Abstract
Background
Virtual reality is a frequently chosen method for learning the basics of robotic surgery. However, it is unclear whether tissue handling is adequately trained in VR training compared to training on a real robotic system.
Methods
In this randomized controlled trial, participants were split into two groups for “Fundamentals of Robotic Surgery (FRS)” training on either a DaVinci VR simulator (VR group) or a DaVinci robotic system (Robot group). All participants completed four tasks on the DaVinci robotic system before training (Baseline test), after proficiency in three FRS tasks (Midterm test), and after proficiency in all FRS tasks (Final test). Primary endpoints were forces applied across tests.
Results
This trial included 87 robotic novices, of which 43 and 44 participants received FRS training in VR group and Robot group, respectively. The Baseline test showed no significant differences in force application between the groups indicating a sufficient randomization. In the Midterm and Final test, the force application was not different between groups. Both groups displayed sufficient learning curves with significant improvement of force application. However, the Robot group needed significantly less repetitions in the three FRS tasks Ring tower (Robot: 2.48 vs. VR: 5.45; p < 0.001), Knot Tying (Robot: 5.34 vs. VR: 8.13; p = 0.006), and Vessel Energy Dissection (Robot: 2 vs. VR: 2.38; p = 0.001) until reaching proficiency.
Conclusion
Robotic tissue handling skills improve significantly and comparably after both VR training and training on a real robotic system, but training on a VR simulator might be less efficient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Robot-assisted surgery (RAS) has become an accepted and standardized surgical approach following the rapid development of technology and scientific knowledge over the last two decades [1, 2]. Laparoscopy is still the method of choice, but the proportion of robotic surgery in minimally invasive abdominal surgery continues to increase [3].
Still, whereas laparoscopic training has been widely implemented in surgical residency and is sometimes even required for board certification as a surgeon, robotic training does not have nearly the same status in surgical residency and education [4, 5].
As a consequence, over one-third of surgical trainees in the USA felt inadequately trained in RAS. Similarly, in the UK and Ireland, the percentages of trainees with subjectively inadequate training were 86.2% and 91.7%, respectively [6]. At the same time, sufficient training is required because RAS is highly demanding owing to the complex technology, elaborate handling, and limitations, such as limited field of view and lack of haptic feedback [7]. In particular, the latter remains a major challenge for surgeons because most modern robotic surgery systems provide no or only rudimentary haptic feedback. However, experienced surgeons are able to compensate for this lack of haptic feedback compared to less experienced surgeons, ultimately resulting in less force being applied to the tissue [8]. It is speculated to be primarily based on a visual assessment of instrument–tissue interactions [9].
Although investigation of the force interaction between surgical instruments and tissue is a relatively new field of surgical research, it has been established that correct tissue handling is essential for surgical performance and patient safety [10]. Tissue handling as such is only part of a surgeon's technical skills, but these technical skills are generally associated with fewer complications, a lower risk of bleeding or the risk of re-operation [11]. Also, for laparoscopic surgery Tang et al. could demonstrate a correlation between excessive force and surgical errors [12, 13]. A similar relationship can be assumed in RAS. However, it is still unknown how the established basic skills training curricula for RAS affect tissue handling skills. Consequently, this trial aimed to investigate the learning curves and potential differences in tissue handling skills depending on the training modality (virtual reality training vs. training on a robotic system) after a basic robotic skills curriculum.
Methods
This investigation was designed and conducted as a prospective, randomized, controlled study. The study protocol was approved by the ethics committee of TU Dresden (decision number EK 285072016) and registered at the German Clinical Trials Register (Registry number DRKS00033919). All experimental methods were performed in accordance with the relevant guidelines, and this article was drafted and written in accordance with the CONSORT statement [14].
Participants
Written informed consent was obtained from all participants. Participants were medical students and first-year surgical residents without any formal experience in robotic surgery. Previous experience in robotic surgery or participation in RAS training courses was exclusion criteria. A questionnaire asking about basic participant characteristics (age, surgical and robotic experience, etc.) was completed by all participants.
