Abstract
Background
Obesity is a chronic and progressive disease associated with significant morbidity, mortality, and health-care costs. Bariatric surgery is the most effective intervention for sustainable weight loss and resolution of obesity-related comorbidities. Studies examining comorbidity resolution largely rely on individual self-reported outcomes and electronic record reviews. We present a population-based study looking at prescription medication utilization before and after bariatric surgery as a measure of comorbidity resolution.
Methods
All patients enrolled in the Center for Metabolic and Bariatric Surgery who underwent either gastric bypass or sleeve gastrectomy between 2013 and 2019 in Manitoba were included. Demographic information, follow up, and outpatient prescription dispensation data were obtained from the Manitoba Population Research Data Repository housed at the Manitoba Centre for Health Policy for 5 years pre- and post-surgery.
Results
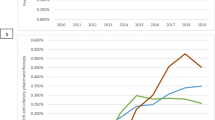
A total of 1184 patients were included. Antidepressants and selective serotonin reuptake inhibitors were the most commonly prescribed classes, and along with thyroid medication, utilization remained stable after bariatric surgery. Proton pump inhibitors and opioid class drugs increased at 1 year after surgery then returned to baseline. Glucose and lipid-lowering medications, including statins, biguanides, sulfonylureas, and insulin, were decreased. Antihypertensives, including ACE inhibitors, calcium channel blockers, angiotensin receptors blockers, thiazides, and beta blockers, similarly decreased.
Conclusion
This is the first Canadian study employing a provincial-wide prescription database to measure long-term comorbidity resolution after bariatric surgery. The use of administrative data eliminates potential biases and inaccuracies in follow up and self-reported outcomes. Consistent with the literature, prescriptions for the treatment of metabolic syndrome all decreased and were sustained at long-term follow up. Further studies are needed to delineate the effects of altered pharmaceutical utilization on patient quality of life and health-care expenditures.



Similar content being viewed by others
References
Haslam DW, James WP (2005) Obesity. Lancet 366(9492):1197–1209
Buchwald H (2005) Consensus conference statement bariatric surgery for morbid obesity: health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis 1(3):371–381
Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB (2003) Years of life lost due to obesity. JAMA 289(2):187–193
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH (2009) The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 9:88
NTF Prevention (2000) Overweight, obesity, and health risk. Arch Intern Med 160(7):898–904
Apovian CM (2016) Obesity: definition, comorbidities, causes, and burden. Am J Manag Care 22(7 Suppl):s176–s185
Ludwig DS, Pollack HA (2009) Obesity and the economy: from crisis to opportunity. JAMA 301(5):533–535
Adams TD, Meeks H, Fraser A, Davidson LE, Holmen J, Newman M et al (2023) Long-term all-cause and cause-specific mortality for four bariatric surgery procedures. Obesity (Silver Spring) 31(2):574–585
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K et al (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292(14):1724–1737
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA et al (2017) Bariatric surgery versus intensive medical therapy for diabetes - 5-year outcomes. N Engl J Med 376(7):641–651
Chang SH, Stoll CR, Song J, Varela JE, Eagon CJ, Colditz GA (2014) The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003–2012. JAMA Surg 149(3):275–287
Sjöström L, Peltonen M, Jacobson P, Ahlin S, Andersson-Assarsson J, Anveden Å et al (2014) Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA 311(22):2297–2304
Sarwer DB, Lavery M, Spitzer JC (2012) A review of the relationships between extreme obesity, quality of life, and sexual function. Obes Surg 22(4):668–676
Van den Eynde A, Mertens A, Vangoitsenhoven R, Meulemans A, Matthys C, Deleus E et al (2021) Psychosocial consequences of bariatric surgery: two sides of a coin: a scoping review. Obes Surg 31(12):5409–5417
Wölnerhanssen BK, Peterli R, Hurme S, Bueter M, Helmiö M, Juuti A et al (2021) Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy: 5-year outcomes of merged data from two randomized clinical trials (SLEEVEPASS and SM-BOSS). Br J Surg 108(1):49–57
Salminen P, Grönroos S, Helmiö M, Hurme S, Juuti A, Juusela R et al (2022) Effect of laparoscopic sleeve gastrectomy vs Roux-en-Y gastric bypass on weight loss, comorbidities, and reflux at 10 years in adult patients with obesity: the SLEEVEPASS randomized clinical trial. JAMA Surg 157(8):656–666
