Abstract
Background
The increasing use of robotic systems for anti-reflux operations prompted this study to evaluate and compare the efficacy of robotic and Laparo-Endoscopic Single-Site (LESS) approaches.
Methods
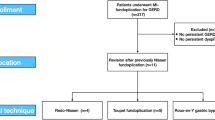
From 2012, 228 robotic fundoplication and 518 LESS fundoplication patients were prospectively followed, analyzing perioperative metrics. Data are presented as median (mean ± SD); significance at p ≤ 0.05.
Results
Patients undergoing a robotic vs. LESS fundoplication were 67 (64 ± 13.7) vs. 61 (59 ± 15.1) years-old with BMIs of 25 (25 ± 3.2) vs. 26 (25 ± 3.9) kg/m2 (p = 0.001 and 1.00, respectively). 72% of patients who underwent the robotic approach had a previous abdominal operation(s) vs 44% who underwent the LESS approach (p = 0.0001). 38% vs. 8% had a re-operative fundoplication (p = 0.0001), 59% vs. 45% had a type IV hiatal hernia (p = 0.0004). Operative duration was 160 (176 ± 76.7) vs. 130 (135 ± 50.5) min (p = 0.0001). There were 0 (robotic) vs. 5 (LESS) conversions to a different approach (p = 0.33). 5 Patients vs. 3 patients experienced postoperative complications (p = 0.06), and length of stay (LOS) was 1 (2 ± 2.6) vs. 1 (1 ± 3.2) days (p = 0.0001). Patient symptomatic dysphagia preoperatively for the robotic vs. LESS approach was scored as 2 (2.4 ± 1.9) vs. 1 (1.9 ± 1.6). Postoperatively, symptomatic dysphagia was scored as 1 (1.5 ± 1.6) vs. 1 (1.7 ± 1.7). The change in these scores was − 1 (− 1 ± 2.2) vs. 0 (− 0.5 ± 2.2) (p = 0.004).
Conclusion
Despite longer operative times and LOS in older patients, the robotic approach is efficient in undertaking very difficult operations, including patients with type IV or recurrent hiatal hernias. Furthermore, preoperative anti-reflux operations were more likely to be undertaken with the robotic approach than the LESS approach. The patient’s postoperative symptomatic dysphagia improved relatively more than after the LESS approach. The vast majority of patients who underwent the LESS approach enjoyed improved cosmesis, thus, making LESS a stronger candidate for more routine operations. Despite patient selection bias, the robotic and LESS approaches to anti-reflux operations are safe, efficacious, and should be situationally utilized.


Similar content being viewed by others
References
Luberice K, Ross S, Crespo K, De La Cruz C, Dolce J-K, Sucandy I, Rosemurgy AS (2021) Robotic complex fundoplication in patients at high-risk to fail. JSLS 25(e2020):00111. https://doi.org/10.4293/JSLS.2020.00111
Rosemurgy AS, Donn N, Paul H, Luberice K, Ross SB (2011) Gastroesophageal reflux disease. Surg Clin N Am 91:1015–1029. https://doi.org/10.1016/j.suc.2011.06.004
US Food and Drug Administration (2010) FDA drug safety communication: possible increased risk of fractures of the hip, wrist, and spine with the use of proton pump inhibitors. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/fda-drug-safety-communication-possible-increased-risk-fractures-hip-wrist-and-spine-use-proton-pump. Accessed 10 Nov 2023
Roark R, Sydor M, Chatila AT, Umar S, Guerra RDL, Bilal M, Guturu P (2020) Management of gastroesophageal reflux disease. Dis Mon 66:100849. https://doi.org/10.1016/j.disamonth.2019.02.002
Dean BB, Gano AD, Knight K, Ofman JJ, Fass R (2004) Effectiveness of proton pump inhibitors in nonerosive reflux disease. Clin Gastroenterol Hepatol 2:656–664. https://doi.org/10.1016/S1542-3565(04)00288-5