Study design
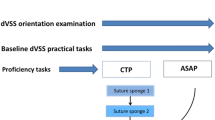
All participants received an individual introduction into the surgeon’s console of the DaVinci Xi® surgical system (Intuitive Surgical, Sunnyvale, CA, USA). Subsequently, all participants had to perform four trial tasks as Baseline test on the DaVinci Xi® surgical system (Fig. 1). The force interactions of the robotic instruments were measured during the trial tasks using a force-measuring device. Based on their respective performance in the Baseline test, the investigators randomized the participants block-wise (block-size six to 10) into two groups to ensure comparable baseline performance between the groups. Each group received the same training curriculum in two training sessions either on the DaVinci Xi virtual reality simulator (VR group) or on the real DaVinci Xi surgical system (Robot group). The trial tasks were repeated as Midterm test between the training sessions and as Final test after both training sessions on the DaVinci Xi® surgical system, respectively. Tests and training sessions were conducted on separate days and always within one week.
Training pathway
Both the VR group and Robot group underwent the same Fundamentals of Robotic Surgery (FRS) training curriculum on their respective training modality. Participants had to perform six FRS tasks in two training sessions of individual length (1st training session: Ring Tower Transfer, 4th Arm Cutting, and Railroad Track and 2nd training session: Knot Tying, Puzzle Piece Dissection, and Vessel Energy Dissection) until reaching a certain level of proficiency (min. 90 points) for each task twice. The proficiency score was calculated for both groups using the same modified scoring algorithm based on the SIMSCORE Version: BETA of the DaVinci Xi® Virtual Reality Simulator. This scoring algorithm considers task time and predefined errors as defined by SIMSCORE Version: BETA. However, the economy of motion was not integrated because it could not be measured for the Robot group.
Trial tasks
The four trial tasks for Baseline, Midterm, and Final test were the Flap task, the Precise Cut task, the Dissection task, and the Suture and Knot task (Supplementary Material). These trial tasks were designed or selected to require surgical skills similar to those of the FRS tasks. The deviation from FRS tasks ensured that neither of both groups had any advantage in performing the trial tasks.
Endpoints
The primary endpoint was tissue handling, represented by the mean non-zero force [N] and the peak force [N] exerted during the trial tasks in the Baseline, Midterm, and Final tests [15, 16]. The force parameters were measured using a force-measuring device (ForceTrap®, MediShield B.V., Delft, The Netherlands). This device can measure the force interaction in three dimensions (Unit: Newton) between robotic instruments and the respective tasks mounted on a platform attached to the ForceTrap (Supplementary Material) [17].
The force inputs were analyzed using the ForceSense software (MediShield B.V., Delft, The Netherlands) whose parameters are defined as follows:
-
Mean non-zero force: the mean of all forces during a task excluding all periods with zero force exertion
-
Peak force: maximum force applied during a task
The secondary endpoints were the time of completion [s] and the occurrence of predefined errors during any trial task (Supplementary Material). The learning curves were defined as the change in task time, mean non-zero force, and peak force over the course of the trial tasks (baseline, midterm, and final). For the FRS training tasks, the number of repetitions until attaining proficiency at the respective modality was counted.
Statistical analysis
All the statistical analyses were performed using SPSS version 26 (IBM Corp., Armonk, NY, USA). Kolmogorov–Smirnov tests were used to check the normality of the continuous data. Variables are represented either as mean values (mean) and standard deviations (SD) for continuous variables or as distributions of frequencies. Differences between groups were tested using the Student’s t-test or Mann–Whitney U-Test depending on the distribution of normality. For the analysis of varying error incidence, a Chi2-test was chosen. Learning curves were analyzed using a general linear model with repeated measurements and post-hoc Bonferroni corrections. The threshold for the level of significance was set at p = 0.05. A preceding power analysis was not performed owing to the lack of data on the potential effect size.
Results
Basic participant characteristics
For this trial, 87 participants were randomized into a Robot group (n = 44) and into a VR group (n = 43). The 50 (57.8%) female participants outweighed the 37 (42.5%) male participants. The mean age was 24.9 (SD 3.5) years. None of the participants had attended a training course on robot-assisted surgeries. However, 35 participants (40.2%) reported previous experience in laparoscopic surgery (e.g., assistance, camera holding), 28 (32.2%) participants completed a training course for laparoscopic surgery, and 9 (10.3%) had used the Da Vinci Surgical System before but did not receive any formal training or participated in robotic surgeries as console surgeons (Table 1).
