Abstract
Background
Sleeve gastrectomy (SG) increased in popularity after 2010 but recent data suggest it has concerning rates of gastroesophageal reflux and need for conversions. This study aims to evaluate recent trends in the utilization of bariatric procedures, associated complications, and conversions using an administrative claims database in the United States.
Methods
We included adults who had bariatric procedures from 2000 to 2020 with continuous enrollment for at least 6 months in the MarketScan Commercial Claims and Encounters database. Index bariatric procedures and subsequent revisions or conversions were identified using CPT codes. Baseline comorbidities and postoperative complications were identified with ICD-9-CM and ICD-10 codes. Cumulative incidences of complications were estimated at 30-days, 6-months, and 1-year and compared with stabilized inverse probability of treatment weighted Kaplan–Meier analysis.
Results
We identified 349,411 bariatric procedures and 5521 conversions or revisions. The sampled SG volume appeared to begin declining in 2018 while Roux-en-Y gastric bypass (RYGB) remained steady. Compared to RYGB, SG was associated with lower 1-year incidence [aHR, (95% CIs)] for 30-days readmission [0.65, (0.64–0.68)], dehydration [0.75, (0.73–0.78)], nausea or vomiting [0.70, (0.69–0.72)], dysphagia [0.55, (0.53–0.57)], and gastrointestinal hemorrhage [0.43, (0.40–0.46)]. Compared to RYGB, SG was associated with higher 1-year incidence [aHR, (95% CIs)] of esophagogastroduodenoscopy [1.13, (1.11–1.15)], heartburn [1.38, (1.28–1.49)], gastritis [4.28, (4.14–4.44)], portal vein thrombosis [3.93, (2.82–5.48)], and hernias of all types [1.36, (1.34–1.39)]. There were more conversions from SG to RYGB than re-sleeving procedures. SG had a significantly lower 1-year incidence of other non-revisional surgical interventions when compared to RYGB.
Conclusions
The overall volume of bariatric procedures within the claims database appeared to be declining over the last 10 years. The decreasing proportion of SG and the increasing proportion of RYGB suggest the specific complications of SG may be driving this trend. Clearly, RYGB should remain an important tool in the bariatric surgeon’s armamentarium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obesity is an epidemic disease that is rapidly growing, with a recent US national survey in 2018 showing the prevalence of obesity has risen from 30.5% in 1999 to 42.4% in 2018. [1] The prevalence of severe obesity has also almost doubled within that time period, from 4.7 to 9.2% [1]. Obesity and its associated medical comorbidities are estimated to have a medical cost of $170 billion annually with an economic burden of $1.72 trillion [2, 3]. Bariatric surgery remains the most effective and durable treatment option for obesity. Currently, laparoscopic sleeve gastrectomy (SG) is the most performed bariatric procedure, having surpassed laparoscopic Roux-en-Y gastric bypass (RYGB) in 2012 [4]. The overall volume of bariatric surgery increased by 60% from 2011 to 2018 with sleeve gastrectomy demonstrating a remarkable 451% growth trend [5]. However, the utilization of bariatric surgery in patients who could qualify remains low despite the significant improvement in perioperative risk reduction.
Revisional surgery had also been rising steadily since 2011, increasing more than three-fold through 2019 and representing the third most commonly performed bariatric procedure after SG and RYGB [6]. Despite the relative simplicity and low incidence of complications of SG, there has been evidence pointing at higher revision and conversion rates when compared to RYGB [7, 8]. Gastroesophageal reflux disease (GERD), insufficient weight loss, and weight regain are the most common reasons for revisions and conversions after SG. Studies have also shown that conversion from SG to RYGB carries a higher risk of serious complications when compared to primary RYGB [9]. Although the choice of primary procedure is typically dependent on patient factors and surgeon preference, it is important to recognize the risks for future revisions and to educate patients accordingly. This study aims to build on a previous retrospective review of nationwide commercial claims data by Chung et al., to evaluate recent trends in bariatric procedure utilization, and to expand upon the previous study by analyzing the associated incidence of complications, revisions, and conversions.
