Abstract
Background
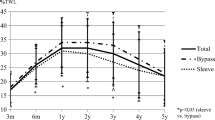
Obesity-related comorbidities may relapse in patients with weight regain after bariatric surgery. However, HDL cholesterol (HDLc) levels increase after surgery and seem to remain stable despite a gradual increase in BMI. The aim of this study is to analyze the effects of weight regain after bariatric surgery on HDL cholesterol.
Materials and methods
This is a retrospective, observational, cohort study in patients who underwent bariatric surgery in the Hospital de la Santa Creu i Sant Pau (Barcelona) between 2007 and 2015. Patients without at least 5 years of follow-up after surgery, under fibrate treatment, and those who required revisional surgery were excluded from the analysis. Data were collected at baseline, 3 and 6 months after surgery, and then annually until 5 years post-surgery.
Results
One hundred fifty patients were analyzed. 93.3% of patients reached > 20% of total weight loss after surgery. At 5th year, 37% of patients had regained > 15% of nadir weight, 60% had regained > 10%, and 22% had regained < 5% of nadir weight. No differences were found in HDLc levels between the different groups of weight regain, nor in the % of change in HDLc levels between nadir weight and 5 years, or in the proportion of patients with normal HDLc concentrations either.
Conclusion
HDLc remains stable regardless of weight regain after bariatric surgery.
Graphical abstract



Similar content being viewed by others
Data availability
The data presented in this study are available upon reasonable request from the corresponding author.
References
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, Lystig T, Sullivan M, Bouchard C, Carlsson B, Bengtsson C, Dahlgren S, Gummesson A, Jacobson P, Karlsson J, Lindroos A-K, Lönroth H, Näslund I, Olbers T, Stenlöf K, Torgerson J, Ågren G, Carlsson LMS (2007) Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 357:741–752. https://doi.org/10.1056/NEJMoa066254
Roth AE, Thornley CJ, Blackstone RP (2020) Outcomes in bariatric and metabolic surgery: an updated 5-year review. Curr Obes Rep 9:380–389
Noria SF, Shelby RD, Atkins KD, Nguyen NT, Gadde KM (2023) Weight regain after bariatric surgery: scope of the problem, causes, prevention, and treatment. Curr Diabetes Rep 23:31–42. https://doi.org/10.1007/s11892-023-01498-z
Lopes KG, Romagna EC, da Silva DS, da Costa Tavares Bezerra M, Leal PRF, da Silva Soares Pinto JE, Bouskela E, das Graças Coelho de Souza M, Kraemer-Aguiar LG (2022) Metabolic and inflammatory profiles of post-bariatric patients with weight recidivism. Obes Surg 32:1849–1855. https://doi.org/10.1007/s11695-022-06025-9
Aaseth JO, Rootwelt H, Retterstøl K, Hestad K, Farup PG (2022) Circulating lipoproteins in subjects with morbid obesity undergoing bariatric surgery with gastric bypass or sleeve gastrectomy. Nutrients 14:2381. https://doi.org/10.3390/nu14122381
Beamish AJ, Olbers T, Kelly AS, Inge TH (2016) Cardiovascular effects of bariatric surgery. Nat Rev Cardiol 13:730–743. https://doi.org/10.1038/nrcardio.2016.162
Genua I, Puig N, Miñambres I, Benítez S, Gil P, Grau-Agramunt M, Rivas-Urbina A, Balagué C, Fernández-Alanin S, García-Osuna Á, Pérez A, Sánchez-Quesada JL (2021) Changes in the composition and function of lipoproteins after bariatric surgery in patients with severe obesity. J Clin Med 10:1716. https://doi.org/10.3390/jcm10081716
