Abstract
Introduction
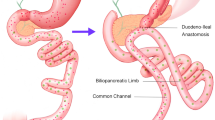
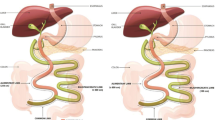
Most surgeons who perform single-anastomosis duodeno-ileal switches (SADI-S) use a pre-determined common channel length without measuring total bowel length (TBL). However, TBL varies between patients, and a standardized common channel length could contribute to malabsorptive complications and reoperations following SADI-S. The purpose of this study was to determine whether using a TBL measurement protocol to individualize common channel length would be associated with reduced reoperations and complications.
Methods
A prospectively maintained data registry was retrospectively reviewed to identify all patients who underwent SADI-S between September 2017 and February 2022. In April 2021, we began using TBL measurements during SADI-S with 40% of the TBL used as the length for the common channel. Outcomes pre-TBL and post-TBL measurement protocol were compared.
Results
A total of 119 SADI-S recipients (59 pre-TBL; 60 post-TBL) were included. The pre-TBL group had a higher frequency of reoperations (23.7% vs 1.7%, p < 0.001) and late complications (29.3% vs 3.3%, p < 0.001). The mean time to reoperation was 13.7 months in the pre-TBL group and 6.7 months in the post-TBL group (p = 0.347). Patients in the post-TBL group had significantly higher serum albumin levels at 3 months (4.2 g/dL vs 3.5 g/dL, p < 0.001), 6 months (4.1 g/dL vs 3.6 g/dL, p < 0.001), and 12 months (4.2 g/dL vs 3.8 g/dL, p = 0.023) postoperatively when compared to the pre-TBL group.
Conclusion
Using TBL measurements to individualize common channel length was associated with a significant reduction in reoperations and late complications following SADI-S.

Similar content being viewed by others
References
Centers for Disease Control and Prevention (2022) Adult obesity facts. https://www.cdc.gov/obesity/data/adult.html#print. Accessed 27 Feb 2023
Cosentino C, Marchetti C, Monami M, Mannucci E, Cresci B (2021) Efficacy and effects of bariatric surgery in the treatment of obesity: network meta-analysis of randomized controlled trials. Nutr Metab Cardiovasc Dis 31(10):2815–2824
Wang L, Lin M, Yu J et al (2021) The impact of bariatric surgery versus non-surgical treatment on blood pressure: systematic review and meta-analysis. Obes Surg 31(11):4970–4984
Khorgami Z, Shoar S, Saber AA et al (2019) Outcomes of bariatric surgery versus medical management for type 2 diabetes mellitus: a meta-analysis of randomized controlled trials. Obes Surg 29(3):964–974
Susstrunk J, Schneider R, Peterli R et al (2023) Long-term outcome after biliopancreatic diversion with duodenal switch: a single-center experience with up to 20 years follow-up. Surg Obes Relat Dis 19(2):83–90
Anthone GJ, Lord RV, DeMeester TR, Crookes PF (2003) The duodenal switch operation for the treatment of morbid obesity. Ann Surg 238(4):618–27 (discussion 627–8)
Fenaroli P, Piazzalunga D, Guffanti Pesenti G, Cassinelli G (1993) Surgical treatment of major obesity by biliopancreatic bypass: our experience. J Chir (Paris) 130(3):125–9
Hess DS, Hess DW (1998) Biliopancreatic diversion with a duodenal switch. Obes Surg 8(3):267–282
Prachand VN, Davee RT, Alverdy JC (2006) Duodenal switch provides superior weight loss in the super-obese (BMI > or =50 kg/m2) compared with gastric bypass. Ann Surg 244(4):611–619
Scopinaro N, Marinari GM, Camerini GB, Papadia FS, Adami GF (2005) Specific effects of biliopancreatic diversion on the major components of metabolic syndrome: a long-term follow-up study. Diabetes Care 28(10):2406–2411
Topart P, Becouarn G, Delarue J (2017) Weight loss and nutritional outcomes 10 years after biliopancreatic diversion with duodenal switch. Obes Surg 27(7):1645–1650