Mikami DJ, Murayama KM (2015) Physiology and pathogenesis of gastroesophageal reflux disease. Surg Clin N Am 95:515–525. https://doi.org/10.1016/j.suc.2015.02.006
Rosemurgy A, Wilfong C, Craigg D, Co F, Sucandy I, Ross S (2019) The evolving landscape of esophageal cancer: a four-decade analysis. Am Surg 85:944–948
Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Lombard R (1991) Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc 1:138–143
Ross S, Roddenbery A, Luberice K, Paul H, Farrior T, Vice M, Patel K, Rosemurgy A (2013) Laparoendoscopic single site (LESS) vs. conventional laparoscopic fundoplication for GERD: is there a difference? Surg Endosc 27:538–547. https://doi.org/10.1007/s00464-012-2476-0
Salminen PTP, Hiekkanen HI, Rantala APT, Ovaska JT (2007) Comparison of long-term outcome of laparoscopic and conventional Nissen fundoplication: a prospective randomized study with an 11-year follow-up. Ann Surg 246:201–206. https://doi.org/10.1097/01.sla.0000263508.53334.af
Cowgill SM, Gillman R, Kraemer E, Al-Saadi S, Villadolid D, Rosemurgy A (2007) Ten-year follow up after laparoscopic Nissen fundoplication for gastroesophageal reflux disease. Am Surg 73:748–752; discussion 752–753
Giovannetti A, Craigg D, Castro M, Ross S, Sucandy I, Rosemurgy A (2019) Laparoendoscopic single-site (LESS) versus robotic “redo” hiatal hernia repair with fundoplication: which approach is better? Am Surg 85:978–984
Sukharamwala P, Teta A, Ross S, Co F, Alvarez-Calderon G, Luberice K, Rosemurgy A (2015) Over 250 laparoendoscopic single site (LESS) fundoplications: lessons learned. Am Surg 81:870–875
Dallemagne B, Arenas Sanchez M, Francart D, Perretta S, Weerts J, Markiewicz S, Jehaes C (2011) Long-term results after laparoscopic reoperation for failed antireflux procedures. Br J Surg 98:1581–1587. https://doi.org/10.1002/bjs.7590
Turkcapar A, Kepenekci I, Mahmoud H, Tuzuner A (2007) Laparoscopic fundoplication with prosthetic hiatal closure. World J Surg 31:2169–2176. https://doi.org/10.1007/s00268-007-9066-7
Humphries LA, Hernandez JM, Clark W, Luberice K, Ross SB, Rosemurgy AS (2013) Causes of dissatisfaction after laparoscopic fundoplication: the impact of new symptoms, recurrent symptoms, and the patient experience. Surg Endosc 27:1537–1545. https://doi.org/10.1007/s00464-012-2611-y
D’Alessio MJ, Rakita S, Bloomston M, Chambers CM, Zervos EE, Goldin SB, Poklepovic J, Boyce HW, Rosemurgy AS (2005) Esophagography predicts favorable outcomes after laparoscopic Nissen fundoplication for patients with esophageal dysmotility. J Am Coll Surg 201:335–342. https://doi.org/10.1016/j.jamcollsurg.2005.04.036
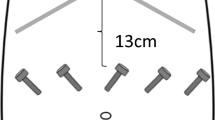
Rosemurgy AS, Downs D, Swaid F, Ross SB (2016) Laparo-Endoscopic Single-Site (LESS) Nissen fundoplication: how we do it. J Gastrointest Surg 20:2093–2099. https://doi.org/10.1007/s11605-016-3290-0
Rosemurgy A, Bourdeau T, Luberice K, Sucandy I, Ross S (2022) Robot application for hepatopancreatic disorders, gastroesophageal reflux disease, and achalasia. Am Surg 88:507–511. https://doi.org/10.1177/0003134820952388
Arcerito M, Changchien E, Falcon M, Parga MA, Bernal O, Moon JT (2018) Robotic fundoplication for gastroesophageal reflux disease and hiatal hernia: initial experience and outcome. Am Surg 84:1945–1950