Comparison between the Robot and VR group: Baseline test
There were no significant differences between the Robot and VR groups in any task in the Baseline test for completion time, mean non-zero force, or peak force (Table 2). In addition, both groups made comparable numbers of major errors during the Baseline test (Table 3).
Comparison between the Robot and VR group: Midterm test
There was a slight loss to follow-up in the Midterm test with 42 and 41 participants remaining in the Robot and VR group, respectively. In the Midterm test, the Robot group showed significantly faster task completion times in Flap task (Robot:59.2 s vs. VR:73.4 s; p = 0.007) and Suture and Knot task (Robot:183.8 s vs. VR:227.2 s; p = 0.006) (Table 2). Except for the mean non-zero force in the Dissection and the Suture and Knot task, all other results were more favorable in the Robot group compared to the VR group. However, these differences were not statistically significant. Similarly, on the Midterm test, the number of errors did not differ between the two groups for any task (Table 3).
Comparison between the Robot and VR group: Final test
Despite not reaching significance, the Final test showed a clear tendency in favor of the Robot group (Table 2). In the Final test, a further slight loss to follow-up with 40 and 38 participants in the Robot and VR group, respectively, was noted. Apart from a better peak-force values by the VR group in the Dissection task, the Robot group performed better in the Flap task (Robot:2.4 N vs. VR:3.2 N; p = 0.113), the Precise Cut task (Robot:1.8 vs. VR:1.9; p = 0.115), and in the Suture and Knot task (Robot:4.1 N vs. VR:4.7 N; p = 0.086). The differences in the mean non-zero force were less pronounced, but again in favor of the Robot group in the Flap task (Robot:0.8 N vs. VR:0.9 N; p = 0.815), the Dissection task (Robot:1.2 N vs. VR:1.3 N; p = 0.206), and the Suture and Knot task (Robot:1.2 N vs. VR:1.3 N; p = 0.103). In the Precise Cut task, both groups performed equally in terms of the mean non-zero force (Robot:0.5 N vs. VR:0.5 N; p = 0.826).
The tendency in favor of the Robot group could also be seen regarding the task times for Flap task (Robot:59 s vs. VR:64.2 s; p = 0.266), Precise Cut task (Robot:160.9 s vs. VR:175.6 s; p = 0.255), Dissection task (Robot:399.6 s vs. VR:401 s; p = 0.964), and Suture and Knot task (Robot:170.5 s vs. VR:182.4 s; p = 0.384).
There were no significant differences in the occurrence of errors and no tendencies were observed in the Final test (Table 3).
Learning curve for task time
Both groups showed an overall significant improvement in task completion time for all tasks (Table 4; Fig. 2a). However, the Robot group improved significantly mainly between Baseline and Midterm test in the Flap task (p < 0.05), the Dissection task (p < 0.05), and the Suture and Knot task (p < 0.05) and the further development between Midterm and Final test did not show significant differences. A significant improvement between all tests was observed only in the Precise Cut task for the Robot group.
For the VR group, the improvement of task completion time was significant between all tests in the Flap task (p < 0.05), the Precise Cut task (p < 0.05), and the Suture and Knot task (p < 0.001) (Table 4; Fig. 2b). In the Dissection task, significant improvement was observed only between Baseline and Midterm (p < 0.05) but not between the Midterm and Final tests.
Learning curve for mean non-zero force
Regarding the mean non-zero force, the Robot group showed a tendency but no significant improvement in the Flap task, Precise Cut task, or Dissection task (Table 4; Fig. 2c). An overall improvement with the steepest improvement between Midterm and Final test could be seen in the Suture and Knot task (p < 0.01).
In the VR group, the learning curve for mean non-zero force was not significant for the Flap task (p > 0.05) (Table 4; Fig. 2d). The Precise Cut task showed an significant overall improvement (p < 0.01). Here, an overall improvement with the steepest improvement between Baseline and Midterm test was observed in the Dissection task (p < 0.05) and Suture and Knot task (p < 0.01).