Methods
The study was conducted using the IBM MarketScan® Commercial Claims and Encounters database. We included adult patients (18 years or older) who underwent bariatric procedures from 2000 to 2020 and had a continuous enrollment for at least 180 days before the index bariatric procedure. We identified the following bariatric procedures using CPT codes: CPT codes 43,644, 43,645 (laparoscopic RYGB), 43,846, 43,847 (open RYGB), 43,775 (laparoscopic SG), 43,770 (laparoscopic adjustable gastric banding (AGB)), 43,842 (vertical banded gastroplasty (VBG)), 43,845 (biliopancreatic diversion with duodenal switch (BPD/DS)). The baseline characteristics of the study cohort in the 6-months before the index procedure were identified using ICD-9-CM and ICD-10 codes. We used the first CPT code for a bariatric operation as the index procedure and recorded subsequent incidence of complications at 30-days, 6-months, and 1-year using ICD-9-CM, ICD-10, and CPT codes from administrative claims, where applicable. The full list of complications and codes used is shown in Appendix 1. Subsequent CPT codes after the index procedure were used to identify revisions and conversions. We also separately identified first and second revisions and/or conversions based on subsequent related CPT codes after the index procedure. Other non-revisional surgical interventions such as internal hernias, ulcer-related procedures, and unlisted procedures were recorded after 6-months and 1-year.
Statistical analysis
The baseline characteristics were stratified by the type of procedure. Continuous variables were reported as either mean ± standard deviation (SD) if the data were normally distributed or median with interquartile ranges (IQR) if the data were not normally distributed. Categorical variables were presented as frequency/counts and percentage. The Charlson comorbidity index (CCI) was calculated using the method described by Deyo et al. [10] We presented the trends in bariatric procedures on a quarterly basis from 2000 to 2020, describing the procedure types by both percentages of all procedure types and also as volume of procedure performed.
We used inverse probability of treatment weights (IPT) to control for confounding. We estimated cumulative incidence of complications of SG, RYGB and BPD/DS at 30-days, 6-months, and 1-year postoperatively using weighted Kaplan–Meier analyses. We estimated the weights based on the inverse of predicted probability (propensity scores) of receiving SG vs. RYGB or BPD/DS vs. RYGB using two separate logistic regression models. These propensity score models included patient age, sex, all comorbidities in CCI (excluding human immunodeficiency virus), location of the procedure (inpatient or outpatient), and the year of the index procedure. The IPT weights were stabilized using the marginal probability of receiving SG vs. RYGB or BPD/DS vs. RYGB. We calculated the adjusted Hazard ratio (aHR) comparing SG vs. RYGB and BPD/DS vs. RYGB on the 1-year risk of complications from 2010 to 2020 with weighted Kaplan–Meier analyses and 95% confidence intervals (CIs) using robust-variance estimators. Similarly, we calculated weighted cumulative incidence of procedure-specific revisions between SG and RYGB at 6-months and 1-year using weighted survival models and calculated aHR, 95% CIs (using robust-variance estimators). All analyses were performed using SAS 9.4 (SAS Inc., Cary, NC).
Results
We identified 343,727 unique individuals who underwent one or more bariatric procedures between 2000 and 2020 and met our inclusion criteria. The baseline characteristics were stratified by procedure type and described in Table 1. The mean age was 43.5 ± 10.6 years old, with the cohort consisting of 78.9% female patients and 21.1% male patients. Laparoscopic RYGB and BPD/DS patients had a higher prevalence of diabetes mellitus at baseline when compared to SG (37.1% and 37.5% vs. 28.6%, respectively). The median length of stay (LOS) was higher in open and laparoscopic RYGB when compared to SG (3 days (IQR: 2–4) and 2 days (1–2) vs. 1 day (1–2)). Table 1 details baseline characteristics of patients by type of index procedure.
