct drainage of these veins to the systemic circulation may also increase the risk of periprocedural bacteremia [3, 8]. Apart from that, the sensory nerve supply of the anal canal is somatic, making procedures in this area painful and thus requiring periprocedural and postprocedural analgesia [3]. Additionally, lesions on the dentate line have been associated with increased risk of submucosal fibrosis, restricting the lifting and visualization of the submucosal plane [14].
EMR is the most commonly used endoscopic resection technique for large colorectal lesions and has been associated with high technical success rates and an extremely favorable safety profile [15]. However, the restricted view and maneuverability of the endoscope in the lower rectum increases the difficulty of this technique even in experienced hands [3]. In a forward view, the almost 90° angle of the rectal wall at the anorectal junction requires an extreme angulation of the endoscope to enable the snare to be pressed against the tissue. The retroflex position offers a better visualization, but the tip of the endoscope is perpendicular to the wall of the lower rectum, which also hampers the positioning of the snare parallel to the lesion. The combination of these factors makes the precise placement of the snare more difficult than in other areas of the colorectum, thus increasing the risk of incomplete resections and injuries of the hemorrhoidal veins. Intraprocedural bleedings from the hemorrhoidal plexus are rarely clinically relevant, but they can quickly reduce the endoscopic view, thus further increasing the risk of incomplete resection. The precision of ESD helps overcome these problems, since the resection margins are carefully marked and followed during the epithelial incision. The reduced overview of the lesion, which is extremely problematic during EMR, is not a restricting factor for ESD because of the close proximity of the endoscope to the tissue required. The initial incision in the anal canal is kept shallow so as not to affect the underlying hemorrhoidal veins, which can then be carefully dissected, coagulated, and transected, thus effectively reducing the risk of intraprocedural bleeding [16]. After the establishment of an initial pocket into the submucosal plane, it is also easier to maintain a stable position of the endoscope and achieve adequate exposure of the submucosal tissue. These technical aspects lead to the increased en bloc and compete resection rates depicted in our data, which are also in accordance with the current literature [12, 17].
Before ESD became popular, TEM was commonly used as an alternative to EMR for the treatment of epithelial lesions in the lower rectum, especially in the suspicion of malignancy. This technique allows for a minimally invasive and precise resection of rectal lesions with the use of a 4cm wide rectoscope and rigid instruments and has been associated with complete resection rates of 83–87% and low recurrence rates [18,19,20,21]. Although mucosectomy and hybrid TEM-ESD have been described, most authors advocate for full-thickness resections when performing TEM [22,23,24,25]. However, TEM is technically challenging in the lower rectum and especially in the anal canal because of the instability of the rectoscope and must often be combined with transanal excision, which is known to increase the risk of incomplete resections [26,27,28]. Additionally, full-thickness resection is an overtreatment since a submucosal dissection is enough for the complete resection of all benign and early malignant lesions without deep submucosal invasion. On the contrary, full-thickness resection has been associated with increased scarring in the mesorectum, which can compromise the dissection plane and the outcomes of completion surgery in case of occult high-risk carcinomas [29, 30]. Finally, the insertion of the TEM rectoscope usually requires muscle relaxation and therefore TEM is mostly performed under general anesthesia [26, 31]. The introduction of ESD offered a new method with all the advantages of TEM regarding complete resections and low recurrence rates, while offering better access to difficult localizations like the anal canal, leaving the mesorectum intact and being performed in the endoscopy suite under sedation, thus leading to ESD gradually replacing TEM for most types of lesions in many centers.
The main advantage of ESD, as demonstrated by our findings, is the significantly lower local recurrence rate in comparison to EMR. Although no other study to our knowledge has directly compared these two techniques for lesions involving the dentate line, the single-arm retrospective studies that are available have shown similar recurrence rates to ours for both techniques, thus confirming our findings [2, 3, 9, 17]. As previously mentioned, ESD has an intrinsically higher en bloc resection rate, which is directly associated with a lower recurrence rate, in all parts of the gastrointestinal tract, but this effect is further enhanced in the lower rectum [32]. Additionally, the en bloc resection rate and recurrence rate of ESD are not directly affected by the size of the lesion, as in the case of EMR, thus further highlighting the advantages of ESD for the treatment of large tumors [2, 12, 33]. New developments in EMR, and particularly the addition of thermal ablation of the resection margins, have significantly reduced its recurrence rate, which nevertheless remains at 16% for lesions in the anorectal junction [15]. It must be pointed out that most recurrencies can be treated endoscopically, but this requires the patient’s commitment to an intensive follow-up program in order to detect the recurrence in time [15]. Additionally, the technical challenges of the anorectal junction increase even more in the presence of fibrotic tissue and the absence of lifting usually found in the site of the previous resection. Similar to previous studies, our data show that most of the patients with recurrent adenomas after EMR required multiple further endoscopic procedures and often transanal surgery to effectively treat these lesions, thus increasing the overall treatment costs and reducing patient satisfaction [2].