Learning curve for peak force
The learning curves of peak-force exertion showed a significant and comparable improvement in both groups for all tasks (Table 4; Fig. 2e). For the Robot group, a significant overall improvement of peak forces was seen in all tasks (Flap: p < 0.01; Precise Cut: p < 0.01; Dissection: p < 0.05; Suture and Knot: p < 0.05). With the exception of the Precise Cut task, all other tasks additionally showed a significant improvement between Baseline and Midterm test.
The VR group (Table 4; Fig. 2f) showed a significant overall improvement in peak forces (Flap: p < 0.05; Precise Cut: p < 0.01; Dissection: p < 0.05; Suture and Knot: p < 0.01). Again, with the exception of the Precise Cut task, all other tasks also improved significantly between Baseline and Midterm test.
Learning efficiency
The number of FRS task repetitions (Ring Tower Transfer, 4th Arm Cutting, Railroad Track, Knot Tying, Puzzle Piece Dissection, Vessel Energy Dissection) performed by each participant until reaching proficiency was counted and compared between the two groups (Table 5). Interestingly, the VR group needed significantly more repetitions in the FRS Ring tower (Robot:2.48 vs. VR: 5.45; p < 0.001), Knot Tying (Robot: 5.34 vs. VR: 8.13; p = 0.006), and Vessel Energy Dissection (Robot: 2 vs. VR: 2.38; p = 0.001) tasks until reaching proficiency.
Discussion
Recently, various training curricula for robot-assisted surgery have been developed, tested, and partially validated. FRS have been developed for learning basic robotic surgery skills and are available on most VR training simulators, as well as training on a real-world robotic surgical system.
Regarding task completion time and occurrence of errors, VR training has already proven to be as effective as the same curriculum using a robotic surgical system [18]. However, this trial did not include any analysis of tissue handling or objective force measurement, although it is well known that the lack of haptic feedback remains a major shortcoming of RAS. Hence, data regarding the force interaction between robotic instruments and tissues are scarce, and consequently, tissue handling has never been the focus of basic skills training curricula for RAS.
The present trial provided detailed information on the learning curve for tissue handling over an FRS-based course for robotic novices. Both training on the robotic surgical system and using the VR simulator showed a significant reduction in tissue handling forces. In general, both groups showed steep and significant improvements in time and force exertion over the course of the training. This indicates that the FRS curriculum-driven training can sufficiently help to develop tissue handling skills, even though the FRS was not specifically designed for teaching and rating tissue handling.
Our findings are supported by a recent study that demonstrated similar reductions in force and time for a repeated robotic suturing task, but without comparison with VR training. In addition, the range of the peak and mean non-zero forces observed by Rahimi et al. was comparable to our measurements [16].
The application of force is significantly influenced by the tissue type, haptic feedback combined with visual assessment, and surgical experience [19]. It is therefore not surprising that there are significant differences between surgical experts and beginners, with the latter using more excessive force [20, 21]. However, these studies did not take RAS into account, whereby in RAS the visual assessment of the interaction between robotic instruments and tissue is thought to play the major role in compensating for missing haptic feedback [9, 22]. Unlike surgical experience, such visual assessment can be trained, but requires a realistic training scenario with high-quality simulation of force interaction between instruments and tissue. It was questionable if VR simulator can provide such a realistic force and haptic feedback simulation [23]. Overtoom et al. were the first to conclude that laparoscopic VR training with simulated forces and haptic feedback leads to only minor improvements for surgical novices compared to force feedback provided by a laparoscopic box-trainer [24].
For RAS, a similar comparison has been missing thus far, in part because there is no haptic feedback in RAS and therefore the difference between training in VR and on a robotic system may have been considered less relevant; therefore, we aimed to investigate the potential differences in the learning of tissue handling depending on the training modality. Consequently, our data suggest that there are no significant differences in the development of tissue handling skills and force interactions depending on the training modality. The comparable Baseline test showed sufficient randomization into the VR and Robot groups. The Midterm and Final tests showed no significant differences in force exertion between the groups but showed an overall tendency in favor of the Robot group. This indicates a slight advantage of training with a real robotic system.