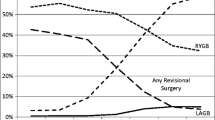
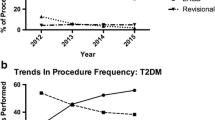
The trend of bariatric surgery procedures performed between 2000 and 2020 as a percentage from the total sample cohort is shown in Fig. 1. Open RYGB, AGB, and VBG all dramatically reduced in overall utilization over the past two decades. SG increased in utilization rapidly since 2010 and appeared to have plateaued around 2018 with a small decline thereafter (peak of 75.9% in 2018 to 69.2% in 2020, in percentage of total sample cohort), while laparoscopic RYGB appeared to increase around the same time (22.1% in 2018 to 28.6% in 2020, as a percentage of total sample cohort). Figure 2 demonstrates a sub-analysis of the actual quarterly and annual volume from our cohort for SG and Laparoscopic RYGB from 2004 to 2020. When examining the trend of bariatric surgery in terms of actual volume from the total sample cohort, however, the laparoscopic RYGB volume appeared to hold steady after 2015 while SG, again, appeared to decline beginning in 2018.
Trend of bariatric surgery 2000–2020, in percentage of total sample cohort. Overall trend of open roux-en-y gastric bypass (RYGB), laparoscopic RYGB, sleeve gastrectomy (SG), laparoscopic adjustable gastric banding (AGD), vertical banded gastroplasty (VBG), and biliopancreatic diversion with duodenal switch (BPD/DS) from 2000 to 2020 in terms of percentage of total sample cohort
The risks of complications between SG and laparoscopic RYGB, and between laparoscopic RYGB and BPD/DS, at 1-year postoperatively are reported in Tables 2 and 3, respectively. Compared to laparoscopic RYGB, SG was associated with lower 1-year incidence for readmission, emergency room visit, wound dehiscence, dehydration, weight/feeding disorder, malabsorption, anemia, vitamin deficiency, nausea or vomiting, dysphagia, other digestive symptoms, pneumonia, sepsis, urinary complications, gastrointestinal ulcers, obstruction, hemorrhage/hematoma, gallbladder disorders, and acute renal failure. Conversely, compared to laparoscopic RYGB, SG was associated with higher 1-year incidence of esophagogastroduodenoscopy (EGD), heartburn, gastritis, portal vein thrombosis, and hernias of all types. Compared to laparoscopic RYGB, BPD/DS was associated with higher incidence of readmission, heartburn, and gastritis. Conversely, BPD/DS was associated with a lower incidence of EGD and gastrointestinal ulcer when compared to laparoscopic RYGB.
Table 4 shows the comparison of revision volumes for the sample cohort over 2000–2020. There were a total of 5370 patients with revisions or conversions captured within our cohort with 151 patients undergoing a second revision or conversion. Overall, the most common revisions were ABG to SG (2220), ABG to RYGB (1092), SG to RYGB (819), and AGB revisions (399). SG was compared with laparoscopic RYGB in Table 5 in terms of incidence of general surgical interventions at 6-months and 1-year. SG had a significantly lower 1-year incidence of need for surgical intervention when compared to RYGB. The 1-year incidence of leak, perforation, or ulcer-related complication was not significantly different between SG and RYGB.
Discussion
This study evaluated the trends of bariatric surgery utilization, postoperative complications, conversions and revisions in the last 20 years using a national commercial claims database. We compared the incidence of postoperative complications between SG and laparoscopic RYGB as well as between laparoscopic RYGB and BPD/DS. Compared to laparoscopic RYGB, SG was associated with lower incidences of most postoperative complications in general, but higher incidences of heartburn, gastritis, portal vein thrombosis, hernias of all types, and need for EGD. These findings are consistent with the most recent studies where SG is often found to have a comparable or lower incidence of postoperative complication than RYGB but is limited by an increased incidence of GERD, worsening of GERD symptoms, or esophagitis [11,12,13]. One of the hypotheses for GERD after SG is an increase in intragastric pressure as well as gastroesophageal pressure gradient, resulting in increased acid exposure and number of reflux episodes [14]. The higher incidences of EGD in SG patients 1-year postoperatively could potentially be secondary to the need for evaluation of gastrointestinal symptoms from unrecognized esophageal dysmotility, GERD, postoperative nausea and vomiting (PONV), or stenosis of the sleeve. A recent study by Zhu et al. showed that, compared to RYGB, SG is associated with a higher incidence of PONV (77.4% versus 21.5%), especially in patients with preoperative reflux symptoms [15]. These symptoms after SG can often be signs of developing or worsening GERD and should be treated and monitored accordingly. Our study showed a higher 1-year incidence of hernias of all types in SG when compared to laparoscopic RYGB. This finding could potentially be due to increased attention to the hiatus during SG leading to increased diagnosis and aggressive treatment of hiatal hernias. The need for gastric specimen extraction in SG also could lead to potential incisional hernias depending on extraction site and port closure methods. The risk of incisional hernia after sleeve gastrectomy was found by Ahlqvist et al. to be as high as 21.5% when using a Hasson technique and continuous closure of the port site [16]. Unfortunately, we did not differentiate between various hernia types in our study. Further study and sub-analysis are planned to investigate the incidence of hiatal hernias and incisional hernias in the SG and RYGB populations.