Tolboom RC, Draaisma WA, Broeders IAMJ (2016) Evaluation of conventional laparoscopic versus robot-assisted laparoscopic redo hiatal hernia and antireflux surgery: a cohort study. J Robot Surg 10:33–39. https://doi.org/10.1007/s11701-016-0558-z
Markar SR, Karthikesalingam AP, Hagen ME, Talamini M, Horgan S, Wagner OJ (2010) Robotic vs. laparoscopic Nissen fundoplication for gastro-oesophageal reflux disease: systematic review and meta-analysis. Int J Med Robot Comput Assist Surg. https://doi.org/10.1002/rcs.309
McKinley SK, Dirks RC, Walsh D, Hollands C, Arthur LE, Rodriguez N, Jhang J, Abou-Setta A, Pryor A, Stefanidis D, Slater BJ (2021) Surgical treatment of GERD: systematic review and meta-analysis. Surg Endosc 35:4095–4123. https://doi.org/10.1007/s00464-021-08358-5
Papasavas PK, Keenan RJ, Yeaney WW, Caushaj PF, Gagné DJ, Landreneau RJ (2003) Effectiveness of laparoscopic fundoplication in relieving the symptoms of gastroesophageal reflux disease (GERD) and eliminating antireflux medical therapy. Surg Endosc 17:1200–1205. https://doi.org/10.1007/s00464-002-8910-y24
Felder SI, Ramanathan R, Russo AE, Jimenez-Rodriguez RM, Hogg ME, Zureikat AH, Strong VE, Zeh HJ, Weiser MR (2018) Robotic gastrointestinal surgery. Curr Probl Surg 55:198–246. https://doi.org/10.1067/j.cpsurg.2018.07.001
Ryan CE, Ross SB, Sukharamwala PB, Sadowitz BD, Wood TW, Rosemurgy AS (2015) Distal pancreatectomy and splenectomy: a robotic or LESS approach. JSLS 19(e2014):00246. https://doi.org/10.4293/JSLS.2014.00246
Sfara A, Dumitrascu DL (2019) The management of hiatal hernia: an update on diagnosis and treatment. Med Pharm Rep 92:321–325. https://doi.org/10.15386/mpr-1323
Frazzoni M, Conigliaro R, Colli G, Melotti G (2012) Conventional versus robot-assisted laparoscopic Nissen fundoplication: a comparison of postoperative acid reflux parameters. Surg Endosc 26:1675–1681. https://doi.org/10.1007/s00464-011-2091-5
Owen B, Simorov A, Siref A, Shostrom V, Oleynikov D (2014) How does robotic anti-reflux surgery compare with traditional open and laparoscopic techniques: a cost and outcomes analysis. Surg Endosc 28:1686–1690. https://doi.org/10.1007/s00464-013-3372-y
Müller-Stich BP, Reiter MA, Wente MN, Bintintan VV, Köninger J, Büchler MW, Gutt CN (2007) Robot-assisted versus conventional laparoscopic fundoplication: short-term outcome of a pilot randomized controlled trial. Surg Endosc 21:1800–1805. https://doi.org/10.1007/s00464-007-9268-y
Braumann C, Jacobi CA, Menenakos C, Ismail M, Rueckert JC, Mueller JM (2008) Robotic-assisted laparoscopic and thoracoscopic surgery with the Da Vinci system: a 4-year experience in a single institution. Surg Laparosc Endosc Percutan Tech 18:260–266. https://doi.org/10.1097/SLE.0b013e31816f85e5
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Sharona B. Ross is a consultant for Intuitive Surgical (Sunnyvale, CA) and Ethicon. Sharona B. Ross receives educational grants for her Women in Surgery Career Symposium from Intuitive Surgical and Medtronic (Minneapolis, MN). Iswanto Sucandy, Michael Trotto, Maria Christodoulou, Tara M. Pattilachan, Jenna Jattan, and Alexander S. Rosemurgy have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ross, S.B., Sucandy, I., Trotto, M. et al. A decade of experience with minimally invasive anti-reflux operations: robot vs. LESS. Surg Endosc 38, 2641–2648 (2024). https://doi.org/10.1007/s00464-024-10771-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10771-5