Lorkowski SW, Brubaker G, Rotroff DM, Kashyap SR, Bhatt DL, Nissen SE, Schauer PR, Aminian A, Smith JD (2020) Bariatric surgery improves HDL function examined by ApoA1 exchange rate and cholesterol efflux capacity in patients with obesity and type 2 diabetes. Biomolecules 10:551. https://doi.org/10.3390/biom10040551
Thakkar H, Vincent V, Shukla S, Sra M, Kanga U, Aggarwal S, Singh A (2021) Improvements in cholesterol efflux capacity of HDL and adiponectin contribute to mitigation in cardiovascular disease risk after bariatric surgery in a cohort with morbid obesity. Diabetol Metab Syndr 13:46. https://doi.org/10.1186/s13098-021-00662-3
Adam S, Ho JH, Liu Y, Siahmansur T, Siddals K, Iqbal Z, Azmi S, Senapati S, New J, Jeziorska M, Ammori BJ, Syed AA, Donn R, Malik RA, Durrington PN, Soran H (2022) Bariatric surgery-induced high-density lipoprotein functionality enhancement is associated with reduced inflammation. J Clin Endocrinol Metab 107:2182–2194. https://doi.org/10.1210/clinem/dgac244
Jayaraman S, Pérez A, Miñambres I, Sánchez-Quesada JL, Gursky O (2023) LDL binding to cell receptors and extracellular matrix is proatherogenic in obesity but improves after bariatric surgery. J Lipid Res. https://doi.org/10.1016/j.jlr.2023.100451
Genua I, Ramos A, Caimari F, Balagué C, Sánchez-Quesada JL, Pérez A, Miñambres I (2020) Effects of bariatric surgery on HDL cholesterol. Obes Surg. https://doi.org/10.1007/s11695-020-04385-8
Nicoletti CF, de Oliveira BAP, de Pinhel MAS, Donati B, Marchini JS, Salgado Junior W, Nonino CB (2015) Influence of excess weight loss and weight regain on biochemical indicators during a 4-year follow-up after Roux-en-Y gastric bypass. Obes Surg 25:279–284. https://doi.org/10.1007/s11695-014-1349-0
Benaiges D, Bisbe M, Pedro-botet J, de Vargas-Machuca A, Ramon JM, Pera M, Villatoro M, Fontané L, Julià H, Climent E, Castañer O, Flores-Le Roux JA, Goday A (2020) Additional metabolic effects of bariatric surgery in patients with a poor mid-term weight loss response: a 5-year follow-up study. J Clin Med 9:1–12. https://doi.org/10.3390/jcm9103193
(1991) NIH conference. Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med 115:956–961
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, de Backer G, Heagerty AM, Agewall S, Bochud M, Borghi C, Boutouyrie P, Brguljan J, Bueno H, Caiani EG, Carlberg B, Chapman N, Cífková R, Cleland JGF, Collet J-P, Coman IM, de Leeuw PW, Delgado V, Dendale P, Diener H-C, Dorobantu M, Fagard R, Farsang C, Ferrini M, Graham IM, Grassi G, Haller H, Hobbs FDR, Jelakovic B, Jennings C, Katus HA, Kroon AA, Leclercq C, Lovic D, Lurbe E, Manolis AJ, McDonagh TA, Messerli F, Muiesan ML, Nixdorff U, Olsen MH, Parati G, Perk J, Piepoli MF, Polonia J, Ponikowski P, Richter DJ, Rimoldi SF, Roffi M, Sattar N, Seferovic PM, Simpson IA, Sousa-Uva M, Stanton AV, van de Borne P, Vardas P, Volpe M, Wassmann S, Windecker S, Zamorano JL, Windecker S, Aboyans V, Agewall S, Barbato E, Bueno H, Coca A, Collet J-P, Coman IM, Dean V, Delgado V, Fitzsimons D, Gaemperli O, Hindricks G, Iung B, Jüni P, Katus HA, Knuuti J, Lancellotti P, Leclercq C, McDonagh TA, Piepoli MF, Ponikowski P, Richter DJ, Roffi M, Shlyakhto E, Simpson IA, Sousa-Uva M, Zamorano JL, Tsioufis C, Lurbe E, Kreutz R, Bochud M, Rosei EA, Jelakovic B, Azizi M, Januszewics A, Kahan T, Polonia J, van de Borne P, Williams B, Borghi C, Mancia G, Parati G, Clement DL, Coca A, Manolis A, Lovic D, Benkhedda S, Zelveian P, Siostrzonek P, Najafov R, Pavlova O, de Pauw M, Dizdarevic-Hudic L, Raev D, Karpettas N, Linhart A, Olsen MH, Shaker