When compared to laparoscopic RYGB, we found BPD/DS was associated with higher 1-year incidences of postoperative complications in general but lower incidences of EGD and gastrointestinal ulcer. This finding is consistent with other studies comparing RYGB to BPD/DS, where BPD/DS is associated with a higher incidence of early 30-days complications (15.3% vs. 8.1%) and long-term adverse events (2.7 vs. 0.9 events per patient) up to 15 years post-operatively [17, 18]. Our reported BPD/DS results based on the 43,845 CPT code are limited as it is likely a combination of laparoscopic and open approaches. Open BPD/DS, though rarely performed, is often associated with higher incidence of postoperative adverse events and longer LOS. Yet, studies that isolated and compared the laparoscopic approaches of RYGB and BPD/DS also showed higher incidence of adverse events for BPD/DS [19, 20]. Although not specifically identified in our current study due to a lack of a discrete CPT code, single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) is a newer procedure aimed at reducing the operative and perioperative complications of BPD/DS while preserving its remarkable weight loss capabilities and effect on comorbidities. Current studies are mixed regarding if SADI-S is comparable in terms of perioperative complications to RYGB and more long-term studies are required to determine its role among the current bariatric armamentarium [21,22,23].
Among the revisions and conversions, the highest volumes of conversions were from AGB to SG and AGB to RYGB. The third most common conversion within our cohort was SG to RYGB. This volume reflected the conversions over the span of 2000–2020, which had a higher number of AGB conversions when compared to a more recent Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) retrospective analysis of conversions performed in 2020 [24].This MBSAQIP study found that the most converted index operations were SG (49.3%) and AGB (45.9%), with the most frequent conversion being SG to RYGB (40.3%) and AGB to SG (27.3%) [24]. This change in proportions of conversions when compared to our study is likely due to the tremendous decline in AGB, which now comprises less than 1% of bariatric procedures. With SG being the most common bariatric procedure in more recent years, it is no surprise that SG to RYGB has become the most common conversion. While our study could not specifically examine the indications for revisions or conversions, most studies identify GERD as the main reason for SG conversions and report a 2–6% rate of SG to RYGB conversion due to severe reflux alone [24, 25]. Inadequate weight loss or weight regain are also indications for SG to RYGB conversions but may potentially be underrepresented given the frequent lack of insurance coverage for these indications. In our study, the proportion of SG to RYGB conversion was only 0.6% out of the total number of SG captured and the overall volume of conversions and revisions were lower than most database studies [24, 26]. We suspect this was due to the limitation of using CPT codes and a private claims database, where change in employer and insurance will lead to a loss of follow up and inability to capture subsequent revisions and conversions due to lack of continuous enrollment.
When comparing 6-months and 1-year surgical interventions (including unlisted procedures, omental patch, internal hernia, and bowel obstructions), SG had a significantly lower incidence of need for surgical intervention by 1-year when compared to RYGB, consistent with prior literature [27]. However, this increased risk for RYGB was not seen when comparing the rates of intervention for leak, perforation, or ulcer. This is contrary to most studies but may be due to only having up to 1 year of follow up [28]. Another potential reason may be that the study period covers the popularization of SG and there may be higher leak rates during the learning curve that offset the leak rates in more recent times [29]. Our results were also limited due to the use of CPT codes as there may be other procedure codes used for leaks that were not reported or captured accurately. In our study, RYGB was associated with a higher 1-year incidence of lysis of adhesions, reduction of volvulus, and closure of internal hernia or mesenteric defect. This was consistent with other reports and is an inherent risk of intestinal reconstruction [30]. Overall, the postoperative complications from this MarketScan database study appear consistent with current literature but were limited by intrinsic limitations of utilizing administrative claims databases.
