Abstract
Background
Laparoscopic cholecystectomy with common bile duct exploration (LCBDE) is equivalent in safety and efficacy to endoscopic retrograde cholangiopancreatography (ERCP) plus laparoscopic cholecystectomy (LC) while decreasing number of procedures and length of stay (LOS). Despite these advantages LCBDE is infrequently utilized. We hypothesized that formal, simulation-based training in LCBDE would result in increased utilization and improve patient outcomes across participating institutions.
Methods
Data was obtained from an on-going multi-center study in which simulator-based transcystic LCBDE training curricula were instituted for attending surgeons and residents. A 2-year retrospective review of LCBDE utilization prior to LCBDE training was compared to utilization up to 2 years after initiation of training. Patient outcomes were analyzed between LCBDE strategy and ERCP strategy groups using χ2, t tests, and Wilcoxon rank tests.
Results
A total of 50 attendings and 70 residents trained in LCBDE since November 2020. Initial LCBDE utilization rate ranged from 0.74 to 4.5%, and increased among all institutions after training, ranging from 9.3 to 41.4% of cases. There were 393 choledocholithiasis patients analyzed using LCBDE (N = 129) and ERCP (N = 264) strategies. The LCBDE group had shorter median LOS (3 days vs. 4 days, p < 0.0001). No significant differences in readmission rates between LCBDE and ERCP groups (4.7% vs. 7.2%, p = 0.33), or in post-procedure pancreatitis (0.8% v 0.8%, p > 0.98). In comparison to LCBDE, the ERCP group had higher rates of bile duct injury (0% v 3.8%, p = 0.034) and fluid collections requiring intervention (0.8% v 6.8%, p < 0.009) secondary to cholecystectomy complications. Laparoscopic antegrade balloon sphincteroplasty had the highest technical success rate (87%), followed by choledochoscopic techniques (64%).
Conclusion
Simulator-based training in LCBDE results in higher utilization rates, shorter LOS, and comparable safety to ERCP plus cholecystectomy. Therefore, implementation of LCBDE training is strongly recommended to optimize healthcare utilization and management of patients with choledocholithiasis.







Similar content being viewed by others
References
Lyu Y, Cheng Y, Li T, Cheng B, Jin X (2019) Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc 33(10):3275–3286. https://doi.org/10.1007/s00464-018-06613-w
Bosley ME, Zamora IJ, Neff LP (2021) Choledocholithiasis-a new clinical pathway. Transl Gastroenterol Hepatol 6:35. https://doi.org/10.21037/tgh-20-172
Wandling MW, Hungness ES, Pavey ES, Stulberg JJ, Schwab B, Yang AD, Shapiro MB, Bilimoria KY, Ko CY, Nathens AB (2016) Nationwide assessment of trends in choledocholithiasis management in the United States from 1998 to 2013. JAMA Surg 151(12):1125–1130. https://doi.org/10.1001/jamasurg.2016.2059
Bell RH Jr, Biester TW, Tabuenca A, Rhodes RS, Cofer JB, Britt LD, Lewis FR Jr (2009) Operative experience of residents in US general surgery programs: a gap between expectation and experience. Ann Surg 249(5):719–724. https://doi.org/10.1097/SLA.0b013e3181a38e59
Dawe SR, Pena GN, Windsor JA, Broeders JA, Cregan PC, Hewett PJ, Maddern GJ (2014) Systematic review of skills transfer after surgical simulation-based training. Br J Surg 101(9):1063–1076. https://doi.org/10.1002/bjs.9482
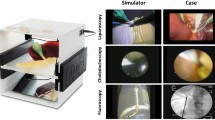
Santos BF, Reif TJ, Soper NJ, Nagle AP, Rooney DM, Hungness ES (2012) Development and evaluation of a laparoscopic common bile duct exploration simulator and procedural rating scale. Surg Endosc 26(9):2403–2415. https://doi.org/10.1007/s00464-012-2213-8
Teitelbaum EN, Soper NJ, Santos BF, Rooney DM, Patel P, Nagle AP, Hungness ES (2014) A simulator-based resident curriculum for laparoscopic common bile duct exploration. Surgery 156(4):880–887. https://doi.org/10.1016/j.surg.2014.06.020
