Abstract
Background
Patients with cT1-2 colon cancer (CC) have a 10–20% risk of lymph node metastases. Sentinel lymph node identification (SLNi) could improve staging and reduce morbidity in future organ-preserving CC surgery. This pilot study aimed to assess safety and feasibility of robot-assisted fluorescence-guided SLNi using submucosally injected indocyanine green (ICG) in patients with cT1-2N0M0 CC.
Methods
Ten consecutive patients with cT1-2N0M0 CC were included in this prospective feasibility study. Intraoperative submucosal, peritumoral injection of ICG was performed during a colonoscopy. Subsequently, the near-infrared fluorescence ‘Firefly’ mode of the da Vinci Xi robotic surgical system was used for SLNi. SLNs were marked with a suture, after which a segmental colectomy was performed. The SLN was postoperatively ultrastaged using serial slicing and immunohistochemistry, in addition to the standard pathological examination of the specimen. Colonoscopy time, detection time (time from ICG injection to first SLNi), and total SLNi time were measured (time from the start of colonoscopy to start of segmental resection). Intraoperative, postoperative, and pathological outcomes were registered.
Results
In all patients, at least one SLN was identified (mean 2.3 SLNs, SLN diameter range 1–13 mm). No tracer-related adverse events were noted. Median colonoscopy time was 12 min, detection time was 6 min, and total SLNi time was 30.5 min. Two patients had lymph node metastases present in the SLN, and there were no patients with false negative SLNs. No patient was upstaged due to ultrastaging of the SLN after an initial negative standard pathological examination. Half of the patients unexpectedly had pT3 tumours.
Conclusions
Robot-assisted fluorescence-guided SLNi using submucosally injected ICG in ten patients with cT1-2N0M0 CC was safe and feasible. SLNi was performed in an acceptable timespan and SLNs down to 1 mm were detected. All lymph node metastases would have been detected if SLN biopsy had been performed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Colorectal cancer is the 3rd most common malignancy in the Netherlands and the second leading cause of cancer-related deaths [1, 2]. More local excisions and polypectomies are performed due to an increased incidence of T1-2 tumours following population screening for colorectal cancer [3]. However, local excisions are limited by the inability to assess lymph node status, which is one of the most important reasons for secondary surgery and adjuvant chemotherapy. Although the risk of lymph node metastases is relatively low, namely 10–20% in pT1-2 colon cancer (CC) [4, 5], segmental resections are routinely performed. However, segmental resections result in substantial morbidity [6], mortality (2.4–3.1%) [6,7,8], hospitalisation [6], and reduction in quality of life (e.g., as a consequence of stomas) [9, 10]. Another drawback is that up to 20% of patients with stage I and II CC still develop recurrent disease or distant metastases despite radical segmental resection [11,12,13], which could result from insufficient sensitivity of conventional histopathological examination for (micro)metastases [12, 14].
Sentinel lymph node (SLN) biopsy combined with local treatment of early-stage CC could potentially be sufficient for therapy and staging, resulting in reduced morbidity due to organ-preserving surgery [15, 16]. Furthermore, SLN biopsy has been proposed to improve detection of lymph node metastases, due to ultrastaging techniques [12, 14]. Several studies regarding SLN identification (SLNi) in CC have been published. Although the technique might be applicable in clinical practice, relatively low sensitivity rates were found, varying between 70 and 76% with subsequent high rates of false negatives [17,18,19]. However, it is suggested that using near-infrared fluorescence (NIRF), optimising the tracer injection method, and patient selection could improve the outcomes of SLNi [20]. Especially SLNi in patients with cT1-2 tumours after submucosal peritumoral tracer injection might lead to a better sensitivity [20]. Furthermore, we hypothesised that the stable, magnified 3D view of the da Vinci Xi could improve identification of SLNs. This pilot study aimed to assess safety and feasibility of robot-assisted fluorescence-guided SLNi in ten patients with cT1-2N0 CC using intraoperative submucosal injection of indocyanine green (ICG).
Materials and methods
Study design
This prospective pilot study assessed safety and feasibility of robot-assisted SLNi using submucosal, peritumoral injection of ICG in patients with cT1-2N0M0 CC. After SLNi, segmental colon resection was performed according to standard of care.
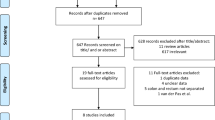
Ten consecutive patients were identified from multidisciplinary team meetings at the large teaching hospital Meander Medical Center (the Netherlands). Preoperative work-up included colonoscopy (with biopsy) and thoracoabdominal computed tomography according to current guidelines [21]. The study was approved by the local medical ethics committee (MEC-U, Nieuwegein, the Netherlands, NL71065.100.19) and registered at https://trialsearch.who.int/ (formerly registered at www.trialregister.nl, NL8901) before inclusion of the first patient.
Patient population
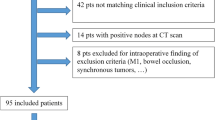
Eligibility criteria for participation were: (1) cT1-2N0M0 colon cancer, (2) age ≥ 18 years, (3) and provided oral and written informed consent. Exclusion criteria were: (1) prior local excision of the tumour, (2) suspicion of lymph node or distant metastases, (3) contraindication for robot-assisted surgery or the use of ICG (i.e., iodine allergy, severe kidney or liver failure, hyperthyroidism or an autonomously functioning thyroid adenoma), (4) pregnancy and lactation, (5) a tumour too large to pass endoscopically, (6) and metastatic disease or T4 tumour discovered during intraoperative staging. Patients underwent mechanical bowel preparation according to local hospital protocol for the intraoperative colonoscopy.