AF, Viigimaa M, Metsärinne K, Vavlukis M, Halimi J-M, Pagava Z, Schunkert H, Thomopoulos C, Páll D, Andersen K, Shechter M, Mercuro G, Bajraktari G, Romanova T, Trušinskis K, Saade GA, Sakalyte G, Noppe S, DeMarco DC, Caraus A, Wittekoek J, Aksnes TA, Jankowski P, Polonia J, Vinereanu D, Baranova EI, Foscoli M, Dikic AD, Filipova S, Fras Z, Bertomeu-Martínez V, Carlberg B, Burkard T, Sdiri W, Aydogdu S, Sirenko Y, Brady A, Weber T, Lazareva I, de Backer T, Sokolovic S, Jelakovic B, Widimsky J, Viigimaa M, Pörsti I, Denolle T, Krämer BK, Stergiou GS, Parati G, Trušinskis K, Miglinas M, Gerdts E, Tykarski A, de Carvalho Rodrigues M, Dorobantu M, Chazova I, Lovic D, Filipova S, Brguljan J, Segura J, Gottsäter A, Pechère-Bertschi A, Erdine S, Sirenko Y, Brady A (2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 39:3021–3104. https://doi.org/10.1093/eurheartj/ehy339
American Diabetes Association (2018) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes—2018. Diabetes Care 41:S13–S27. https://doi.org/10.2337/dc18-S002
Digiorgi M, Rosen DJ, Choi JJ, Milone L, Schrope B, Olivero-Rivera L, Restuccia N, Yuen S, Fisk M, Inabnet WB, Bessler M (2010) Re-emergence of diabetes after gastric bypass in patients with mid- to long-term follow-up. Surg Obes Relat Dis 6:249–253. https://doi.org/10.1016/j.soard.2009.09.019
Debédat J, Sokolovska N, Coupaye M, Panunzi S, Chakaroun R, Genser L, de Turenne G, Bouillot J-L, Poitou C, Oppert J-M, Blüher M, Stumvoll M, Mingrone G, Ledoux S, Zucker J-D, Clément K, Aron-Wisnewsky J (2018) Long-term relapse of type 2 diabetes after Roux-en-Y gastric bypass: prediction and clinical relevance. Diabetes Care 41:2086–2095. https://doi.org/10.2337/dc18-0567
Brissman M, Beamish AJ, Olbers T, Marcus C (2021) Prevalence of insufficient weight loss 5 years after Roux-en-Y gastric bypass: metabolic consequences and prediction estimates: a prospective registry study. BMJ Open. https://doi.org/10.1136/bmjopen-2020-046407
Voorwinde V, Steenhuis IHM, Janssen IMC, Monpellier VM, van Stralen MM (2020) Definitions of long-term weight regain and their associations with clinical outcomes. Obes Surg 30:527–536. https://doi.org/10.1007/s11695-019-04210-x
King WC, Hinerman AS, Belle SH, Wahed AS, Courcoulas AP (2018) Comparison of the performance of common measures of weight regain after bariatric surgery for association with clinical outcomes. J Am Med Assoc 320:1560–1569. https://doi.org/10.1001/jama.2018.14433
Capoccia D, Guida A, Coccia F, Guarisco G, Testa M, Leonetti F, Silecchia G (2020) Weight regain and diabetes evolution after sleeve gastrectomy: a cohort study with over 5 years of follow-up. Obes Surg 30:1046–1051. https://doi.org/10.1007/s11695-019-04350-0
Torrego-Ellacuría M, Barabash A, Larrad-Sainz A, Hernández-Nuñez GM, Matía-Martín P, Pérez-Ferre N, Marcuello C, Sánchez-Pernaute A, Torres AJ, Calle-Pascual AL, Rubio MA (2021) Weight regain outcomes after bariatric surgery in the long-term follow-up: role of preoperative factors. Obes Surg 31:3947–3955. https://doi.org/10.1007/s11695-021-05497-5
Grover BT, Morell MC, Kothari SN, Borgert AJ, Kallies KJ, Baker MT (2019) Defining weight loss after bariatric surgery: a call for standardization. Obes Surg 29:3493–3499. https://doi.org/10.1007/s11695-019-04022-z
El AW, Elhag W (2021) Weight regain and insufficient weight loss after bariatric surgery: definitions, prevalence, mechanisms, predictors, prevention and management strategies, and knowledge gaps—a scoping review. Obes Surg. https://doi.org/10.1007/s11695-020-05160-5