A subgroup of patients that will particularly benefit from ESD are those with low-risk early rectal cancer, since the resection can be curative and offers a pristine specimen, allowing for the accurate staging and evaluation of the resection status [4, 34, 35]. Epithelial lesions involving the dentate line are reported to have an increased incidence of malignancy with submucosal invasion, which highlights the importance of en bloc and complete resection of those lesions [36]. In our study, almost all low-risk T1 tumors were able to be completely resected, thus sparing the patient a major, amputating surgical procedure with high morbidity and the need for a permanent ostomy. Even in case of a lateral positive margin, careful marking of the specimen can point out the exact area of the resection defect with potential residual tumor, thus offering the possibility of a further endoscopic resection, provided that the histological tumor characteristics are favorable [35]. This is usually not possible after pmEMR, since the quality of the fragmented resection specimen is insufficient for obtaining an adequate estimation of tumor infiltration or resection status [4].
The main arguments raised against ESD are the long procedure times, the technical difficulties, and the high complication rates [3]. Similar to previous reports, our results revealed that ESD in the lower rectum required double the procedure time for lesions of the same size [7, 37]. However, it should be noted that our cohort included the entire ESD learning curve of both endoscopists primarily performing the procedure, and studies have shown that accumulating experience not only improves the outcomes but also significantly reduces procedure time [5, 38, 39]. There is no doubt that ESD procedures in difficult anatomical areas such as the anorectal junction should be performed by experienced endoscopists, but the same applies for EMR, since overcoming the technical challenges described above requires considerable experience [3]. As for periinterventional morbidity, we found no difference between ESD and EMR in our study. The much-feared colon perforation is clinically less relevant in the lower rectum, since it is supported by the mesorectum and peritoneal entry is nearly impossible [7, 9]. The risk of postprocedural bleeding is not negligible, and various studies have shown that it is higher for rectal lesions, particularly those involving the dentate line [9]. However, this is mostly associated with the anatomy of the lower rectum and not with the procedure itself, which explains the similar bleeding rates found in both groups in our study. The same applies for strictures in the anal canal and the lower rectum.
The main strength of our study is the direct comparison of ESD with EMR, with both techniques being performed in two high-volume centers by the same experienced endoscopists, thus contributing to the homogeneity of the groups regarding indication, definitions, and experience of the contributing teams. The multicentric design and the large number of consequent cases included also contribute to the validity of the results. The main limitation of this study is its retrospective nature. The retrospective study design also explains the discrepancy in the median follow-up periods between the two groups, since ESD was primarily performed in the later part of the study period. However, the median follow-up period of the ESD group, although shorter, is still long enough and exceeds the expected interval for recurrence, as demonstrated in the EMR group. Therefore we believe, that the influence of this discrepancy on our findings is minimal. Nevertheless, a prospective, randomized trial comparing these two techniques is required to verify our conclusions.
Based on the findings of our study we believe that ESD is superior to EMR for the treatment of epithelial lesions in the lower rectum that involve the dentate line, especially regarding local recurrence rates and the possibility of curative resection of low-risk early rectal cancer. In experienced hands, ESD is an effective procedure with a safety profile comparable to that of EMR. The long procedure times, the costs involved, and the technical challenges of ESD certainly do not justify its application for all colorectal lesions, and careful patient selection is required in order to maximize its advantages [40]. On the other hand, our data show that patients with lesions located in the anorectal junction are a subgroup who can profit from ESD and therefore we believe that it should be considered as the treatment of choice for those lesions.