Outcomes
The primary outcomes were: (1) SLNi rate (defined as the number of patients with one or more SLNs identified divided by total number of patients) and (2) rate of adverse events related to ICG injection (defined as the number of adverse events related to injection ICG divided by number of procedures). Secondary outcomes included: total number of SLNs, false negative SLNs, true negative SLNs, sensitivity, upstaging, aberrant lymph nodes, accuracy, and negative predictive value. Furthermore, intraoperative times were noted for the different steps of the procedure.
Technique
SLNi was performed using the da Vinci Xi (Intuitive Surgical Inc., Sunnyvale, USA) robot-assisted surgical platform. First, the abdominal cavity was inspected to rule out a T4 tumour or visible metastases that would exclude the patient from continuing the study. Second, 25 mg of ICG (Verdye, Diagnostic Green GmbH, Aschheim-Dornach, Germany) was diluted in 5 ml water for injection. Third, a gastroenterologist performed a colonoscopy and submucosally injected 1 ml of ICG in four aliquots around the tumour (4 ml in total). After the first four patients, aliquots were created with 0.9% NaCl. Subsequently, the ICG was injected in this aliquot to minimise risk of intra-abdominal spillage of ICG. After injection of ICG, the mesocolon was inspected with the NIRF ‘Firefly’ mode of the da Vinci Xi. Thereafter, SLNs were marked with a suture. Afterwards, segmental resection was performed according to standard of care to ensure removal of lymph node metastases in non-SLNs. If no sentinel lymph nodes were found during in vivo examination, a repeated ex vivo fluorescence examination of the specimen was performed using the Firefly.
Pathological examination of the lymph nodes
Immediately after surgery, the pathologist used the sutures to identify and isolate SLNs from the specimen. Excised SLNs were again evaluated for the presence of fluorescence using the Firefly. SLNs were ultrastaged: paraffin-embedded tissue blocks were sectioned at 250 μm intervals and examined at five levels using hematoxylin–eosin staining and immunohistochemically staining with a cytokeratin AE1/AE3 antibody cocktail, based on the current standard pathology assessment of SLNs in breast cancer [22]. Non-SLNs were stained with hematoxylin–eosin. In case both the SLNs and non-SLNs were negative for metastases after initial assessment, all non-SLNs were also ultrastaged.
Definitions
Three categories of lymph node metastases were defined: isolated tumour cells (≤ 0.2 mm), micrometastases (0.2–2 mm), and macrometastases (> 2 mm). Micrometastases and macrometastases were considered positive lymph nodes. SLNs were defined as the first, up to four, fluorescent lymph nodes visible after injection. Other lymph nodes were defined as non-SLNs. Upstaging was defined as patients with lymph nodes metastases after ultrastaging, and aberrant lymph nodes as SLNs outside the planned resection margins. False negative SLNs were defined as negative SLNs with positive non-SLNs, and true negative SLNs as the SLN and the non-SLN not containing metastases. Sensitivity was the proportion of patients with a positive SLN divided by the total number of patients with metastases (the sum of patients with a positive SLN and false negative SLNs). Accuracy was the sum of positive SLNs and true negative SLNs as a percentage of patients in which an SLN was found. Preoperative cT-classification was based on computed tomography. If a tumour could not be localised (cTx), it was considered cT1-2. Colonoscopy time was defined as the time from start of colonoscopy until the end of the colonoscopy. Detection time was the time from first ICG injection to first SLNi. Total SLNi time was the time from start of the colonoscopy to continuing the surgical procedure according to standard of care, and operation time was the time from first incision to wound closure.
Statistics
Descriptive statistics were used to describe patient and tumour characteristics.
Results
Patients
Ten consecutive patients with cT1-2N0M0 CC underwent curative resection between September 2020 and August 2021. Seven males and three females were included with a mean age of 70 years (range 59–84 years), body mass index ranged from 21 to 35 kg/m2, and 60% of patients had ASA 2 score (Table 1).
Intraoperative outcomes
There were no adverse events related to ICG or its injection. Minimal intra-abdominal leakage of ICG occurred in patient 4 (Table 2). Thereafter, 0.9% NaCl submucosal aliquots were first created before ICG administration; still another leakage occurred in patient 9. Nevertheless, SLNi was possible regardless of minimal intra-abdominal leakage of ICG in the two patients. In total, 22 sutures were placed to mark a potential SLN (Fig. 1). One suture turned out to be an injection spot during ex vivo examination, but two other sutures correctly marked SLNs in this patient. SLNi rate was 100%; at least one SLN (mean 2.3 SLNs per patient) was identified in all patients (Table 3). In patient 5 and 10, two fluorescent lymph nodes were found near the same suture, thus both were assigned as SLN. In patient 7, a limited fluorescent SLN was visible, and due to uncertainty of having marked an SLN, ex vivo fluorescence examination revealed an additional SLN. No aberrant SLNs were found.
a The near-infrared fluorescence (NIRF) view of the mesocolon, b annotated picture, and c and the white-light picture of the same view as a reference. a Two sentinel lymph nodes (SLNs) and the corresponding lymphatic vessels were visible using NIRF. b The first and second visible SLN are highlighted with a white and red circle, respectively; both SLNs were to become brighter after waiting some time. The lymph vessels are highlighted in green. Bringing the camera closer to the tissue would also improve visibility of the SLNs (Color figure online)
The median colonoscopy time was 12 min (range 8–44 min), detection time 6 min (range 2–54 min), total SLNi time 30.5 min (range 18–75 min), and operation time 133 min (range 92–240 min). In two patients, conversion was required due to limited overview; SLNi was already completed in one patient. In the other patient SLNi was performed after laparotomy by covering the abdominal cavity with gauzes, dimming the operating room lights, and inspecting the mesocolon whilst holding the da Vinci camera. In addition, one conversion was required due to bleeding during the segmental dissection phase and postoperative blood transfusion was required. Subsequently, the patient experienced postoperative ileus and wound infection, which later resolved.