King WC, Hinerman AS, Courcoulas AP (2020) Weight regain after bariatric surgery: a systematic literature review and comparison across studies using a large reference sample. Surg Obes Relat Dis 16:1133–1144. https://doi.org/10.1016/j.soard.2020.03.034
da Silva FBL, Gomes DL, de Carvalho KMB (2016) Poor diet quality and postoperative time are independent risk factors for weight regain after Roux-en-Y gastric bypass. Nutrition 32:1250–1253. https://doi.org/10.1016/j.nut.2016.01.018
Odom J, Zalesin KC, Washington TL, Miller WW, Hakmeh B, Zaremba DL, Altattan M, Balasubramaniam M, Gibbs DS, Krause KR, Chengelis DL, Franklin BA, McCullough PA (2010) Behavioral predictors of weight regain after bariatric surgery. Obes Surg 20:349–356. https://doi.org/10.1007/s11695-009-9895-6
Monaco-Ferreira DV, Leandro-Merhi VA (2017) Weight regain 10 years after Roux-en-Y gastric bypass. Obes Surg 27:1137–1144. https://doi.org/10.1007/s11695-016-2426-3
Livhits M, Mercado C, Yermilov I, Parikh JA, Dutson E, Mehran A, Ko CY, Gibbons MM (2011) Patient behaviors associated with weight regain after laparoscopic gastric bypass. Obes Res Clin Pract 5:e258–e265. https://doi.org/10.1016/j.orcp.2011.03.004
Bastos ECL, Barbosa EMWG, Soriano GMS, dos Santos EA, Vasconcelos SML (2013) Determinants of weight regain after bariatric surgery. Arq Bras Cir Dig 26(Suppl 1):26–32. https://doi.org/10.1590/S0102-67202013000600007
Freire RH, Borges MC, Alvarez-Leite JI, Correia MITD (2012) Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition 28:53–58. https://doi.org/10.1016/j.nut.2011.01.011
Nienov OH, Machado FD, Dias LS, de Carli LA, Schmid H (2020) Effect of bariatric surgery on high-density lipoprotein (HDL) cholesterol in non-diabetic patients with severe obesity. Obes Surg 30:154–160. https://doi.org/10.1007/s11695-019-04126-6
Climent E, Benaiges D, Goday A, Villatoro M, Julià H, Ramón JM, Flores JA, Pedro-Botet J (2020) Obesidad mórbida y dislipemia: impacto de la cirugía bariátrica. Clínica e Investigación en Arteriosclerosis 32:79–86. https://doi.org/10.1016/j.arteri.2019.11.001
Laguna S, Andrada P, Silva C, Rotellar F, Valenti V, Gil MJ, Gómez-Ambrosi J, Frühbeck G, Salvador J (2016) Las variaciones en colesterol-HDL tras bypass gástrico proximal son independientes de la evolución ponderal. An Sist Sanit Navar 39:23–33. https://doi.org/10.4321/S1137-6627/2016000100004
Peng Y-M, Ou J-S (2022) HDL and surgery. In: Zheng L (ed) HDL metabolism and diseases, AEMB, vol 1377. Springer, Singapore, pp 189–195. https://doi.org/10.1007/978-981-19-1592-5_15
Piché M-E, Tardif I, Auclair A, Poirier P (2021) Effects of bariatric surgery on lipid-lipoprotein profile. Metabolism 115:154441. https://doi.org/10.1016/j.metabol.2020.154441
Santos AL, da Silva SA, Cavalcante-E-Silva LM, de Albuquerque Leão LH, Coutinho LR, de Santa Cruz Oliveira FD, Ferraz ÁAB (2023) Weight regain and the metabolic profile of women in the postoperative period of bariatric surgery: a multivariate analysis. Arquivos Brasileiros de Cirurgia Digestiva (São Paulo). https://doi.org/10.1590/0102-672020230037e1755
Ouimet M, Barrett TJ, Fisher EA (2019) HDL and reverse cholesterol transport. Circ Res 124:1505–1518. https://doi.org/10.1161/CIRCRESAHA.119.312617
Rosenson RS, Brewer HB, Ansell BJ, Barter P, Chapman MJ, Heinecke JW, Kontush A, Tall AR, Webb NR (2016) Dysfunctional HDL and atherosclerotic cardiovascular disease. Nat Rev Cardiol 13:48–60. https://doi.org/10.1038/nrcardio.2015.124