When comparing the efficiency of VR training with training on a surgical robotic system, we found that the Robot group required significantly fewer sessions for three of the six FRS training tasks (Ring tower, Knot, and Vessel Dissection task) to achieve the required competency. In particular, for the Knot task, the VR group struggled regularly with the simulated thread. Here, the limited realism of the VR simulation could be the cause of the poorer performance and thus lead to a less efficient and even frustrating training experience.
Strengths and limitations
To the best of our knowledge, this is the first randomized trial to analyze and compare the learning curves of tissue handling between training for RAS using VR simulators and a robotic surgical system. To increase comparability, the participants were purposefully chosen to be naïve to RAS. In particular, the distinction in surgical experience based on the respective tissue handling skills in RAS has been observed previously [16].
The relevance of the observed tissue handling skills and their transferability to the OR remain vague and partially unknown. A force interaction of approximately 2 N is discussed as a threshold for damage to certain tissues (e.g., large intestine) in a suture-like scenario [25]. In our study, both groups exceeded this threshold by far in the Suture and Knot task even after completing the FRS training. Organ-specific differences were shown by the damage occurring after 20 N grasping force in intestine and 1 N grasping force in liver [26, 27]. However, the data supporting these claims were collected in animal experiments and may not be applicable to humans.
The data shown were collected using the most common robotic surgical system, the DaVinci Xi surgical system, and the most common robotic VR trainer, the DaVinci Xi Virtual Reality simulator. However, other robotic systems or VR simulators could potentially yield different results. Novel developments in RAS already provide some sort of haptic feedback and may change the relevance of our findings and conclusions. Alternatively, successful attempts have been made to use optical data to estimate the force estimation [28,29,30,31].
Still, the importance of haptic feedback should not be underestimated, since providing haptic and tactile feedback improves the surgeon’s force application toward the tissue, decreasing tissue damage and surgical performance in general [8, 32]. Notwithstanding, the integration of haptic feedback does not exempt the need for training. Singapore et al. concluded that at least for laparoscopy, receiving haptic feedback per se and processing force cues would also require training [23]. Also, future robotic systems might even incorporate feedback technology that exceeds the human tactile sense. It therefore remains to be seen whether and how the implementation of haptic feedback in surgical robotic systems might change RAS training.
Eventually, the exploratory nature of this study meant that a preceding power analysis was not possible. It is therefore possible that this study was underpowered and possible measurement differences would only have become apparent after the inclusion of additional participants.
Conclusion
Tissue handling in RAS is particularly demanding because of the lack of haptic feedback and requires extensive and specialized training. The results of our study indicate that the FRS curriculum can significantly improve tissue handling, with no differences in outcomes between robotic and VR training modalities. However, VR training might be slightly less efficient in terms of task repetitions needed to reach proficiency.
Still, objective assessment of tissue handling should be integrated into RAS training. Robotic surgical systems with implemented haptic feedback may help improve force exertion and also training for RAS to some extent. However, the transferability of robotic surgery tissue handling skills to the operating room is still unknown and should be the subject of future studies.