Pathological examination
Presence of fluorescence was confirmed in all SLNs after isolating the SLN from the specimen. Two patients, patient 2 and 7, had macrometastases in the SLN (Table 3). In addition, isolated tumour cells were found in a second SLN of patient 2. In patient 7, two SLNs were identified although the SLNs showed reduced NIRF. These two SLNs contained massive lymph node metastases with little residual lymph node tissue. Microscope slides of massive lymph node metastases showed that fluorescence is (largely) absent in and around metastases compared to normal lymph node tissue (Fig. 2). Furthermore, there were no patients with false negative SLNs. Thus, eight patients had a true negative SLN (Table 3). As a result, sensitivity and accuracy were 100%, and the negative predictive value was 1. The diameter of SLNs ranged from 1 to 13 mm. No patient was upstaged after ultrastaging. Five out of ten patients had a pT3 tumour.
Massive lymph node metastases in a SLN. a Ex vivo macroscopic view with the Firefly after the SLN (9 mm in diameter) was isolated from the specimen. NIRF in the SLN was unevenly distributed. b, d Two intervals of the same SLN on microscope slides with hematoxylin and eosin (H&E) staining with a black bar demonstrating 1 mm. c, e The NIRF view of the same slides with the LI-COR Odyssey CLx flatbed imager (LI-COR Biosciences Inc., NE, USA); bright yellow represents a high fluorescence signal, while dark purple represents a low signal. b Lymph node metastases, displayed in the green circle, surrounded by normal lymph node tissue. Sidenote: ink from the endoscopic tattoo was visible in the SLN; an example is magnified. c The flatbed scanner showed reduced NIRF in and near the lymph node metastases. d Metastases almost entirely occupied this SLN interval with only a small area of residual normal lymph node tissue displayed in the blue circle. e The NIRF signal is low to absent in the microscope slide compared to panel (c) (Color figure online)
Discussion
This pilot study aimed to assess safety and feasibility of robot-assisted fluorescence-guided SLNi using submucosally injected ICG in patients with cT1-2N0 CC. At least one SLN was identified in every patient (median 2.3 SLNs). The SLNs correctly represented the presence or absence of lymph node metastases in all patients. No tracer (injection-)related adverse events occurred. One intraoperative bleeding occurred during the segmental dissection phase of the procedure, after having completed SLNi, which required a laparotomy and blood transfusion.
Twenty-one sutures correctly marked an SLN, although a single suture incorrectly marked an injection spot as an SLN. Similarly, Currie et al. described that in 2 out of 30 patients a fluorescent marked spot was not a lymph node [23]. Performing white-light examination during SLNi, thus turning off NIRF mode, might prevent incorrectly marking an injection spot. Presence of fluorescence was confirmed in all SLNs after isolating the SLN from the specimen. Since all lymph node metastases were detected with SLNi, sensitivity and accuracy were 100% in this pilot study. In a meta-analysis (N = 139), SLNi for T1-2 CC had 80% sensitivity and 98% accuracy [20], which might already be sufficient for SLNi when considering the risk of lymph node metastases is 10–20% for pT1-2 tumours [4, 5]. The negative consequences of missed lymph node metastases could outweigh the morbidity and mortality of segmental resection [6,7,8,9,10]. Ultimately, to prove the reliability of SLNi a study of 3000 patients would be required (assuming a 10% chance of lymph node metastases, 95% identification rate, and 5% false negative rate) [24], which might not be feasible.
In one patient, two SLNs with massive lymph node metastases were identified with the Firefly although the SLNs had a (subjectively) low NIRF intensity compared to other SLNs. The massive lymph node metastases, with little residual lymph node tissue, might have resulted in limited ICG uptake in these SLNs. The effect of massive lymph node metastases on tracer uptake was also seen by Ribero et al. in 1/70 patients following ICG lymphadenectomy [25], but was also reported in earlier studies for locally advanced tumours and lymph node metastases that blocked lymphatic vessels [26, 27]. NIRF is negatively correlated with the percentage of lymph node that is occupied with metastases, resulting in that no fluorescence was detectable in lymph nodes containing > 90% cancer cells [28]. Thus, one should be aware that limited, or no, visible SLNs could signify the presence of lymph node metastases. Therefore, ex vivo SLNi should be attempted to find additional SLNs in case of uncertainty or standard segmental resection should be performed. Ideally, contrast between SLNs and background should be high to facilitate identification. SLNi can be hindered by background NIRF (i.e., scattering, autofluorescence of tissue, and automatic gain of NIRF systems [29,30,31,32,33]) and spillage of ICG [34]. In our study spillage occurred two times; once after the introduction of 0.9% NaCl aliquots before ICG injection. After the NaCl injection failed to form a proper aliquot, indicating a possible transmural penetration, changing the injection site could have prevented the second spillage of ICG. However, SLNi was still possible in both cases of spillage. Spillage may occur in both subserosal and submucosal injection methods [20], however, it is hypothesised that submucosal administration could lead to less false negative SLNs since it is injected near the tumour [35].