Laparoscopic SG continued to be the most commonly performed bariatric procedure, but the observed volume in our cohort appeared to decline in 2018. This decline in volume, also seen in the rest of the cohorts for other commonly performed bariatric procedures, was in contrast to data from other national samples such as the MBSAQIP and Medicare and Medicaid databases, where an increase in overall volume was demonstrated until the reduction in 2020 secondary to the COVID-19 pandemic [6, 31]. The decline in volume within the MarketScan database may potentially be due to the limitation that the sampled volume is based on private employer insurance, where changes in bariatric surgery coverage, preoperative requirements, and employment can affect access to care [32, 33]. Interestingly, the decline in RYGB volume appeared less precipitous than the decline in SG. This resulted in an overall increase in proportion of RYGB performed and a decrease in proportion of SG performed since around 2018, although both volumes were decreasing. This increase in proportion of RYGB in recent years was also seen in the most recent MBSAQIP analysis, where RYGB increased to 22.2% from 17% and SG decreased to 57.4% from 61.4% from 2018 to 2022 [34]. This rebound of RYGB utilization in recent years may signify the growing recognition of the limitations of SG. Currently, there is no established consensus on the choice of SG vs. RYGB other than in patients with severe GERD and patients with type-II diabetes mellitus despite numerous randomized trials comparing the two and a recent expert modified Delphi consensus [35]. Although both procedures produce excellent weight loss and comorbidity reduction results, the choice of the procedure ultimately is dependent on patient characteristics, patient preference, and surgeon experience as the two procedures have differing profiles of benefits and risks associated with them.
Our study was limited due to its retrospective nature and its restriction to private, employer-sponsored insurance claims. First, the procedures and complications were abstracted using CPT and ICD codes (ICD-9 was used until 2015, then followed by ICD-10), which rely on healthcare providers’ and coders’ accurate input and may have led to misclassification of some of the complications. Second, patients who switch insurance during the study period are lost to follow up within the database, likely contributing to the low incidence of revisions captured in our study. Third, the database does not include information on death, so we could not account for death as a competing risk in our analysis. Future studies using the MBSAQIP, the Michigan Bariatric Surgery Collaborative, or other statewide databases may be helpful in evaluating whether payor types affect the rate of revisions. Despite these limitations, this study is one of the largest longitudinal studies on the trends of bariatric surgery based on private claims data. The MarketScan claims database was chosen specifically for its ability to track individuals longitudinally regardless of which healthcare system to which they present with complications or revisions. This capability provides a unique perspective over traditional databases where complications or revisions can be missed if patients present to a different healthcare system. This study also demonstrated validity of the private claims database with results consistent with other published retrospective and prospective studies. We plan to utilize the strengths of the private claims database to investigate the prescription patterns and trends of Glucagon-like peptide-1 agonist medications as well as use of proton pump inhibitors in the preoperative and postoperative settings in the cohort identified in this study.
In conclusion, this IBM MarketScan Commercial database study from 2000 to 2020 demonstrated a reduction in SG utilization starting from 2018 with a corresponding increase in proportion of RYGB performed, which matches well with recent MBSAQIP data. Although SG remains the most frequently utilized bariatric procedure given its low risks for complications, the incidence of GERD, weight regain, and potential need for conversion may limit its use in certain populations. RYGB continues to be one of the gold standard bariatric procedures and should remain part of the modern bariatric surgeon’s armamentarium.
Data availability
Source data: Copyright © 2021 IBM Watson Health. All Rights Reserved. IBM Watson Health and MarketScan are trademarks of IBM Corporation in the United States, other countries or both.
