Abstract
Introduction
Minimally invasive surgery (MIS) fellowship is one of the most popular fellowship programs, but little is known about the individual fellow’s clinical experience. Our goal was to determine the differences in case volume and case type in academic and community programs.
Methods
A retrospective review of advanced gastrointestinal, MIS, foregut, or bariatric fellowship cases logged into the Fellowship Council directory of fellowships during the 2020 and 2021 academic years included for analysis. The final cohort included 57,324 cases from all fellowship programs, that list data on the Fellowship Council website, including 58 academic programs and 62 community-based programs. All comparisons between groups were completed using Student’s t-test.
Results
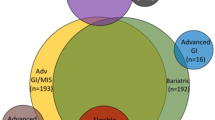
The mean number of cases logged during a fellowship year was 477.7 ± 149.9 with similar case numbers in academic and community programs, 462.5 ± 115.0 and 491.9 ± 176.2 respectively (p = 0.28). The mean data is illustrated in Fig. 1. The most common performed cases were in the following categories: bariatric surgery (149.8 ± 86.9 cases), endoscopy (111.1 ± 86.4 cases), hernia (68.0 ± 57.7 cases) and foregut (62.8 ± 37.3 cases). In these case-type categories, no significant differences in case volume were found between academic and community-based MIS fellowship programs. However, community-based programs had significantly more case experience compared to academic programs in all of the less commonly performed case-type categories: appendix 7.8 ± 12.8 vs 4.6 ± 5.1 cases (p = 0.08), colon 16.1 ± 20.7 vs 6.8 ± 11.7 cases (p = 0.003), hepato-pancreatic-biliary 46.9 ± 50.8 vs 32.5 ± 18.5 cases (p = 0.04), peritoneum 11.7 ± 16.0 vs 7.0 ± 7.6 cases (p = 0.04), and small bowel 11.9 ± 9.6 vs 8.8 ± 5.9 cases (p = 0.03).
Conclusion
MIS fellowship has been a well-established fellowship program under the Fellowship Council guideline. In our study, we aimed to identify the categories of fellowship training and the perspective case volumes in academic vs community setting. We conclude that fellowship training experience is similar in case volumes of commonly performed cases when comparing academic and community programs. However, there is substantial variability in the operative experience among MIS fellowship programs. Further study is necessary to identify the quality of fellowship training experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Minimally invasive surgery (MIS) fellowship was popularized in the early 1990’s. At the time, there was a true need for advanced training in emerging laparoscopic technology, as residency did not provide sufficient training experience. Thirty years later, MIS remains one of the most popular fellowships, with nearly 200 training positions available on an annual basis [1]. In fact, only surgical critical care has more fellowship positions on an annual basis. Despite this numeric dominance, MIS fellowships have had relatively little independent analysis. For instance, a simple search of Pubmed shows triple the number of articles on “critical care fellowship” than “minimally invasive surgery fellowship” (394 versus 134).
The Fellowship Council serves as the organizing body for the fellowship match, as well as the accrediting body for fellowship programs (www.fellowshipcouncil.org). Requirements for fellowship are broad and inclusive, due to the fact that some fellowships may specialize in one particular aspect of minimally invasive surgery. The actual title of the Fellowship Council directory is as follows: “Advanced GI MIS, Bariatrics, Complex gastrointestinal surgery, comprehensive flexible endoscopy, foregut, and HPB.” In an of itself, this speaks to the wide variability of fellowships that come under the “MIS” umbrella. Individual fellows are able to achieve a certificate from the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) [2]. Recently, SAGES has proposed new guidelines for fellowship defined categories [3]. However, the implementation of these guidelines may have been hampered by declining volumes of elective surgery during the COVID-19 pandemic.
Our goal was to help define the average experience among current MIS fellows. We reviewed publicly available data to the determine the spectrum of clinical experience in MIS fellowship programs during the pandemic. Specifically, we reviewed the differences in case volume and case type in academic and community programs.
Methods
We accessed the Fellowship Council directory of fellowships (www.fellowshipcouncil.org) on July 1, 2022. As the dataset was publicly available and not specifically identifiable on the level of the individual fellow, the study did not require IRB approval. All fellowships that were advanced gastrointestinal, MIS, foregut, or bariatric were included for analysis. Programs that were listed as “flexible endoscopy” (n = 3) were predominantly ERCP, and were excluded. Programs that were self-described as hepato-pancreatic-biliary did not specify a minimally invasive focus and were also excluded. After review of the 132 individual programs, those that did not include specific case information for both years (n = 7) were excluded, yielding a final cohort of 120 programs This included 58 academic programs and 62 community programs. The 57,324 cases logged in these programs during the 2020 and 2021 academic years were used in this analysis.
All data was entered into an Excel database. Statistical analysis was performed using SAS 9.4 was used for all data management and statistical analysis. The student's t-test assessed the association between independent groups. Statistical significance was defined as α < 0.05, with all p-values reported as two-tailed. Data are expressed as a mean and standard deviation.