References
Schmiegel W, Buchberger B, Follmann M, Graeven U, Heinemann V, Langer T, Nothacker M, Porschen R, Rödel C, Rösch T, Schmitt W, Wesselmann S, Pox C (2017) S3-Leitlinie—Kolorektales Karzinom. Z Gastroenterol 55:1344–1498. https://doi.org/10.1055/S-0043-121106
Liu S, Li Y, Yang H, Li A, Han Z, Wang X, Xiong F, Xu W, Zhou D (2016) Retroflexion-assisted endoscopic mucosal resection: a useful and safe method for removal of low rectal laterally spreading tumors. Surg Endosc 30:139–146. https://doi.org/10.1007/S00464-015-4173-2
Holt BA, Bassan MS, Sexton A, Williams SJ, Bourke MJ (2014) Advanced mucosal neoplasia of the anorectal junction: endoscopic resection technique and outcomes (with videos). Gastrointest Endosc 79:119–126. https://doi.org/10.1016/J.GIE.2013.07.003
Asayama N, Oka S, Tanaka S, Hayashi N, Arihiro K, Chayama K (2015) Endoscopic submucosal dissection as total excisional biopsy for clinical T1 colorectal carcinoma. Digestion 91:64–69
Saito Y, Sakamoto T, Fukunaga S, Nakajima T, Kuriyama S, Matsuda T (2009) Endoscopic submucosal dissection (ESD) for colorectal tumors. Dig Endosc. https://doi.org/10.1111/j.1443-1661.2009.00870.x
Lee EJ, Lee JB, Lee SH, Kim DS, Lee DH, Lee DS, Youk EG (2013) Endoscopic submucosal dissection for colorectal tumors—1,000 colorectal ESD cases: one specialized institute’s experiences. Surg Endosc 27:31–39. https://doi.org/10.1007/s00464-012-2403-4
Probst A, Ebigbo A, Märkl B, Schaller T, Anthuber M, Fleischmann C, Messmann H (2017) Endoscopic submucosal dissection for early rectal neoplasia: Experience from a European center. Endoscopy 49:222–232. https://doi.org/10.1055/s-0042-118449
Imai K, Hotta K, Yamaguchi Y, Shinohara T, Ooka S, Shinoki K, Kakushima N, Tanaka M, Takizawa K, Matsubayashi H, Oishi T, Ono H (2015) Safety and efficacy of endoscopic submucosal dissection of rectal tumors extending to the dentate line. Endoscopy 47:529–532. https://doi.org/10.1055/S-0034-1391078
Probst A, Ebigbo A, Märkl B, Ting S, Schaller T, Anthuber M, Fleischmann C, Messmann H (2018) Endoscopic submucosal dissection for rectal neoplasia extending to the dentate line: European experience. Endosc Int Open 6:E1355–E1362. https://doi.org/10.1055/A-0749-8735
Pérez-Cuadrado-Robles E, Chupin A, Perrod G, Severyns T, Cellier C, Rahmi G (2022) Endoscopic submucosal dissection in tumors extending to the dentate line compared to proximal rectal tumors: a systematic review with meta-analysis. Eur J Gastroenterol Hepatol 34:121–127. https://doi.org/10.1097/MEG.0000000000001998
Komeda Y, Kashida H, Sakurai T, Asakuma Y, Tribonias G, Nagai T, Kono M, Minaga K, Takenaka M, Arizumi T, Hagiwara S, Matsui S, Watanabe T, Nishida N, Chikugo T, Chiba Y, Kudo M (2017) Magnifying narrow band imaging (NBI) for the diagnosis of localized colorectal lesions using the Japan NBI Expert Team (JNET) classification. Oncology 93:49–54. https://doi.org/10.1159/000481230
Guo HM, Ling TS, Wang L, Lv Y, Zhang XQ, Yang T, Xu GF, Sun Q, Nie L, Zou XP (2019) Clinical outcomes of endoscopic submucosal dissection for laterally spreading tumors involving the dentate line. J Dig Dis 20:83–88. https://doi.org/10.1111/1751-2980.12701
Tanaka S, Toyonaga T, Morita Y, Hoshi N, Ishida T, Ohara Y, Yoshizaki T, Kawara F, Umegaki E, Azuma T (2016) Feasibility and safety of endoscopic submucosal dissection for lower rectal tumors with hemorrhoids. World J Gastroenterol 22:6268–6275. https://doi.org/10.3748/WJG.V22.I27.6268
Tanaka S, Oka S, Chayama K (2008) Colorectal endoscopic submucosal dissection: present status and future perspective, including its differentiation from endoscopic mucosal resection. J Gastroenterol 43:641–651
Shahidi N, Sidhu M, Vosko S, Van Hattem WA, Bar-Yishay I, Schoeman S, Tate DJ, Holt B, Hourigan LF, Lee EYT, Burgess NG, Bourke MJ (2020) Endoscopic mucosal resection is effective for laterally spreading lesions at the anorectal junction. Gut 69:673–680. https://doi.org/10.1136/GUTJNL-2019-319785
