Abstract
Background
While well-established protocols direct laparoscopic training, there remains a relative paucity of guidelines for robotic education. Furthermore, it is unknown how exposure to one platform influences trainees’ proficiency in the other. This study aimed to compare and quantify (1) learning curves and (2) transference of skill between the two modalities in novice learners.
Methods
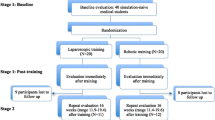
Thirty pre-clinical medical students were randomized into two groups. One group performed the peg-transfer task using the robot first, followed by laparoscopy, while the other group performed the same task laparoscopically first. Participants completed five repetitions with each methodology. Participants were timed and errors were recorded. We hypothesized that laparoscopic experience with the peg-transfer task would assist in completing the task robotically, and there would be a higher degree of skill transference from the laparoscopic to robotic platform.
Results
Peg-transfer task completion was consistently faster and more accurate with the robot compared to laparoscopy (p < 0.01). We observed a positive transference of skill from the laparoscopic to robotic platform. However, exposure to the robot-hindered students’ ability to perform the task laparoscopically, evidenced by significantly increased time and errors when compared with baseline laparoscopic performance (p < 0.01).
Conclusion
These findings encourage surgical residency programs to treat robotic and laparoscopic training as discrete entities and consider their unique learning curves and skill transference when designing an efficient curriculum. While these effects are observed in novices, future directions include uncovering the trends among resident trainees and practicing surgeons.




Similar content being viewed by others
References
Henderson L et al (2018) Outcomes during a transition period from open to laparoscopic pyloromytomy. J Laparoendosc Adv Surg Tech A 28(4):481–485
Peng C et al (2016) Safety outcomes of NOTES cholecystectomy versus laparoscopic cholecystectomy: a systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech 26(5):347–353
Wee IJY et al (2020) A systematic review of the true benefit of robotic surgery: ergonomics. Int J Med Robot 16(4):e2113
Li X et al (2017) The safety and effectiveness of robot-assisted versus laparoscopic TME in patients with rectal cancer: a meta-analysis and systematic review. Medicine (Baltimore) 96(29):e7585
Diana M, Marescaux J (2015) Robotic surgery. Br J Surg 102(2):e15–e28
Vasudevan V et al (2016) Clinical outcomes and cost-benefit analysis comparing laparoscopic and robotic colorectal surgeries. Surg Endosc 30(12):5490–5493
Narula V et al (2007) A computerized analysis of robotic versus laparoscopic task performance. Surg Endosc 21:2258
Obek C et al (2005) Robotic versus conventional laparoscopic skill acquisition: implications for training. J Endourol 19(9):1098–1103
Chen R et al (2020) A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg Endosc 34(1):361–367
Ruaidhri M et al (2016) Baseline laparoscopic skill may predict baseline robotic skill and early robotic surgery learning curve. J Endourol 30(5):588–592
Kilic GS et al (2012) Effect of residents’ previous laparoscopic surgery experience on initial robotic suturing experience. ISRN Obstet Gynecol 2012:569456
Pio L et al (2020) Learning curve for robotic surgery in children: a systematic review of outcomes and fellowship programs. J Robot Surg 14(4):531–541
Heemskerk J et al (2007) Learning curves of robot-assisted laparoscopic surgery compared with conventional laparoscopic surgery: an experimental study evaluating skill acquisition of robot-assisted laparoscopic tasks compared with conventional laparoscopic tasks in inexperienced users. Surg Laparosc Endosc Percutan Tech 17(3):171–174
Vidovszky TJ et al (2006) Robotic cholecystectomy: learning curve, advantages, and limitations. J Surg Res 136(2):172–178
Guend H et al (2017) Developing a robotic colorectal cancer surgery program: understanding institutional and individual learning curves. Surg Endosc 31(7):2820–2828
Lovegrove CE et al (2017) Training modalities in robot-assisted urologic surgery: a systematic review. Eur Urol Focus 3(1):102–116
Pilka R et al (2017) Laparoscopic and robotic sacropexy: retrospective review of learning curve experiences and follow-up. Ceska Gynekol 82(4):261–267
Chang L et al (2003) Robotic surgery: identifying the learning curve through objective measurement of skill. Surg Endosc Other Interv Tech 17(11):1744–1748
Howard JM (2021) Robotic, laparoscopic, and open radical prostatectomy—is the jury still out? JAMA Netw Open 4(8):e2120693
Chahal B et al (2022) Transfer of open and laparoscopic skills to robotic surgery: a systematic review. J Robot Surg. https://doi.org/10.1007/s11701-022-01492-9
Moit H et al (2019) A standardized robotic training curriculum in a general surgery program. JSLS 23(4):e2019.00045
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Xiaodong Chen has Research Support from Intuitive Robotics. Kristen M. Quinn, Claire Griffiths, Grace Chen, Sylvester Osayi, and Syed Husain have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Quinn, K.M., Chen, X., Griffiths, C. et al. Skill transference and learning curves in novice learners: a randomized comparison of robotic and laparoscopic platforms. Surg Endosc 37, 8483–8488 (2023). https://doi.org/10.1007/s00464-023-10486-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10486-z