References
Hales CM, Carroll MD, Fryar CD, Ogden CL (2020) Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief 360:1–8
Tsai AG, Williamson DF, Glick HA (2011) Direct medical cost of overweight and obesity in the USA: a quantitative systematic review. Obes Rev 12(1):50–61. https://doi.org/10.1111/j.1467-789X.2009.00708.x
Waters H, Graf M (2018) America’s obesity crisis: the health and economic costs of excess weight [monograph on the internet]. Milken Institute, Santa Monica
Chung AY, Strassle PD, Schlottmann F, Patti MG, Duke MC, Farrell TM (2019) Trends in utilization and relative complication rates of bariatric procedures. J Gastrointest Surg 23(7):1362–1372. https://doi.org/10.1007/s11605-018-3951-2
English WJ, DeMaria EJ, Hutter MM, Kothari SN, Mattar SG, Brethauer SA, Morton JM (2020) American society for metabolic and bariatric surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis 16(4):457–463. https://doi.org/10.1016/j.soard.2019.12.022
Clapp B, Ponce J, DeMaria E, Ghanem O, Hutter M, Kothari S, LaMasters T, Kurian M, English W (2022) American society for metabolic and bariatric surgery 2020 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis 18(9):1134–1140. https://doi.org/10.1016/j.soard.2022.06.284
Felsenreich DM, Artemiou E, Steinlechner K, Vock N, Jedamzik J, Eichelter J, Gensthaler L, Bichler C, Sperker C, Beckerhinn P, Kristo I, Langer FB, Prager G (2021) Fifteen years after sleeve gastrectomy: weight loss, remission of associated medical problems, quality of life, and conversions to Roux-en-Y gastric bypass-long-term follow-up in a multicenter study. Obes Surg 31(8):3453–3461. https://doi.org/10.1007/s11695-021-05475-x
Altieri MS, Yang J, Nie L, Blackstone R, Spaniolas K, Pryor A (2018) Rate of revisions or conversion after bariatric surgery over 10 years in the state of New York. Surg Obes Relat Dis 14(4):500–507. https://doi.org/10.1016/j.soard.2017.12.019
Dang JT, Vaughan T, Mocanu V, Mubashir H, Barajas-Gamboa JS, Codina RC, Rodriguez J, Karmali S, Kroh M (2023) Conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: indications, prevalence, and safety. Obes Surg 33(5):1486–1493. https://doi.org/10.1007/s11695-023-06546-x
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Tai CM, Huang CK, Lee YC, Chang CY, Lee CT, Lin JT (2013) Increase in gastroesophageal reflux disease symptoms and erosive esophagitis 1 year after laparoscopic sleeve gastrectomy among obese adults. Surg Endosc 27(4):1260–1266. https://doi.org/10.1007/s00464-012-2593-9
Peterli R, Wölnerhanssen BK, Peters T, Vetter D, Kröll D, Borbély Y, Schultes B, Beglinger C, Drewe J, Schiesser M, Nett P, Bueter M (2018) Effect of laparoscopic sleeve gastrectomy vs. laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. JAMA 319(3):255–265. https://doi.org/10.1001/jama.2017.20897
Salminen P, Grönroos S, Helmiö M, Hurme S, Juuti A, Juusela R, Peromaa-Haavisto P, Leivonen M, Nuutila P, Ovaska J (2022) Effect of laparoscopic sleeve gastrectomy vs. Roux-en-Y gastric bypass on weight loss, comorbidities, and reflux at 10 years in adult patients with obesity: the SLEEVEPASS randomized clinical trial. JAMA Surg 157(8):656–666. https://doi.org/10.1001/jamasurg.2022.2229
Tolone S, Savarino E, de Bortoli N, Frazzoni M, Frazzoni L, Savarino V, Docimo L (2020) Esophageal high-resolution manometry can unravel the mechanisms by which different bariatric techniques produce different reflux exposures. J Gastrointest Surg 24(1):1–7. https://doi.org/10.1007/s11605-019-04406-7