Sanchez-Pernaute A, Rubio Herrera MA, Perez-Aguirre E et al (2007) Proximal duodenal-ileal end-to-side bypass with sleeve gastrectomy: proposed technique. Obes Surg 17(12):1614–1618
Sanchez-Pernaute A, Herrera MA, Perez-Aguirre ME et al (2010) Single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). One to three-year follow-up Obes Surg 20(12):1720–1726
Topart P, Becouarn G (2017) The single anastomosis duodenal switch modifications: a review of the current literature on outcomes. Surg Obes Relat Dis 13(8):1306–1312
Spinos D, Skarentzos K, Esagian SM, Seymour KA, Economopoulos KP (2021) The effectiveness of single-anastomosis duodenoileal bypass with sleeve gastrectomy/one anastomosis duodenal switch (SADI-S/OADS): an updated systematic review. Obes Surg 31(4):1790–1800
Cottam D, Roslin M, Enochs P et al (2020) Single anastomosis duodenal switch: 1-year outcomes. Obes Surg 30(4):1506–1514
Gebelli JP, Lazzara C, de Gordejuela AGR et al (2022) Duodenal switch vs. single-anastomosis duodenal switch (SADI-S) for the treatment of grade iv obesity: 5-year outcomes of a multicenter prospective cohort comparative study. Obes Surg 32(12):3839–3846
Tacchino RM (2015) Bowel length: measurement, predictors, and impact on bariatric and metabolic surgery. Surg Obes Relat Dis 11(2):328–334
Marie L, Nacache R, Scemama U et al (2018) Preoperative prediction of small bowel length using CT scan and tridimensional reconstructions: a new tool in bariatric surgery? Obes Surg 28(5):1217–1224
Teitelbaum EN, Vaziri K, Zettervall S, Amdur RL, Orkin BA (2013) Intraoperative small bowel length measurements and analysis of demographic predictors of increased length. Clin Anat 26(7):827–832
Hess DS, Hess DW, Oakley RS (2005) The biliopancreatic diversion with the duodenal switch: results beyond 10 years. Obes Surg 15(3):408–416
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
McLean C, Mocanu V, Birch DW, Karmali S, Switzer NJ (2021) Hypoalbuminemia predicts serious complications following elective bariatric surgery. Obes Surg 31(10):4519–4527
McConnell Donald B, O’Rourke Robert W, Deveney Clifford W (2005) Common channel length predicts outcomes of biliopancreatic diversion alone and with the duodenal switch surgery. Am J Surg 189(5):536–540 (discussion 540)
Ortiz-Zuniga AM, Costa Forner P, Cirera de Tudela A et al (2022) The impact of the length of the common intestinal loop on metabolic and nutritional outcomes of patients with severe obesity who undergo of single anastomosis duodeno-ileal bypass with sleeve gastrectomy: 5-year follow-up. J Laparoendosc Adv Surg Tech A 32(9):955–961
Surve A, Cottam D, Medlin W et al (2020) Long-term outcomes of primary single-anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S). Surg Obes Relat Dis 16(11):1638–1646
Cottam D, Cottam S, Surve A (2021) Single-anastomosis duodenal ileostomy with sleeve gastrectomy “continued innovation of the duodenal switch”. Surg Clin N Am 101(2):189–198
Author information
Authors and Affiliations
Contributions
All authors listed above contributed to this manuscript and meet the requirements of appropriate authorship as defined by the International Committee of Medical Journal Editors (ICMJE).
Corresponding author
Ethics declarations
Disclosures
Daniel Davis is a consultant for Intuitive Surgical Inc. Lucas Fair, Anthony Waddimba, Phillip Strothman, Darby Dwyer, Priscilla Anderton, Anella Bittle, Gerald Ogola, and Steven Leeds have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fair, L., Waddimba, A.C., Strothman, P. et al. The use of a total bowel length measurement protocol may reduce reoperations and complications after single-anastomosis duodenal switch. Surg Endosc 37, 9310–9317 (2023). https://doi.org/10.1007/s00464-023-10505-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10505-z