Kemp Bohan PM, Connelly CR, Crawford J, Bronson NW, Schreiber MA, Lucius CW, Hunter JG, Kiraly LN, Ham B (2017) Early analysis of laparoscopic common bile duct exploration simulation. Am J Surg 213(5):888–894. https://doi.org/10.1016/j.amjsurg.2017.03.011
Schwab B, Teitelbaum EN, Barsuk JH, Soper NJ, Hungness ES (2018) Single-stage laparoscopic management of choledocholithiasis: an analysis after implementation of a mastery learning resident curriculum. Surgery 163(3):503–508. https://doi.org/10.1016/j.surg.2017.10.006
Nyren MQ, Filiberto AC, Underwood PW, Abbott KL, Balch JA, Efron PA, George BC, Shickel B, Upchurch GR Jr, Sarosi GA Jr, Loftus TJ (2023) A simulation curriculum for laparoscopic common bile duct exploration, balloon sphincterotomy, and endobiliary stenting: associations with resident performance and autonomy in the operating room. Surgery 173(4):950–956. https://doi.org/10.1016/j.surg.2022.11.007
Rosser J, Hungness ES, Teitelbaum E, Santos BF, Vazquez R, Schwab B, Berci G, Fanelli RD (2018) Transcystic common bile duct exploration. Stealth Learning Company. https://books.apple.com/us/book/transcystic-common-bile-duct-exploration/id1447754319
Campagna RAJ, Belette AM, Holmstrom AL, Halverson AL, Santos BF, Hungness ES, Teitelbaum EN (2021) Addressing the gap in laparoscopic common bile duct exploration training for rural surgeons: imparting procedural ability is not enough. Surg Endosc 35(9):5140–5146. https://doi.org/10.1007/s00464-020-08003-7
Navaratne L, Martinez IA (2021) Transductal versus transcystic laparoscopic common bile duct exploration: an institutional review of over four hundred cases. Surg Endosc 35(1):437–448. https://doi.org/10.1007/s00464-020-07522-7
Reinders JSK, Gouma DJ, Ubbink DT, van Ramshorst B, Boerma D (2014) Transcystic or transductal stone extraction during single-stage treatment of choledochocystolithiasis: a systematic review. World J Surg 38(9):2403–2411. https://doi.org/10.1007/s00268-014-2537-8
Bekheit M, Smith R, Ramsay G, Soggiu F, Ghazanfar M, Ahmed I (2019) Meta-analysis of laparoscopic transcystic versus transcholedochal common bile duct exploration for choledocholithiasis. BJS Open 3(3):242–251. https://doi.org/10.1002/bjs5.50132
Zhu J, Wang G, Xie B, Jiang Z, Xiao W, Li Y (2023) Minimally invasive management of concomitant gallstones and common bile duct stones: an updated network meta-analysis of randomized controlled trials. Surg Endosc 37(3):1683–1693. https://doi.org/10.1007/s00464-022-09723-8
Funding
Boston Scientific provided grant funding and educational equipment for teaching LCBDE [ISREND00116].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr Michael Ujiki is a scientific advisory board member of Boston Scientific and Apollo, and receives payment lectures from Medtronic, and Gore. Dr. B. Fernando Santos is a consultant for Boston Scientific and is entitled to shared royalties as a co-inventor of the 3D-Med LCBDE simulator. Dr. Edward Auyang is a consultant for Boston Scientific. Dr. Edward Jones is a consultant for Boston Scientfic. Drs. Vanesa N. VanDruff, Eugene P. Ceppa, Wendy Li, Brian Davis, Danielle Abbitt, Michael Cutshall, Casey Lamb, Robin Cotter, Xavier Fowler, Ming Cai, Jenaya Goldwag, Julia R. Amundson, Stephanie Joseph, Simon Che, Michael McCormack, H. Mason Hedberg, and Kristine Kuchta have no financial interests or conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript was accepted for an oral presentation at the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) in Montreal, Quebec, Canada on March 29-April 2, 2023.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
VanDruff, V.N., Santos, B.F., Kuchta, K. et al. The Laparoscopy in Biliary Exploration Research and Training Initiative (LIBERTI) trial: simulator-based training for laparoscopic management of choledocholithiasis. Surg Endosc 38, 931–941 (2024). https://doi.org/10.1007/s00464-023-10480-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10480-5