Zhu J, Wu L, Chen G, Zhao X, Chen W, Dong Z, Chen X, Hu S, Xie X, Wang C, Wang H, Yang W (2022) Chinese obesity and metabolic surgery collaborative. Preoperative reflux or regurgitation symptoms are independent predictors of postoperative nausea and vomiting (PONV) in patients undergoing bariatric surgery: a propensity score matching analysis. Obes Surg 32(3):819–828. https://doi.org/10.1007/s11695-021-05859-z
Ahlqvist S, Edling A, Alm M, Dackhammar JB, Nordin P, Cengiz Y (2022) Trocar site hernia after gastric sleeve. Surg Endosc 36(6):4386–4391. https://doi.org/10.1007/s00464-021-08787-2
Möller F, Hedberg J, Skogar M, Sundbom M (2023) Long-term follow-up 15 years after duodenal switch or gastric bypass for super obesity: a randomized controlled trial. Obes Surg 33(10):2981–2990. https://doi.org/10.1007/s11695-023-06767-0
Skogar ML, Sundbom M (2020) Early complications, long-term adverse events, and quality of life after duodenal switch and gastric bypass in a matched national cohort. Surg Obes Relat Dis 16(5):614–619. https://doi.org/10.1016/j.soard.2020.02.001
Laurenius A, Taha O, Maleckas A, Lönroth H, Olbers T (2010) Laparoscopic biliopancreatic diversion/duodenal switch or laparoscopic Roux-en-Y gastric bypass for super-obesity-weight loss versus side effects. Surg Obes Relat Dis 6(4):408–414. https://doi.org/10.1016/j.soard.2010.03.293
Topart P, Becouarn G, Ritz P (2012) Comparative early outcomes of three laparoscopic bariatric procedures: sleeve gastrectomy, Roux-en-Y gastric bypass, and biliopancreatic diversion with duodenal switch. Surg Obes Relat Dis 8(3):250–254. https://doi.org/10.1016/j.soard.2011.05.012
Balamurugan G, Leo SJ, Sivagnanam ST, Balaji Prasad S, Ravindra C, Rengan V, Arora E, Bindal V (2023) Comparison of efficacy and safety between Roux-en-Y gastric bypass (RYGB) vs. one anastomosis gastric bypass (OAGB) vs. single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S): a systematic review of bariatric and metabolic surgery. Obes Surg 33(7):2194–2209. https://doi.org/10.1007/s11695-023-06602-6
Verhoeff K, Mocanu V, Jogiat U, Forbes H, Switzer NJ, Birch DW, Karmali S (2022) Patient selection and 30-day outcomes of SADI-S compared to RYGB: a retrospective cohort study of 47,375 patients. Obes Surg 32(7):1–8. https://doi.org/10.1007/s11695-022-06068-y
Surve A, Cottam D, Richards C, Medlin W, Belnap L (2021) A matched cohort comparison of long-term outcomes of Roux-en-Y gastric bypass (RYGB) versus single-anastomosis duodeno-ileostomy with sleeve gastrectomy (SADI-S). Obes Surg 31(4):1438–1448. https://doi.org/10.1007/s11695-020-05131-w
Vanetta C, Dreifuss NH, Schlottmann F, Baz C, Masrur MA (2022) Bariatric surgery conversions in MBSAQIP centers: current indications and outcomes. Obes Surg 32(10):3248–3256. https://doi.org/10.1007/s11695-022-06229-z
Yeung KTD, Penney N, Ashrafian L, Darzi A, Ashrafian H (2020) Does sleeve gastrectomy expose the distal esophagus to severe reflux?: a systematic review and meta-analysis. Ann Surg 271(2):257–265. https://doi.org/10.1097/SLA.0000000000003275
Clapp B, Harper B, Dodoo C, Klingsporn W, Barrientes A, Cutshall M, Tyroch A (2020) Trends in revisional bariatric surgery using the MBSAQIP database 2015–2017. Surg Obes Relat Dis 16(7):908–915. https://doi.org/10.1016/j.soard.2020.03.002
Sudan R, Maciejewski ML, Wilk AR, Nguyen NT, Ponce J, Morton JM (2017) Comparative effectiveness of primary bariatric operations in the United States. Surg Obes Relat Dis 13(5):826–834. https://doi.org/10.1016/j.soard.2017.01.021
Clapp B, Corbett J, Ahmad M, Vivar A, Sharma I, Hage K, Ghanem OM (2023) When do leaks occur? An analysis of the metabolic and bariatric surgery accreditation and quality improvement program. Surg Obes Relat Dis 19(10):1128–1133. https://doi.org/10.1016/j.soard.2023.04.334