Although several methods of injection of ICG are being used, we chose to perform intraoperative injection of ICG for SLNi as more, and higher echelon, lymph nodes will be visible after prolonged waiting. Median detection time of SLNs was 6 min. A systematic review found that more SLNs were identified 15 min after injection [35]. Cahill et al. had similar laparoscopic SLN detection times after intraoperative ICG injection, but also demonstrated that preoperative injection of ICG led to detection of 12 fluorescent lymph nodes [36]. In addition, the short interval between injection of ICG and SLNi could be why no aberrant lymph nodes were observed in our study. For instance, 49% of patients had aberrant lymph nodes after ICG was injected 24 h preoperatively [25]. However, Saha et al. demonstrated that only 1% of patients had isolated metastases in aberrant lymph nodes, which were all found in T3-4 tumours [37]. In another study, Saha et al. showed that all lymph node metastases were found in the segment of the colon with the primary tumour while no metastases were found in the distal segment of the colon (outside the field of SLNs) if the proximal part was negative [38]. Therefore, we question the importance of aberrant SLNs in T1-2 CC.
Both patient and tumour characteristics were important for SLNi. Colonoscopy time and total SLNi time were substantially longer in two patients with a tumour in the splenic flexure. In one of these patients, the tumour was preoperatively localised in the descending colon and ultimately re-docking of the robot was required. In the other patient, conversion to laparotomy was required due to a limited view associated with obesity. After laparotomy, SLNi could still be performed by covering the abdominal cavity with gauzes and dimming lights in the operating theatre. Injection of ICG was completed within 15 min in the remaining eight patients. Regarding tumour characteristics, this study intended to include only patients with pT1-2 tumours as more invasive tumours might alter lymph drainage patterns [36, 39,40,41,42,43,44,45,46]. Six prior studies distinguished between SLNi in patients with T1-2 tumours and T3-4 tumours [23, 35, 41, 43, 45, 47]. However, only two studies had false negative SLNs, which used subserosal injection or older camera systems [23, 41]. More sensitive NIRF laparoscopes have been developed in recent years, and a stable robotic surgical platform with magnified 3D view could be highly beneficial for detecting small SLNs; even down to 1 mm as shown in our study. As reported in literature, half of positive lymph nodes are present in ≤ 5–6 mm lymph nodes and the largest metastatic lymph node might only be 2–3 mm [48, 49]. Therefore, the da Vinci Xi robot would be capable enough to detect clinically relevant SLNs using the SLNi technique described in this study. Regarding patient selection based on tumour characteristics, 50% of patients in this study had pT3 tumours despite complete preoperative work-up according to guidelines. Likewise, Currie et al. intended to perform SLNi in patients with T1-2 tumours: 13 out of 27 patients had pT3 tumours. The number of patients incorrectly preoperatively staged as cT1-2 corresponds to the 43% understaging of cT1-2 patients found in our previously published study that was conducted as a result of this pilot study [50]. More research should be performed regarding preoperative staging of CC for patient-tailored treatment. Nevertheless, SLNi in our study was not negatively impacted by patients with a pT3 tumours.
Strengths and limitations
To our knowledge, this is the first study exploring robot-assisted SLNi using intraoperative submucosal ICG injections in ten patients, as prior studies on robot-assisted SLNi used preoperative ICG injection for lymphadenectomy [25, 51, 52]. Consecutive patients were asked to participate and neither BMI nor tumour location were exclusion criteria. Robot-assisted segmental resection of a tumour in the splenic flexure and high BMI was more challenging. Thus, a more careful selection of patients might aid SLNi as a good overview of the mesocolon is required, but difficult (patient) characteristics ultimately did not prevent SLNi.
Although colonoscopy time was relatively short, intraoperative colonoscopies were performed by a gastroenterologist, which required logistical coordination and downtime was not measured. SLNi cases were scheduled first of the day and resulted in shorter downtime for the gastroenterologist. In other hospitals, surgeons might inject ICG themselves. Alternatively, tumour-targeted tracers could improve logistics as preoperative administration is possible. Bevacizumab-800CW [53, 54], cetuximab-800CW [55, 56] and SGM-101 [57], targeting, respectively, VEGF-A, EGFR, and CEA, are currently being investigated for the detection of resection margins of the primary tumour and (lymph node) metastases. More importantly, tumour-targeted tracers can be intravenously administered to detect lymph node metastases and would eliminate the need for colonoscopy. In addition, intravenous administration is not hindered by massive lymph node metastases or locally advanced cancers that block lymph flow.
Conclusion
Robot-assisted fluorescence-guided SLNi in cT1-2N0M0 CC using intraoperative submucosal ICG injection was safe, feasible, and was performed in a timely manner. SLNi was achieved in all ten patients and SLNs down to 1 mm were detected. Furthermore, SLNi correctly identified the presence of lymph node metastases if SLN biopsy had been performed instead of segmental resection. Future studies in SLN biopsy and tumour-targeted tracers for the detection of lymph node metastases in CC are warranted.