Nakadoi K, Tanaka S, Hayashi N, Ozawa SI, Terasaki M, Takata S, Kanao H, Oka S, Chayama K (2012) Clinical outcomes of endoscopic submucosal dissection for rectal tumor close to the dentate line. Gastrointest Endosc 76:444–450. https://doi.org/10.1016/J.GIE.2012.04.004
Tamaru Y, Oka S, Tanaka S, Hiraga Y, Kunihiro M, Nagata S, Furudoi A, Ninomiya Y, Asayama N, Shigita K, Nishiyama S, Hayashi N, Chayama K (2016) Endoscopic submucosal dissection for anorectal tumor with hemorrhoids close to the dentate line: a multicenter study of Hiroshima GI Endoscopy Study Group. Surg Endosc 30:4425–4431. https://doi.org/10.1007/S00464-016-4761-9
Buess G, Theiss R, Gunther M, Hutterer F, Pichlmaier H (1985) Endoscopic surgery in the rectum. Endoscopy 17:31–35. https://doi.org/10.1055/s-2007-1018451
Serra-Aracil X, Ruiz-Edo N, Casalots-Casado A, Mora-López L, Pallisera-Lloveras A, Serra-Pla S, Puig-Diví V, Navarro-Soto S (2019) Importance of resection margins in the treatment of rectal adenomas by transanal endoscopic surgery. J Gastrointest Surg 23:1874–1883. https://doi.org/10.1007/s11605-018-3980-x
De Graaf EJR, Doornebosch PG, Tetteroo GWM, Geldof H, Hop WCJ (2009) Transanal endoscopic microsurgery is feasible for adenomas throughout the entire rectum: a prospective study. Dis Colon Rectum 52:1107–1113. https://doi.org/10.1007/DCR.0b013e3181a0d06d
Bretagnol F, Merrie A, George B, Warren BF, Mortensen NJ (2007) Local excision of rectal tumours by transanal endoscopic microsurgery. Br J Surg 94:627–633. https://doi.org/10.1002/bjs.5678
Serra-Aracil X, Caro-Tarrago A, Mora-López L, Casalots A, Rebasa P, Navarro-Soto S (2014) Transanal endoscopic surgery with total wall excision is required with rectal adenomas due to the high frequency of adenocarcinoma. Dis Colon Rectum 57:823–829
Morino M, Arezzo A, Allaix ME (2013) Transanal endoscopic microsurgery. Tech Coloproctol. https://doi.org/10.1007/s10151-012-0936-0
Kouladouros K, Baral J (2022) Transanal endoscopic microsurgical submucosal dissection (TEM-ESD) for rectal adenomas: a retrospective cohort study of 145 consecutive cases. Langenbecks Arch Surg. https://doi.org/10.1007/s00423-022-02562-0
Kouladouros K, Baral J (2021) Transanal endoscopic microsurgical submucosal dissection (TEM-ESD): a novel approach to the local treatment of early rectal cancer. Surg Oncol 39:101662. https://doi.org/10.1016/j.suronc.2021.101662
Saclarides TJ (2007) TEM/local excision: indications, techniques, outcomes, and the future. J Surg Oncol 96:644–650
Lev-Chelouche D, Margel D, Goldman G, Rabau MJ (2000) Transanal endoscopic microsurgery: experience with 75 rectal neoplasms. Dis Colon Rectum 43:662–668. https://doi.org/10.1007/bf02235583
Madbouly KM, Remzi FH, Erkek BA, Senagore AJ, Baeslach CM, Khandwala F, Fazio VW, Lavery IC (2005) Recurrence after transanal excision of T1 rectal cancer: Should we be concerned? Dis Colon Rectum 48:711–721. https://doi.org/10.1007/s10350-004-0666-0
Hompes R, McDonald R, Buskens C, Lindsey I, Armitage N, Hill J, Scott A, Mortensen NJ, Cunningham C, Association of Coloproctology of Great Britain and Ireland Transanal Endoscopic Microsurgery Collaboration (2013) Completion surgery following transanal endoscopic microsurgery: assessment of quality and short- and long-term outcome. Colorectal Dis 15:e576–e581. https://doi.org/10.1111/codi.12381
Morino M, Allaix ME, Arolfo S, Arezzo A (2013) Previous transanal endoscopic microsurgery for rectal cancer represents a risk factor for an increased abdominoperineal resection rate. Surg Endosc 27:3315–3321. https://doi.org/10.1007/s00464-013-2911-x
Dafnis G, Påhlman L, Raab Y, Gustafsson UM, Graf W (2004) Transanal endoscopic microsurgery: clinical and functional results. Colorectal Dis 6:336–342. https://doi.org/10.1111/j.1463-1318.2004.00629.x