Goldberg RB, Temprosa M, Mele L, Orchard T, Mather K, Bray G, Horton E, Kitabchi A, Krakoff J, Marcovina S, Perreault L, White N (2016) Change in adiponectin explains most of the change in HDL particles induced by lifestyle intervention but not metformin treatment in the Diabetes Prevention Program. Metabolism 65:764–775. https://doi.org/10.1016/j.metabol.2015.11.011
Belalcazar LM, Lang W, Haffner SM, Hoogeveen RC, Pi-Sunyer FX, Schwenke DC, Balasubramanyam A, Tracy RP, Kriska AP, Ballantyne CM (2012) Adiponectin and the mediation of HDL-cholesterol change with improved lifestyle: the Look AHEAD Study. J Lipid Res 53:2726–2733. https://doi.org/10.1194/jlr.M030213
Funding
This work was supported by the Instituto de Salud Carlos III, Spanish Ministry of Health (co-financed by the European Regional Development Fund) PI16/00471 and PI20/00334, and by Consorcio Centro de Investigación Biomédica en Red (CIBER) (CB07/08/0016). José Luis Sánchez-Quesada is a member of the Group of Vascular Biology of the Spanish Society of Atherosclerosis.
Author information
Authors and Affiliations
Contributions
Conceptualization: Idoia Genua, Inka Miñambres, Antonio Pérez, and José Luis Sánchez-Quesada; Methodology: Idoia Genua, Inka Miñambres, and Antonio Pérez; Formal analysis: Idoia Genua and Inka Miñambres; Resources: Idoia Genua, Inka Miñambres, Helena Sardà, Rocío Puig, Sonia Fernández-Ananin, José Luis Sánchez-Quesada, and Antonio Pérez; Writing—original draft preparation: Idoia Genua and Inka Miñambres; Writing—review & editing: Idoia Genua, Inka Miñambres, Helena Sardà, Rocío Puig, Sonia Fernández-Ananin, José Luis Sánchez-Quesada, and Antonio Pérez; Supervision: Inka Miñambres, José Luis Sánchez-Quesada, and Antonio Pérez.
Corresponding authors
Ethics declarations
Disclosures
Antonio Pérez has served as a consultant for or received research support, lecture fees, or travel reimbursement from Sanofi Aventis, Almirall, Novo Nordisk, Eli Lilly, MSD, Abbott, Boehringer Ingelheim, Esteve, Gilead, Novartis, Amgen, Menarini, Amarin, Daiichi Sankyo, and Astra Zeneca. Antonio Pérez, Inka Miñambres, and José Luis Sánchez-Quesada received a grant from Instituto de Salud Carlos III, Spanish Ministry of Health (co-financed by the European Regional Development Fund) PI16/00471 and PI20/00334, and by Consorcio Centro de Investigación Biomédica en Red (CIBER) (CB07/08/0016). Sonia Fernández-Ananin has received a grant of the Catalan Society of Surgery in Research: ‘Non-absorbable running barbed suture versus non-absorbable interrupted suture in paraesophageal hernia repair. Can this surgical gesture improve the outcomes? A Multicenter Randomized Controlled Trial.’ The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. Idoia Genua, Helena Sardà, and Rocío Puig have no conflicts of interest or financial ties to disclose.
Informed consent
Written informed consent was obtained from all subjects involved in the study.
Institutional review board statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Hospital de la Santa Creu i Sant Pau research institute (protocol IIBSP-BAR-2020-157; date of approval: February 24, 2021).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Genua, I., Miñambres, I., Puig, R. et al. Weight loss benefits on HDL cholesterol persist even after weight regaining. Surg Endosc (2024). https://doi.org/10.1007/s00464-024-10826-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00464-024-10826-7