Abbreviations
- CC:
-
Colon cancer
- ICG:
-
Indocyanine green
- NIRF:
-
Near-infrared fluorescence
- SLN:
-
Sentinel lymph node
- SLNi:
-
Sentinel lymph node identification
- cTNM:
-
Clinical TNM stage
- pTNM:
-
Pathological TNM stage
References
Netherlands Cancer Registry. National data. https://iknl.nl/nkr-cijfers. Accessed 14 Nov 2022
CBS (2022) Deaths; underlying cause of death (shortlist), sex, age. https://opendata.cbs.nl/statline/#/CBS/en/dataset/7052eng/table?ts=1668456838794. Accessed 14 Nov 2022
Breekveldt ECH, Lansdorp-Vogelaar I, Toes-Zoutendijk E, Spaander MCW, van Vuuren AJ, van Kemenade FJ, Ramakers CRB, Dekker E, Nagtegaal ID, Krul MF, Kok NFM, Kuhlmann KFD, Vink GR, van Leerdam ME, Elferink MAG (2022) Colorectal cancer incidence, mortality, tumour characteristics, and treatment before and after introduction of the faecal immunochemical testing-based screening programme in the Netherlands: a population-based study. Lancet Gastroenterol Hepatol 7:60–68. https://doi.org/10.1016/S2468-1253(21)00368-X
Backes Y, Elias SG, Bhoelan BS, Groen JN, van Bergeijk J, Seerden TCJ, Pullens HJM, Spanier BWM, Geesing JMJ, Kessels K, Kerkhof M, Siersema PD, de Vos tot Nederveen Cappel WH, van Lelyveld N, Wolfhagen FHJ, ter Borg F, Offerhaus GJA, Lacle MM, Moons LMG (2017) The prognostic value of lymph node yield in the earliest stage of colorectal cancer: a multicenter cohort study. BMC Med 15:1–11. https://doi.org/10.1186/s12916-017-0892-7
Ricciardi R, Madoff RD, Rothenberger DA, Baxter NN (2006) Population-based analyses of lymph node metastases in colorectal cancer. Clin Gastroenterol Hepatol 4:1522–1527. https://doi.org/10.1016/j.cgh.2006.07.016
van den Bosch T, Warps A-LK, Tot Babberich MP, Stamm C, Geerts BF, Vermeulen L, Wouters MWJM, Dekker JWT, Tollenaar RAEM, Tanis PJ, Miedema DM, Audit DC (2021) Predictors of 30-day mortality among Dutch patients undergoing colorectal cancer surgery, 2011–2016. JAMA Netw Open 4:e217737. https://doi.org/10.1001/jamanetworkopen.2021.7737
Sánchez-Guillén L, Frasson M, García-Granero PG, Flor-Lorente B, Álvarez-Sarrado E, García-Granero E (2019) Risk factors for leak, complications and mortality after ileocolic anastomosis: comparison of two anastomotic techniques. Ann R Coll Surg Engl 101:571–578. https://doi.org/10.1308/rcsann.2019.0098
Dohrn N, Klein MF, Gögenur I (2021) Robotic versus laparoscopic right colectomy for colon cancer: a nationwide cohort study. Int J Colorectal Dis 36:2147–2158. https://doi.org/10.1007/s00384-021-03966-y
Liu H, Zhu X, Yu J, He P, Shen B, Tang X, Xu X, Wei D, Chen Y, Li X (2021) The quality of life of patients with colorectal cancer and a stoma in China: a quantitative cross-sectional study. Adv Skin Wound Care 34:302–307. https://doi.org/10.1097/01.ASW.0000744348.32773.b9
Whistance RN, Conroy T, Chie W, Costantini A, Sezer O, Koller M, Johnson CD, Pilkington SA, Arraras J, Ben-Josef E, Pullyblank AM, Fayers P, Blazeby JM (2009) Clinical and psychometric validation of the EORTC QLQ-CR29 questionnaire module to assess health-related quality of life in patients with colorectal cancer. Eur J Cancer 45:3017–3026. https://doi.org/10.1016/j.ejca.2009.08.014
Weixler B, Warschkow R, Güller U, Zettl A, von Holzen U, Schmied B, Zuber M (2016) Isolated tumor cells in stage I & II colon cancer patients are associated with significantly worse disease-free and overall survival. BMC Cancer 16(1):1–7
Saha S, Elgamal M, Cherry M, Buttar R, Pentapati S, Mukkamala S, Devisetty K, Kaushal S, Alnounou M, Singh T, Grewal S, Eilender D, Arora M, Wiese D (2018) Challenging the conventional treatment of colon cancer by sentinel lymph node mapping and its role of detecting micrometastases for adjuvant chemotherapy. Clin Exp Metastasis 35:463–469
QUASAR Collaborative Group (2007) Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. The Lancet 370:2020–2029. https://doi.org/10.1016/S0140-6736(07)61866-2
Bilchik AJ, Trocha SD (2003) Lymphatic mapping and sentinel node analysis to optimize laparoscopic resection and staging of colorectal cancer: an update. Cancer Control 10(3):219–223
Leicher LW, Huisman JF, van Grevenstein WMU, Didden P, Backes Y, Offerhaus GJA, Laclé MM, Moll FCP, Geesing JMJ, Smakman N, Droste JSTS, Verdaasdonk EGG, Ter Borg F, Talsma AK, Erkelens GW, van der Zaag ES, Schrauwen RWM, van Wely BJ, Schot I, Vermaas M, van Bergeijk JD, Sietses C, Hazen WL, Wasowicz DK, Ramsoekh D, Tuynman JB, Alderlieste YA, Renger R-J, Oort FA, Bilgen EJS, Vleggaar FP, de Vos VasenTot Nederveen Cappel HFAWH, Moons LMG, van Westreenen HL (2022) Colonoscopic-assisted laparoscopic wedge resection for colonic lesions: a prospective multicentre cohort study (LIMERIC-study). Ann Surg. https://doi.org/10.1097/SLA.0000000000005417