Results
The mean number of cases logged during a fellowship year was 477.7 ± 149.9 with similar case numbers in academic and community programs, 462.5 ± 115.0 and 491.9 ± 176.2 respectively (p = 0.28). The overall distribution of logged cases is seen in Fig. 1. The most common performed cases were in the following categories: bariatric surgery (149.8 ± 86.9 cases), endoscopy (111.1 ± 86.4 cases), hernia (68.0 ± 57.7 cases) and foregut (62.8 ± 37.3 cases). In these commonly performed case categories, there were no significant differences in case volume between academic and community MIS fellowship programs (Table 1). However, community MIS fellows had significantly more case experience than academic MIS fellows in all of the less commonly performed case categories—specifically appendix, colon, hepatico-pancreatic-biliary, peritoneum and small bowel, 7.8 ± 12.8 vs 4.6 ± 5.1 cases (p = 0.08), 16.1 ± 20.7 vs 6.8 ± 11.7 cases (p = 0.003), 46.9 ± 50.8 vs 32.5 ± 18.5 cases (p = 0.04), 11.7 ± 16.0 vs 7.0 ± 7.6 cases (p = 0.04), 11.9 ± 9.6 vs 8.8 ± 5.9 cases (p = 0.03), respectively.
Discussion
Despite the prevalence of MIS fellowships, relatively little information has been published in scholarly journals. Previous work has shown that MIS fellowship may lead to increased confidence [4] and that a majority of fellowship graduates would recommend their former fellowship [5]. However, specific data about fellow experience has not been well collated, and there is a real question that completing “MIS fellowship” actually results in a uniform product. Our analysis suggests that umbrella term “MIS fellowship” does indeed cover a surprisingly varied experience.
During the past two years, MIS fellows logged a substantial operative experience, despite the pandemic. The majority of MIS cases are elective, but there was no specific information available on the percentage of elective versus emergent cases in this sample. In general, case volumes at academic medical centers were lower than at community-based training programs. These differences were significant only in low-volume case-type categories: appendix, colon, hepatico-pancreatic-biliary, peritoneum, small bowel. The differences were not significantly different in the case-type categories (bariatric, foregut, hernia) used by the Fellowship Council. Moreover, all case-type categories had high standard deviations (~ 50–80% of the mean) suggesting large case volume variability between programs. There may be research or teaching expectations at an academic medical center that is not present in the community setting, but the impact on case volumes is purely speculative.
In this database analysis, robotic surgery is not specified in the existing reporting structure. There were no definitive case numbers provided by the programs, and little in the qualitative description that provided specific information. Any comment on robotic surgery, which may have increasing relevance to MIS training, is purely speculative.
In any training program, autonomy is a key concept [6]. Autonomy is probably more of a factor in fellowship than in more junior levels of training, as the goal is to produce an independent, competent specialist. It is possible that a fellowship program may be more observational than participatory, but there is no record from any program of the percent of the case that the fellow does, or the individual critical moves of any procedure.
Our study has limitations related to the available data and to our method of analysis. First, case-type categories provide no measure of case complexity. The impact of case complexity on training is not well understood but may change the quality of the training experience. Second, procedures can be double counted, specifically components of a single case (e.g., a gastric bypass and an intraoperative endoscopy completed during the same gastric bypass) can be logged into different categories. This may suggest a more substantial experience than the fellow might actually receive. Some programs may have more than one fellow, and we cannot determine how uniform the experience is between fellows at a multi-fellow program, or between those fellows and those at a single-fellow program. We compared the aggregate data of academic and community-based MIS fellowship programs. The high standard deviations found in all the case-type categories suggests the training experience of the individual fellow vary not only by case volumes, but also by case-type distribution. Last, the time interval of the data includes the global pandemic, and it may represent an atypical pattern of cases compared to historical standards. However, it does reflect the current state of MIS fellow training.
Conclusions
MIS fellowship has been a well-established fellowship program under the Fellowship Council and SAGES guidelines. In our review of the data, fellowship training experience is similar in case volumes of commonly performed cases when comparing academic and community programs. Further study is necessary to identify the quality of fellowship training experience. Robotic assisted laparoscopic experience in the different fellowship program should be evaluated.
References
Shockcor N, Hayssen H, Kligman MD, Kubicki NS, Kavic SM (2021) Ten year trends in minimally invasive surgery fellowship. JSLS 25:1–5
Weis JJ, Gee D, Honigsberg E, Goldblatt M, Pryor A, Scott DJ (2022) SAGES advanced GI/MIS certificate program. Surg Endosc 36:1–5
Weis JJ, Goldblatt M, Pryor A, Dunkin BJ, Brunt LM, Jones DB, Scott DJ (2018) SAGES’s advanced GI/MIS fellowship curriculum pilot project. Surg Endosc 32:2613–2619
Park A, Kavic SM, Lee TH, Heniford BT (2007) Minimally invasive surgery: the evolution of fellowship. Surgery 142:505–511
Grover BT, Kothari SN, Kallies KJ, Mathiason MA (2009) Benefits of laparoscopic fellowship training: a survey of former fellows. Surg Innov 16:283–288
The Fellowship Council: directory of fellowships. https://fellowshipcouncil.org/directory-of-fellowships. Accessed July 13, 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Delandy McConnell, Ace St. John, Mark D. Kligman, and Stephen M. Kavic, has no conflicts of interest, or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McConnell, D., John, A.S., Kligman, M.D. et al. What is MIS fellowship? Community and academic program experience. Surg Endosc 37, 4623–4626 (2023). https://doi.org/10.1007/s00464-023-09958-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09958-z