References
Lu H, Han T, Li F, Yang J, Hou Z (2022) Global trends and hotspots in research of robotic surgery in oncology: a bibliometric and visual analysis from 2002 to 2021. Front Oncol 12:1–18. https://doi.org/10.3389/fonc.2022.1055118
Juo YY, Mantha A, Abiri A, Lin A, Dutson E (2018) Diffusion of robotic-assisted laparoscopic technology across specialties: a national study from 2008 to 2013. Surg Endosc 32(3):1405–1413. https://doi.org/10.1007/s00464-017-5822-4
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):1–9. https://doi.org/10.1001/jamanetworkopen.2019.18911
von Bechtolsheim F, Schneider A, Schmidt S et al (2024) Satisfaction of surgeons with the current state of training in minimally invasive surgery: a survey among German surgeons. Surg Endosc 38(2):1029–1044. https://doi.org/10.1007/s00464-023-10584-y
Tom CM, Maciel JD, Korn A et al (2019) A survey of robotic surgery training curricula in general surgery residency programs: how close are we to a standardized curriculum? Am J Surg 217(2):256–260. https://doi.org/10.1016/j.amjsurg.2018.11.006
Gall TMH, Malhotra G, Elliott JA, Conneely JB, Fong Y, Jiao LR (2022) The Atlantic divide: contrasting surgical robotics training in the USA, UK and Ireland. J Robot Surg 17(1):117–123. https://doi.org/10.1007/s11701-022-01399-5
Supe A, Kulkarni G, Supe P (2010) Ergonomics in laparoscopic surgery. J Minim Access Surg 6(2):31. https://doi.org/10.4103/0972-9941.65161
Wottawa CR, Genovese B, Nowroozi BN et al (2016) Evaluating tactile feedback in robotic surgery for potential clinical application using an animal model. Surg Endosc 30(8):3198–3209. https://doi.org/10.1007/s00464-015-4602-2
Meccariello G, Faedi F, AlGhamdi S et al (2016) An experimental study about haptic feedback in robotic surgery: may visual feedback substitute tactile feedback? J Robot Surg 10(1):57–61. https://doi.org/10.1007/s11701-015-0541-0
Golahmadi AK, Khan DZ, Mylonas GP, Marcus HJ (2021) Tool-tissue forces in surgery: a systematic review. Ann Med Surg 65:102268. https://doi.org/10.1016/j.amsu.2021.102268
Woods MS, Liberman JN, Rui P et al (2023) Association between surgical technical skills and clinical outcomes: a systematic literature review and meta-analysis. JSLS J Soc Laparosc Robot Surg 27(1):e2022.00076. https://doi.org/10.4293/JSLS.2022.00076
Tang B, Hanna GB, Cuschieri A (2005) Analysis of errors enacted by surgical trainees during skills training courses. Surgery 138(1):14–20. https://doi.org/10.1016/j.surg.2005.02.014
Tang B, Hanna GB, Joice P, Cuschieri A (2004) Identification and categorization of technical errors by observational clinical human reliability assessment (OCHRA) during laparoscopic cholecystectomy. Arch Surg 139(11):1215–1220. https://doi.org/10.1001/archsurg.139.11.1215
Moher D, Hopewell S, Schulz KF et al (2010) CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol 63(8):e1–e37. https://doi.org/10.1016/j.jclinepi.2010.03.004
Hardon SF, Horeman T, Bonjer HJ, Meijerink WJHJ (2018) Force-based learning curve tracking in fundamental laparoscopic skills training. Surg Endosc 32(8):3609–3621. https://doi.org/10.1007/s00464-018-6090-7
Rahimi AM, Hardon SF, Willuth E et al (2023) Force-based assessment of tissue handling skills in simulation training for robot-assisted surgery. Surg Endosc. https://doi.org/10.1007/s00464-023-09905-y
Horeman T, Blikkendaal MD, Feng D et al (2014) Visual force feedback improves Knot-tying security. J Surg Educ 71(1):133–141. https://doi.org/10.1016/j.jsurg.2013.06.021
Satava RM, Stefanidis D, Levy JS et al (2020) Proving the effectiveness of the fundamentals of robotic surgery (FRS) skills curriculum. Ann Surg 272(2):384–392. https://doi.org/10.1097/SLA.0000000000003220
Susmitha WK, Mathew G, Devasahayam SR, Perakath B, Velusamy SK (2015) Factors influencing forces during laparoscopic pinching: towards the design of virtual simulator. Int J Surg 18:211–215. https://doi.org/10.1016/j.ijsu.2015.04.078
Sugiyama T, Lama S, Gan LS, Maddahi Y, Zareinia K, Sutherland GR (2018) Forces of tool-tissue interaction to assess surgical skill level. JAMA Surg 153(3):234–242. https://doi.org/10.1001/jamasurg.2017.4516