Gribsholt SB, Thomsen RW, Farkas DK, Sørensen HT, Richelsen B, Svensson E (2017) Changes in prescription drug use after gastric bypass surgery: a nationwide cohort study. Ann Surg 265(4):757–765
Pajecki D, Kawamoto F, Dantas ACB, Andrade PC, Brasil NC, Junqueira SM et al (2020) Real-world evidence of health outcomes and medication use 24 months after bariatric surgery in the public healthcare system in Brazil: a retrospective, single-center study. Clinics (Sao Paulo) 75:e1588
NIH Conference (1991) Gastrointestinal surgery for severe obesity. Consensus Development Conference Panel. Ann Intern Med 115(12):956–961
Brolin RE (1996) Update: NIH consensus conference. Gastrointestinal surgery for severe obesity. Nutrition 12(6):403–404
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J et al (2020) Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis 16(2):175–247
Howard R, Chao GF, Yang J, Thumma JR, Arterburn DE, Telem DA et al (2022) Medication use for obesity-related comorbidities after sleeve gastrectomy or gastric bypass. JAMA Surg 157(3):248–256
Kennedy AL, Nelson T, Pettine S, Miller BF, Hamilton KL, Donovan EL (2014) Medication use following bariatric surgery: factors associated with early discontinuation. Obes Surg 24(5):696–704
Segal JB, Clark JM, Shore AD, Dominici F, Magnuson T, Richards TM et al (2009) Prompt reduction in use of medications for comorbid conditions after bariatric surgery. Obes Surg 19(12):1646–1656
Gadiraju S, Lee CJ, Cooper DS (2016) Levothyroxine dosing following bariatric surgery. Obes Surg 26(10):2538–2542
Cunningham JL, Merrell CC, Sarr M, Somers KJ, McAlpine D, Reese M et al (2012) Investigation of antidepressant medication usage after bariatric surgery. Obes Surg 22(4):530–535
Durão C, Vaz C, de Oliveira VN, Calhau C (2021) Confinement during the COVID-19 pandemic after metabolic and bariatric surgery-associations between emotional distress, energy-dense foods, and body mass index. Obes Surg 31(10):4452–4460
Bellicha A, Lassen PB, Poitou C, Genser L, Marchelli F, Aron-Wisnewsky J et al (2022) Effect of COVID-19 lockdowns on physical activity, eating behavior, body weight and psychological outcomes in a post-bariatric cohort. Obes Surg 32(7):1–9
Pereira X, Romero-Velez G, Skendelas JP, Rodriguez-Quintero JH, Grosser R, Lima DL et al (2021) The COVID-19 pandemic did not affect target weight loss 1 year post bariatric surgery. Obes Surg 31(11):4926–4932
Hardy K, Anistratov A, He W, Daeninck F, Gu J, Vergis A (2022) Bariatric patient experience with virtual care during the COVID-19 pandemic. Obes Surg 32(3):940–943
Patkar A, Fegelman E, Sangeetha RK, Brethauer S, Bour E, Yoo A et al (2017) Assessing the real-world effect of laparoscopic bariatric surgery on the management of obesity-related comorbidities: A retrospective matched cohort study using a US Claims Database. Diabetes Obes Metab 19(2):181–188
Schiavon CA, Bersch-Ferreira AC, Santucci EV, Oliveira JD, Torreglosa CR, Bueno PT et al (2018) Effects of bariatric surgery in obese patients with hypertension: the GATEWAY randomized trial (gastric bypass to treat obese patients with steady hypertension). Circulation 137(11):1132–1142
Tajeu GS, Johnson E, Buccilla M, Gadegbeku CA, Janick S, Rubin D et al (2022) Changes in antihypertensive medication following bariatric surgery. Obes Surg 32(4):1312–1324
Hatoum IJ, Blackstone R, Hunter TD, Francis DM, Steinbuch M, Harris JL et al (2016) Clinical factors associated with remission of obesity-related comorbidities after bariatric surgery. JAMA Surg 151(2):130–137
Benaiges D, Sagué M, Flores-Le Roux JA, Pedro-Botet J, Ramón JM, Villatoro M et al (2016) Predictors of hypertension remission and recurrence after bariatric surgery. Am J Hypertens 29(5):653–659
Hinojosa MW, Varela JE, Smith BR, Che F, Nguyen NT (2009) Resolution of systemic hypertension after laparoscopic gastric bypass. J Gastrointest Surg 13(4):793–797
Carlsson LMS, Sjöholm K, Karlsson C, Jacobson P, Andersson-Assarsson JC, Svensson PA et al (2017) Long-term incidence of microvascular disease after bariatric surgery or usual care in patients with obesity, stratified by baseline glycaemic status: a post-hoc analysis of participants from the Swedish Obese Subjects study. Lancet Diabetes Endocrinol 5(4):271–279
Crémieux PY, Ledoux S, Clerici C, Cremieux F, Buessing M (2010) The impact of bariatric surgery on comorbidities and medication use among obese patients. Obes Surg 20(7):861–870
Makary MA, Clark JM, Shore AD, Magnuson TH, Richards T, Bass EB et al (2010) Medication utilization and annual health care costs in patients with type 2 diabetes mellitus before and after bariatric surgery. Arch Surg 145(8):726–731