Noel P, Nedelcu M, Gagner M (2016) Impact of the surgical experience on leak rate after laparoscopic sleeve gastrectomy. Obes Surg 26(8):1782–1787. https://doi.org/10.1007/s11695-015-2003-1
Ende V, Devas N, Zhang X, Yang J, Pryor AD (2023) Internal hernia trends following gastric bypass surgery. Surg Endosc 37(9):7183–7191. https://doi.org/10.1007/s00464-023-10206-7
Somerset AE, Wood MH, Bonham AJ, Carlin AM, Finks J, Ghaferi AA, Varban OA (2023) Association of program-specific variation in bariatric surgery volume for Medicaid patients and access to care: a tale of inequality? Surg Endosc 37(11):8570–8576. https://doi.org/10.1007/s00464-023-10411-4
Love KM, Mehaffey JH, Safavian D, Schirmer B, Malin SK, Hallowell PT, Kirby JL (2017) Bariatric surgery insurance requirements independently predict surgery dropout. Surg Obes Relat Dis 13(5):871–876. https://doi.org/10.1016/j.soard.2017.01.022
Alvarez R, Matusko N, Stricklen AL, Ross R, Buda CM, Varban OA (2018) Factors associated with bariatric surgery utilization among eligible candidates: who drops out? Surg Obes Relat Dis 14(12):1903–1910. https://doi.org/10.1016/j.soard.2018.08.014
Clapp B, Ponce J, Corbett J, Ghanem OM, Kurian M, Rogers AM, Peterson RM, LaMasters T, English WJ (2024) American society for metabolic and bariatric surgery 2022 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis. https://doi.org/10.1016/j.soard.2024.01.012
Kermansaravi M, Chiappetta S, Parmar C, Shikora SA, Prager G, LaMasters T, Ponce J, Kow L, Nimeri A, Kothari SN, Aarts E, Abbas SI, Aly A, Aminian A, Bashir A, Behrens E, Billy H, Carbajo MA, Clapp B, Chevallier JM, Cohen RV, Dargent J, Dillemans B, Faria SL, Neto MG, Garneau PY, Gawdat K, Haddad A, ElFawal MH, Higa K, Himpens J, Husain F, Hutter MM, Kasama K, Kassir R, Khan A, Khoursheed M, Kroh M, Kurian MS, Lee WJ, Loi K, Mahawar K, McBride CL, Almomani H, Melissas J, Miller K, Misra M, Musella M, Northup CJ, O’Kane M, Papasavas PK, Palermo M, Peterson RM, Peterli R, Poggi L, Pratt JSA, Alqahtani A, Ramos AC, Rheinwalt K, Ribeiro R, Rogers AM, Safadi B, Salminen P, Santoro S, Sann N, Scott JD, Shabbir A, Sogg S, Stenberg E, Suter M, Torres A, Ugale S, Vilallonga R, Wang C, Weiner R, Zundel N, Angrisani L, De Luca M (2024) Current recommendations for procedure selection in class I and II obesity developed by an expert modified Delphi consensus. Sci Rep 14(1):3445. https://doi.org/10.1038/s41598-024-54141-6
Funding
This work was supported by the University of North Carolina, Department of Surgery, Division of GI Surgery. The database infrastructure used for this project was funded by the Department of Epidemiology, UNC Gillings School of Global Public Health; the Cecil G. Sheps Center for Health Services Research, UNC; the CER Strategic Initiative of UNC's Clinical Translational Science Award (UL1TR001111); and the UNC School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Justin Hsu, Sherin Ismail, Maggie Hodges, Chris Agala, and Timothy Farrell have no conflicts of interest or financial ties to disclose.
Informed consent
The study was deemed exempt by the University of North Carolina, as it contained deidentified secondary data, and therefore informed consent was not required (IRB # 20-0443).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hsu, J.L., Ismail, S., Hodges, M.M. et al. Bariatric surgery: trends in utilization, complications, conversions and revisions. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-10985-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-10985-7