Abstract
Objective
This study aimed to evaluate the clinical application and efficacy of a super-low-positioned intestinal decompression tube in the treatment of intestinal obstruction.
Methods
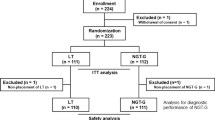
A total of 130 patients with postoperative small bowel obstruction were included in this study. The patients were divided into a super-low-positioned intestinal decompression group and a conventional intestinal decompression group. The clinical data, treatment outcomes, and complications were compared between the two groups.
Results
The technical success rate of placing the super-low-positioned intestinal decompression tube was 100%, with no intraoperative complications. The patients in the super-low-positioned intestinal decompression group had a significantly shorter hospital stay (8.3 ± 5.2 vs 17.7 ± 13.3, P < 0.001) and a higher non-operative treatment success rate (83.6% vs 57.9%, P = 0.001) compared to the conventional intestinal decompression group. Multivariate logistic regression analysis showed that the placement of a super-low-positioned intestinal decompression tube was an independent protective factor for treatment outcomes (P = 0.001). The hospital stay was significantly shorter in the super-low-positioned intestinal decompression group compared to the conventional group in both successful non-operative treatment patients (6.9 ± 3.0 vs 11.2 ± 7.5, P < 0.001) and failed non-operative treatment patients (16.2 ± 7.4 vs 26.6 ± 14.4, P < 0.001). The super-low-positioned intestinal decompression tube effectively relieved the “Self-strangulation” phenomenon in patients with intestinal obstruction.
Conclusion
The super-low-positioned intestinal decompression tube is a safe and effective method for the treatment of intestinal obstruction, with better treatment outcomes and shorter hospital stays compared to conventional intestinal decompression. Further prospective studies are needed to validate these findings.



Similar content being viewed by others
References
Guo SB, Duan ZJ (2012) Decompression of the small bowel by endoscopic long-tube placement. World J Gastroenterol 18(15):1822–1826. https://doi.org/10.3748/wjg.v18.i15.1822
Gowen GF (2007) Rapid resolution of small-bowel obstruction with the long tube, endoscopically advanced into the jejunum. Am J Surg 193(2):184–189. https://doi.org/10.1016/j.amjsurg.2006.11.005
Li M, Ren J, Zhu W et al (2015) Long intestinal tube splinting really prevents recurrence of postoperative adhesive small bowel obstruction: a study of 1,071 cases. Am J Surg 209(2):289–296. https://doi.org/10.1016/j.amjsurg.2013.10.027
Ten Broek RPG, Krielen P, Di Saverio S et al (2018) Bologna guidelines for diagnosis and management of adhesive small bowel obstruction (ASBO): 2017 update of the evidence-based guidelines from the world society of emergency surgery ASBO working group. World J Emerg Surg 13:24. https://doi.org/10.1186/s13017-018-0185-2
Klingbeil KD, Wu JX, Osuna-Garcia A et al (2023) Management of small bowel obstruction and systematic review of treatment without nasogastric tube decompression. Surg Open Sci 12:62–67. https://doi.org/10.1016/j.sopen.2022.10.002
Maung AA, Johnson DC, Piper GL et al (2012) Evaluation and management of small-bowel obstruction: an Eastern Association for the Surgery of Trauma practice management guideline. J Trauma Acute Care Surg 73(5 Suppl 4):S362–S369. https://doi.org/10.1097/TA.0b013e31827019de
Sekiba K, Ohmae T, Odawara N et al (2016) A new method for insertion of long intestinal tube for small bowel obstruction: nonendoscopic over-the-wire method via short nasogastric tube. Medicine (Baltimore) 95(47):e5449. https://doi.org/10.1097/MD.0000000000005449
Wang ZW, Li XG, Pan J et al (2015) Placement of a long intestinal tube in patients with early postoperative small bowel obstruction under fluoroscopic guidance. Chin Med Sci J 30(3):156–161. https://doi.org/10.1016/s1001-9294(15)30040-7
Acknowledgements
This study was completed by all authors.
Funding
Sponsored by Fujian provincial social development science and technology guiding project (Grant No. 2022Y01010238).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Sun-Jian Wang, Yun-Jing Xue, Li-Lan She, Yu Xia, and Ju-Li Lin have no conflict of interest or financial ties to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, SJ., Xue, YJ., She, LL. et al. Clinical application of super-low-positioned intestinal decompression tube in the treatment of intestinal obstruction: a pilot study. Surg Endosc 38, 880–887 (2024). https://doi.org/10.1007/s00464-023-10639-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10639-0