Araki A, Makiyama K, Yamanaka H et al (2017) Comparison of the performance of experienced and novice surgeons: measurement of gripping force during laparoscopic surgery performed on pigs using forceps with pressure sensors. Surg Endosc 31(4):1999–2005. https://doi.org/10.1007/s00464-016-5153-x
Munawar A, Fischer G (2016) A surgical robot teleoperation framework for providing haptic feedback incorporating virtual environment-based guidance. Front Robot AI 3:1–15. https://doi.org/10.3389/frobt.2016.00047
Singapogu R, Burg T, Burg KJL, Smith DE, Eckenrode AH (2014) A perspective on the role and utility of haptic feedback in laparoscopic skills training. Crit Rev Biomed Eng 42(3–4):293–318. https://doi.org/10.1615/CritRevBiomedEng.2014011701
Overtoom EM, Horeman T, Jansen FW, Dankelman J, Schreuder HWR (2019) Haptic feedback, force feedback, and force-sensing in simulation training for laparoscopy: a systematic overview. J Surg Educ 76(1):242–261. https://doi.org/10.1016/j.jsurg.2018.06.008
Rodrigues SP, Horeman T, Dankelman J, van den Dobbelsteen JJ, Jansen FW (2012) Suturing intraabdominal organs: when do we cause tissue damage? Surg Endosc 26(4):1005–1009. https://doi.org/10.1007/s00464-011-1986-5
Barrie J, Russell L, Hood AJ, Jayne DG, Neville A, Culmer PR (2018) An in vivo analysis of safe laparoscopic grasping thresholds for colorectal surgery. Surg Endosc 32(10):4244–4250. https://doi.org/10.1007/s00464-018-6172-6
Okuda Y, Nakai A, Sato T et al (2022) New device with force sensors for laparoscopic liver resection–investigation of grip force and histological damage. Minim Invasive Ther Allied Technol 31(1):28–33. https://doi.org/10.1080/13645706.2020.1755313
Chua Z, Jarc AM, Okamura AM (2021) Toward force estimation in robot-assisted surgery using deep learning with vision and robot state. 2021 IEEE international conference on robotics and automation (ICRA). IEEE, New York, pp 12335–12341. https://doi.org/10.1109/ICRA48506.2021.9560945
Edwards PJE, Colleoni E, Sridhar A, Kelly JD, Stoyanov D (2021) Visual kinematic force estimation in robot-assisted surgery-application to knot tying. Comput Methods Biomech Biomed Eng Imaging Vis 9(4):414–420. https://doi.org/10.1080/21681163.2020.1833368
Neidhardt M, Mieling R, Bengs M, Schlaefer A (2023) Optical force estimation for interactions between tool and soft tissues. Sci Rep 13(1):506. https://doi.org/10.1038/s41598-022-27036-7
Aviles AI, Alsaleh SM, Hahn JK, Casals A (2017) Towards retrieving force feedback in robotic-assisted surgery: a supervised neuro-recurrent-vision approach. IEEE Trans Haptics 10(3):431–443. https://doi.org/10.1109/TOH.2016.2640289
Miller J, Braun M, Bilz J et al (2021) Impact of haptic feedback on applied intracorporeal forces using a novel surgical robotic system—a randomized cross-over study with novices in an experimental setup. Surg Endosc 35(7):3554–3563. https://doi.org/10.1007/s00464-020-07818-8
Funding
Open Access funding enabled and organized by Projekt DEAL. Jürgen Weitz, Marius Distler, Felix von Bechtolsheim, and Grit Krause-Jüttler were funded by the German Research Foundation (DFG, Deutsche Forschungsgemeinschaft) as part of Germany’s Excellence Strategy—EXC 2050/1—Project ID 390696704—Cluster of Excellence “Centre for Tactile Internet with Human-in-the-Loop” (CeTI) of Technische Universität Dresden.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Felix von Bechtolsheim, Andreas Franz, Sofia Schmidt, Alfred Schneider, Felicitas La Rosée, Olga Radulova-Mauersberger, Grit Krause-Jüttler, Anja Hümpel, Sebastian Bodenstedt, Stefanie Speidel, Jürgen Weitz, Marius Distler, and Florian Oehme have no conflicts of interest or financial ties to disclosure.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
von Bechtolsheim, F., Franz, A., Schmidt, S. et al. The development of tissue handling skills is sufficient and comparable after training in virtual reality or on a surgical robotic system: a prospective randomized trial. Surg Endosc 38, 2900–2910 (2024). https://doi.org/10.1007/s00464-024-10842-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10842-7