Keating CL, Peeters A, Swinburn BA, Carter R, Moodie ML (2013) Pharmaceutical utilisation and costs before and after bariatric surgery. Int J Obes (Lond) 37(11):1467–1472
Alsuhibani A, Albogami Y, Diaby V, Friedman J, Vouri SM (2021) Evaluation of statin discontinuation stratified by primary versus secondary prevention following bariatric surgery: a retrospective cohort study. Surg Obes Relat Dis 17(5):939–946
Maciejewski ML, Livingston EH, Kahwati LC, Henderson WG, Kavee AL, Arterburn DE (2010) Discontinuation of diabetes and lipid-lowering medications after bariatric surgery at Veterans Affairs medical centers. Surg Obes Relat Dis 6(6):601–607
Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE et al (2012) Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 366(17):1567–1576
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS et al (2019) 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: a Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 73(24):e285–e350
Chang P, Friedenberg F (2014) Obesity and GERD. Gastroenterol Clin N Am 43(1):161–173
King WC, Chen JY, Belle SH, Courcoulas AP, Dakin GF, Flum DR et al (2017) Use of prescribed opioids before and after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis 13(8):1337–1346
Raebel MA, Newcomer SR, Reifler LM, Boudreau D, Elliott TE, DeBar L et al (2013) Chronic use of opioid medications before and after bariatric surgery. JAMA 310(13):1369–1376
Tian C, Maeda A, Okrainec A, Anvari M, Jackson T (2020) Impact of preoperative opioid use on health outcomes after bariatric surgery. Surg Obes Relat Dis 16(6):768–776
Ehlers AP, Sullivan KM, Stadeli KM, Monu JI, Chen-Meekin JY, Khandelwal S (2020) Opioid use following bariatric surgery: results of a prospective survey. Obes Surg 30(3):1032–1037
Hill MV, McMahon ML, Stucke RS, Barth RJ Jr (2017) Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg 265(4):709–714
Johannesdottir SA, Mægbæk ML, Hansen JG, Lash TL, Pedersen L, Ehrenstein V (2012) Correspondence between general practitioner-reported medication use and timing of prescription dispensation. Clin Epidemiol 4:13–18
Keating CL, Moodie ML, Bulfone L, Swinburn BA, Stevenson CE, Peeters A (2012) Healthcare utilization and costs in severely obese subjects before bariatric surgery. Obesity (Silver Spring) 20(12):2412–2419
Monk JS Jr, Dia Nagib N, Stehr W (2004) Pharmaceutical savings after gastric bypass surgery. Obes Surg 14(1):13–15
Narbro K, Agren G, Jonsson E, Näslund I, Sjöström L, Peltonen M (2002) Pharmaceutical costs in obese individuals: comparison with a randomly selected population sample and long-term changes after conventional and surgical treatment: the SOS intervention study. Arch Intern Med 162(18):2061–2069
Nguyen NT, Varela JE, Sabio A, Naim J, Stamos M, Wilson SE (2006) Reduction in prescription medication costs after laparoscopic gastric bypass. Am Surg 72(10):853–856
Weiner JP, Goodwin SM, Chang HY, Bolen SD, Richards TM, Johns RA et al (2013) Impact of bariatric surgery on health care costs of obese persons: a 6-year follow-up of surgical and comparison cohorts using health plan data. JAMA Surg 148(6):555–562
Sharples AJQ, Mullan M, Hardy K, Vergis A (2019) Effect of Roux-en-Y gastric bypass on pharmacologic dependence in obese patients with type 2 diabetes. Can J Surg 62(4):259–264
Acknowledgements
This research project was funded by a GFT (Geographical Full Time) grant provided by the University of Manitoba (UM 323268). The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Manitoba Population Research Data Repository under project # 2021-002 (HIPC # 2020/2021-18). The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy or Manitoba Health is intended or should be inferred. Data used in this study are from the Manitoba Population Research Data Repository housed at the Manitoba Centre for Health Policy, University of Manitoba and were derived from data provided by Manitoba Health.
Funding
This research project was funded by a GFT (Geographical Full Time) grant provided by the University of Manitoba (UM 323268).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ashley Vergis is a hernia proctor for Becton Dickinson. Ted Chia Hao Wu, Wenjing He, Isuru Dharmasena, Heather J Prior, Krista Hardy has no disclosure or conflicts of interests. The authors have no disclosures or conflicts of interests related to the results in this publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wu, T.C.H., He, W., Dharmasena, I. et al. Prescription drug usage as measure of comorbidity resolution after bariatric surgery: a population-based cohort study. Surg Endosc 37, 8601–8610 (2023). https://doi.org/10.1007/s00464-023-10294-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10294-5