Cahill RA, Leroy J, Marescaux J (2009) Localized resection for colon cancer. Surg Oncol 18:334–342. https://doi.org/10.1016/j.suronc.2008.08.004
Des Guetz G, Uzzan B, Nicolas P, Cucherat M, De Mestier P, Morere JF, Breau JL, Perret G (2007) Is sentinel lymph node mapping in colorectal cancer a future prognostic factor? A meta-analysis. World J Surg 31:1304–1312. https://doi.org/10.1007/s00268-007-9059-6
van der Pas MHGM, Meijer S, Hoekstra OS, Riphagen II, de Vet HC, Knol DL, van Grieken NC, Meijerink WJ (2011) Sentinel-lymph-node procedrue in colon and rectal cancer: a systematic review and meta-analysis. Lancet Oncol 12:540–550. https://doi.org/10.1016/S1470
Currie AC (2019) Intraoperative sentinel node mapping in the colon: potential and pitfalls. Eur Surg Res. https://doi.org/10.1159/000494833
Burghgraef TA, Zweep AL, Sikkenk DJ, van der Pas MHGM, Verheijen PM, Consten ECJ (2021) In vivo sentinel lymph node identification using fluorescent tracer imaging in colon cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol 158:103149. https://doi.org/10.1016/j.critrevonc.2020.103149
Richtlijnendatabase. Colorectaal carcinoom (CRC). https://richtlijnendatabase.nl/richtlijn/colorectaal_carcinoom_crc/startpagina_-_crc.html. Accessed 1 Mar 2023
Oncoline Nationale richtlijn borstkanker
Currie AC, Brigic A, Thomas-Gibson S, Suzuki N, Moorghen M, Jenkins JT, Faiz OD, Kennedy RH (2017) A pilot study to assess near infrared laparoscopy with indocyanine green (ICG) for intraoperative sentinel lymph node mapping in early colon cancer. Eur J Surg Oncol 43:2044–2051. https://doi.org/10.1016/j.ejso.2017.05.026
Tanis PJ, Nieweg OE, Hart AAM, Kroon BBR (2002) The illusion of the learning phase for lymphatic mapping. Ann Surg Oncol 9:142–147. https://doi.org/10.1007/BF02557365
Ribero D, Mento F, Sega V, Lo Conte D, Mellano A, Spinoglio G (2022) ICG-guided lymphadenectomy during surgery for colon and rectal cancer-interim analysis of the GREENLIGHT trial. Biomedicines 10:541. https://doi.org/10.3390/biomedicines10030541
Patten LC, Berger DH, Rodriguez-Bigas M, Mansfield P, Delpassand E, Cleary KR, Fagan SP, Curley SA, Hunt KK, Feig BW (2004) A prospective evaluation of radiocolloid and immunohistochemical staining in colon carcinoma lymphatic mapping. Cancer 100:2104–2109. https://doi.org/10.1002/cncr.20233
Grinnell RS (1966) Lymphatic block with atypical and retrograde lymphatic metastasis and spread in carcinoma of the colon and rectum. Ann Surg 163(2):272
Sato Y, Satoyoshi T, Okita K, Kyuno D, Hamabe A, Okuya K, Nishidate T, Akizuki E, Ishii M, Yamano H-O, Sugita S, Nakase H, Hasegawa T, Takemasa I (2021) Snapshots of lymphatic pathways in colorectal cancer surgery using near-infrared fluorescence, in vivo and ex vivo. Eur J Surg Oncol 47:3130–3136. https://doi.org/10.1016/j.ejso.2021.07.025
Kang H, Shamim M, Yin X, Adluru E, Fukuda T, Yokomizo S, Chang H, Park SH, Cui Y, Moy AJ, Kashiwagi S, Henary M, Choi HS (2022) Tumor-associated immune-cell-mediated tumor-targeting mechanism with NIR-II fluorescence imaging. Adv Mater 34:e2106500. https://doi.org/10.1002/adma.202106500
Kenry, Duan Y, Liu B (2018) Recent advances of optical imaging in the second near-infrared window. Adv Mater 30:e1802394. https://doi.org/10.1002/adma.201802394
He M, Wu D, Zhang Y, Fan X, Zhuang S, Yang W, Lin H, Qian J (2020) Protein-enhanced NIR-IIb emission of indocyanine green for functional bioimaging. ACS Appl Bio Mater 3:9126–9134. https://doi.org/10.1021/acsabm.0c01384
Li C, Chen G, Zhang Y, Wu F, Wang Q (2020) Advanced fluorescence imaging technology in the near-infrared-II window for biomedical applications. J Am Chem Soc 142:14789–14804. https://doi.org/10.1021/jacs.0c07022
Hong G, Antaris AL, Dai H (2017) Near-infrared fluorophores for biomedical imaging. Nat Biomed Eng 1:10. https://doi.org/10.1038/s41551-016-0010
Ho MF, Futaba K, Mak TWC, Ng SSM (2022) Personalized laparoscopic resection of colon cancer with the use of indocyanine green lymph node mapping: technical and clinical outcomes. Asian J Endosc Surg 15:563–568. https://doi.org/10.1111/ases.13050