De Ceglie A, Hassan C, Mangiavillano B, Matsuda T, Saito Y, Ridola L, Bhandari P, Boeri F, Conio M (2016) Endoscopic mucosal resection and endoscopic submucosal dissection for colorectal lesions: a systematic review. Crit Rev Oncol Hematol 104:138–155
Hayashi Y, Shinozaki S, Sunada K, Sato H, Miura Y, Ino Y, Horie H, Fukushima N, Lefor AK, Yamamoto H (2016) Efficacy and safety of endoscopic submucosal dissection for superficial colorectal tumors more than 50 mm in diameter. Gastrointest Endosc 83:602–607. https://doi.org/10.1016/j.gie.2015.08.037
Suh JP, Youk EG, Lee EJ, Lee JB, Lee IT, Lee DS, Kim MJ, Lee SH (2013) Endoscopic submucosal dissection for nonpedunculated submucosal invasive colorectal cancer: is it feasible? Eur J Gastroenterol Hepatol 25:1051–1059. https://doi.org/10.1097/MEG.0b013e328361dd39
Pimentel-Nunes P, Libânio D, Bastiaansen BAJ, Bhandari P, Bisschops R, Bourke MJ, Esposito G, Lemmers A, Maselli R, Messmann H, Pech O, Pioche M, Vieth M, Weusten BLAM, Van Hooft JE, Deprez PH, Dinis-Ribeiro M (2022) Endoscopic submucosal dissection for superficial gastrointestinal lesions: European Society of Gastrointestinal Endoscopy (ESGE) Guideline—Update 2022. Endoscopy 54:591–622. https://doi.org/10.1055/A-1811-7025
Andrisani G, Fukuchi T, Hassan C, Hamanaka J, Antonelli G, Costamagna G, Di Matteo FM, Hirasawa K (2020) Rectal neoplasia extending to the dentate line: clinical outcomes of endoscopic submucosal dissection. Scand J Gastroenterol 55:1363–1368. https://doi.org/10.1080/00365521.2020.1825791
Saito Y, Fukuzawa M, Matsuda T, Fukunaga S, Sakamoto T, Uraoka T, Nakajima T, Ikehara H, Fu KI, Itoi T, Fujii T (2010) Clinical outcome of endoscopic submucosal dissection versus endoscopic mucosal resection of large colorectal tumors as determined by curative resection. Surg Endosc 24:343–352. https://doi.org/10.1007/s00464-009-0562-8
Probst A, Golger D, Anthuber M, Märkl B, Messmann H (2012) Endoscopic submucosal dissection in large sessile lesions of the rectosigmoid: learning curve in a European center. Endoscopy 44:660–667. https://doi.org/10.1055/s-0032-1309403
Matsumoto S, Mashima H (2017) The efficacy of endoscopic submucosal dissection for colorectal tumors extending to the dentate line. Int J Colorectal Dis 32:831–837. https://doi.org/10.1007/S00384-017-2775-Y
Bahin FF, Heitman SJ, Rasouli KN, Mahajan H, McLeod D, Lee EYT, Williams SJ, Bourke MJ (2018) Wide-field endoscopic mucosal resection versus endoscopic submucosal dissection for laterally spreading colorectal lesions: a cost-effectiveness analysis. Gut 67:1965–1973. https://doi.org/10.1136/GUTJNL-2017-313823
Funding
Open Access funding enabled and organized by Projekt DEAL. No internal or external funding was received for this study.
Author information
Authors and Affiliations
Contributions
Konstantinos Kouladouros designed the study, contributed to the data collection and analysis, performed the literature review, and wrote and revised the manuscript. Johanna Jakobs contributed to the data collection and analysis and the revision of the manuscript. Petros Stathopoulos, Georg Kähler, and Sebastian Belle contributed to the literature research and the preparation and revision of the manuscript. Ulrike Denzer contributed to the design of the study, the data collection and analysis, and the preparation and revision of the manuscript.
Corresponding author
Ethics declarations
Disclosures
K. Kouladouros, J. Jakobs, P. Stathopoulos, G. Kähler, S. Belle and U. Denzer have no relevant conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kouladouros, K., Jakobs, J., Stathopoulos, P. et al. Endoscopic submucosal dissection versus endoscopic mucosal resection for the treatment of rectal lesions involving the dentate line. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-10994-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-10994-6