Ankersmit M, Bonjer HJ, Hannink G, Schoonmade LJ, van der Pas MHGM, Meijerink WJHJ (2019) Near-infrared fluorescence imaging for sentinel lymph node identification in colon cancer: a prospective single-center study and systematic review with meta-analysis. Tech Coloproctol 23:1113–1126. https://doi.org/10.1007/s10151-019-02107-6
Cahill RA, Anderson M, Wang LM, Lindsey I, Cunningham C, Mortensen NJ (2012) Near-infrared (NIR) laparoscopy for intraoperative lymphatic road-mapping and sentinel node identification during definitive surgical resection of early-stage colorectal neoplasia. Surg Endosc 26:197–204. https://doi.org/10.1007/s00464-011-1854-3
Saha S, Johnston G, Korant A, Shaik M, Kanaan M, Johnston R, Ganatra B, Kaushal S, Desai D, Mannam S (2013) Aberrant drainage of sentinel lymph nodes in colon cancer and its impact on staging and extent of operation. Am J Surg 205:302–305
Saha S, Philimon B, Efeson M, Helina A, Elgamal M, Kiya G, Hilkiah S, Arora M, Wiese D, Kitagawa Y (2022) The role of sentinel lymph node mapping in colon cancer: detection of micro-metastasis, effect on survival, and driver of a paradigm shift in extent of colon resection. Clin Exp Metastasis 39:109–115. https://doi.org/10.1007/s10585-021-10121-y
Chand M, Keller DS, Joshi HM, Devoto L, Rodriguez-Justo M, Cohen R (2018) Feasibility of fluorescence lymph node imaging in colon cancer: FLICC. Tech Coloproctol 22:271–277. https://doi.org/10.1007/s10151-018-1773-6
van der Pas MHGM, Ankersmit M, Stockmann HBAC, Silvis R, van Grieken NCT, Bril H, Meijerink WJHJ (2013) Laparoscopic sentinel lymph node identification in patients with colon carcinoma using a near-infrared dye: description of a new technique and feasibility study. J Laparoendosc Adv Surg Tech 23:367–371. https://doi.org/10.1089/lap.2012.0407
Kusano M, Tajima Y, Yamazaki K, Kato M, Watanabe M, Miwa M (2008) Sentinel node mapping guided by indocyanine green fluorescence imaging: a new method for sentinel node navigation surgery in gastrointestinal cancer. Dig Surg 25:103–108. https://doi.org/10.1159/000121905
Hirche C, Mohr Z, Kneif S, Doniga S, Murawa D, Strik M, Hünerbein M (2012) Ultrastaging of colon cancer by sentinel node biopsy using fluorescence navigation with indocyanine green. Int J Colorectal Dis 27:319–324. https://doi.org/10.1007/s00384-011-1306-5
Nagata K, Endo S, Hidaka E, Tanaka JI, Kudo SE, Shiokawa A (2006) Laparoscopic sentinel node mapping for colorectal cancer using infrared ray laparoscopy. Anticancer Res 26:2307–2311
Dan AG, Saha S, Monson KM, Wiese D, Schochet E, Barber KR, Ganatra B, Desai D, Kaushal S (2014) 1% lymphazurin vs 10% fluorescein for sentinel node mapping in colorectal tumors. Arch Surg 139:1180–1184
Andersen HS, Bennedsen ALB, Burgdorf SK, Eriksen JR, Eiholm S, Toxværd A, Riis LB, Rosenberg J, Gögenur I (2017) In vivo and ex vivo sentinel node mapping does not identify the same lymph nodes in colon cancer. Int J Colorectal Dis 32:983–990. https://doi.org/10.1007/s00384-017-2777-9
Ankersmit M, Hoekstra OS, van Lingen A, Bloemena E, Jacobs MAJM, Vugts DJ, Bonjer HJ, van Dongen GAMS, Meijerink WJHJ (2019) Perioperative PET/CT lymphoscintigraphy and fluorescent real-time imaging for sentinel lymph node mapping in early staged colon cancer. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-019-04284-w
Carrara A, Motter M, Amabile D, Pellecchia L, Moscatelli P, Pertile R, Barbareschi M, Decarli NL, Ferrari M, Tirone G (2020) Predictive value of the sentinel lymph node procedure in the staging of non-metastatic colorectal cancer. Int J Colorectal Dis 35:1921–1928. https://doi.org/10.1007/s00384-020-03654-3
Märkl B, Rößle J, Arnholdt HM, Schaller T, Krammer I, Cacchi C, Jähnig H, Schenkirsch G, Spatz H, Anthuber M (2012) The clinical significance of lymph node size in colon cancer. Mod Pathol 25:1413–1422. https://doi.org/10.1038/modpathol.2012.92
Schrembs P, Martin B, Anthuber M, Schenkirsch G, Märkl B (2018) The prognostic significance of lymph node size in node-positive colon cancer. PLoS ONE 13:e0201072. https://doi.org/10.1371/journal.pone.0201072
Sikkenk DJ, Sijmons JML, Burghgraef TA, Asaggau I, Vos A, da Costa DW, Somers I, Verheijen PM, Dekker J-WT, Nagengast WB, Tanis PJ, Consten ECJ (2023) Nationwide practice in CT-based preoperative staging of colon cancer and concordance with definitive pathology. Eur J Surg Oncol. https://doi.org/10.1016/j.ejso.2023.05.016
Petz W, Bertani E, Borin S, Fiori G, Ribero D, Spinoglio G (2021) Fluorescence-guided D3 lymphadenectomy in robotic right colectomy with complete mesocolic excision. Int J Med Robot 17:e2217. https://doi.org/10.1002/rcs.2217
Spinoglio G, Petz W, Borin S, Piccioli AN, Bertani E (2019) Robotic right colectomy with complete mesocolic excision and indocyanine green guidance. Minerva Chir 74:165–169. https://doi.org/10.23736/S0026-4733.18.07831-8
de Jongh SJ, Tjalma JJJ, Koller M, Linssen MD, Vonk J, Dobosz M, Jorritsma-Smit A, Kleibeuker JH, Hospers GAP, Havenga K, Hemmer PHJ, Karrenbeld A, van Dam GM, van Etten B, Nagengast WB (2020) Back-table fluorescence-guided imaging for circumferential resection margin evaluation using bevacizumab-800CW in patients with locally advanced rectal cancer. J Nucl Med 61:655–661. https://doi.org/10.2967/jnumed.119.232355
Harlaar NJ, Koller M, de Jongh SJ, van Leeuwen BL, Hemmer PH, Kruijff S, van Ginkel RJ, Been LB, de Jong JS, Kats-Ugurlu G, Linssen MD, Jorritsma-Smit A, van Oosten M, Nagengast WB, Ntziachristos V, van Dam GM (2016) Molecular fluorescence-guided surgery of peritoneal carcinomatosis of colorectal origin: a single-centre feasibility study. Lancet Gastroenterol Hepatol 1:283–290. https://doi.org/10.1016/S2468-1253(16)30082-6
Rosenthal EL, Moore LS, Tipirneni K, de Boer E, Stevens TM, Hartman YE, Carroll WR, Zinn KR, Warram JM (2017) Sensitivity and specificity of cetuximab-IRDye800CW to identify regional metastatic disease in head and neck cancer. Clin Cancer Res 23:4744–4752. https://doi.org/10.1158/1078-0432.CCR-16-2968
Vonk J, de Wit JG, Voskuil FJ, Tang YH, Hooghiemstra WT, Linssen MD, van den Broek E, Doff JJ, de Visscher SA, Schepman KP, van der Vegt B, van Dam GM, Witjes MJ (2021) Epidermal growth factor receptor targeted fluorescence molecular imaging for postoperative lymph node assessment in patients with oral cancer. J Nucl Med. https://doi.org/10.2967/jnumed.121.262530
Boogerd LSF, Hoogstins CES, Schaap DP, Kusters M, Handgraaf HJM, van der Valk MJM, Hilling DE, Holman FA, Peeters KCMJ, Mieog JSD, van de Velde CJH, Farina-Sarasqueta A, van Lijnschoten I, Framery B, Pèlegrin A, Gutowski M, Nienhuijs SW, de Hingh IHJT, Nieuwenhuijzen GAP, Rutten HJT, Cailler F, Burggraaf J, Vahrmeijer AL (2018) Safety and effectiveness of SGM-101, a fluorescent antibody targeting carcinoembryonic antigen, for intraoperative detection of colorectal cancer: a dose-escalation pilot study. Lancet Gastroenterol Hepatol 3:181–191. https://doi.org/10.1016/S2468-1253(17)30395-3
Funding
This research was funded by the European Association for Endoscopic Surgery 2020 and ‘Stichting het Stichts Gastroenterologisch Genootschap’ 2020 grant. Funding had no role in the design of the study; in data collection, analyses, or interpretation; in writing the manuscript; or in the decision to publish the study. No right of review of the data or manuscript was requested or provided.
Author information
Authors and Affiliations
Contributions
DJS, AJS, TAB, HA, MPS, RA, PMV, WBN, ECJC: Conceptualisation. DJS, AJS, TAB, HA, MPS, RA, PMV, WBN, ECJC: Methodology. DJS: software. DJS: validation. DJS, AJS: formal analysis. DJS, AJS, HA, MPS, RA, PMV, ECJC: investigation. DJS, AJS, HA, MPS, RA, PMV, WBN, ECJC: resources. DJS, AJS, TAB, HA, MPS, RA, PMV, WBN, ECJC: data curation. DJS: writing—original draft preparation. DJS, AJS, TAB, HA, MPS, RA, PMV, WBN, ECJC: writing—review and editing. DJS, AJS: visualisation. PMV, WBN, ECJC: supervision. DJS, AJS: project administration. DJS, TAB, PMV, ECJC: funding acquisition. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Disclosures
Daan J. Sikkenk and Esther C. J. Consten received grants from the ‘European Association for Endoscopic Surgery’ and ‘Stichting het Stichts Gastroenterologisch Genootschap’ for this study, but the funding had no role in the study. Esther C. J. Consten and Paul M. Verheijen are proctors for Intuitive Surgical. Daan J. Sikkenk, Andrea J. Sterkenburg, Thijs A. Burghgraef, Halil Akol, Matthijs P. Schwartz, René Arensman, Paul M. Verheijen, Wouter B. Nagengast and Esther C. J. Consten have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sikkenk, D.J., Sterkenburg, A.J., Burghgraef, T.A. et al. Robot-assisted fluorescent sentinel lymph node identification in early-stage colon cancer. Surg Endosc 37, 8394–8403 (2023). https://doi.org/10.1007/s00464-023-10394-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10394-2