Abstract
Background
Proficiency of the operating surgeon is one of the most critical factors potentially associated with reductions in complications and surgery-related mortality. With video-rating systems having shown potential for assessing laparoscopic surgeons’ proficiency, the Endoscopic Surgical Skill Qualification System (ESSQS) was developed by the Japan Society for Endoscopic Surgery to subjectively assess the proficiency of laparoscopic surgeons by rating applicants’ non-edited case videos. We conducted a study to evaluate how ESSQS skill-qualified (SQ) surgeon involvement influences short-term outcomes of laparoscopic gastrectomy performed for gastric cancer.
Methods
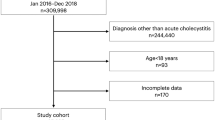
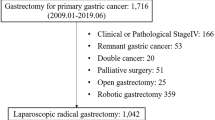
Data from the National Clinical Database regarding laparoscopic distal and total gastrectomy performed for gastric cancer between January 2016 and December 2018 were analyzed. Operative mortality, defined as 30-day mortality or 90-day in-hospital mortality, and anastomotic leakage rates were compared per involvement vs. non-involvement of an SQ surgeon. Outcomes were also compared per involvement of a gastrectomy-, colectomy-, or cholecystectomy-qualified surgeon. The association between the area of qualification and operative mortality/anastomotic leakage was also analyzed with a generalized estimating equation logistic regression model used to account for patient-level risk factors and institutional differences.
Results
Of 104,093 laparoscopic distal gastrectomies, 52,143 were suitable for inclusion in the study; 30,366 (58.2%) were performed by an SQ surgeon. Of 43,978 laparoscopic total gastrectomies, 10,326 were suitable for inclusion; 6501 (63.0%) were performed by an SQ surgeon. Gastrectomy-qualified surgeons outperformed non-SQ surgeons in terms of both operative mortality and anastomotic leakage. They also outperformed cholecystectomy- and colectomy-qualified surgeons in terms of operative mortality or anastomotic leakage in distal and total gastrectomy, respectively.
Conclusion
The ESSQS appears to discriminate laparoscopic surgeons who can be expected to achieve significantly improved gastrectomy outcomes.


Similar content being viewed by others
References
Mackenzie H, Dixon A (2014) Proficiency gain curve and predictors of outcome for laparoscopic ventral mesh rectopexy. Surgery 156:158–167
Twijnstra AR, Blikkendaal MD, van Zwet EW, van Kesteren PJM, de Kroon CD, Jansen FW (2012) Predictors of successful surgical outcome in laparoscopic hysterectomy. Obstet Gynecol 119:700–708
Yamakawa T, Kimura T, Matsuda T, Konishi F, Bandai Y (2013) Endoscopic Surgical Skill Qualification System (ESSQS) of the Japanese Society of Endoscopic Surgery (JSES). BH Surg 3:6–8
Mori T, Kimura T, Kitajima M (2010) Skill accreditation system for laparoscopic gastro-enterologic surgeons in Japan. Minim Invasive Ther Allied Technol 19:18–23
Kimura T, Mori T, Konishi F, Kitajima M (2010) Endoscopic Surgical Skill Qualification System in Japan: five years of experience in the gastrointestinal field. Asian J Endosc Surg 3:66–70
Mori T, Endo H, Misawa T, Yamaguchi S, Sakamoto Y, Inomata M, Sakai Y, Kakeji Y, Miyata H, Kitagawa Y, Watanabe M (2022) Involvement of a skill-qualified surgeon favorably influences outcomes of laparoscopic cholecystectomy performed for acute cholecystitis. Surg Endosc 36:5956–5963
Etoh T, Honda M, Kumamaru H, Miyata H, Yoshida K, Kodera Y, Kakeji Y, Inomata M, Konno H, Seto Y, Kitano S, Hiki N (2018) Morbidity and mortality from a propensity score-matched, prospective cohort study of laparoscopic versus open total gastrectomy for gastric cancer: data from a nationwide web-based database. Surg Endosc 32:2766–2773
Matsubara N, Miyata H, Gotoh M, Tomita N, Baba H, Kimura W, Nakagoe T, Simada M, Kitagawa Y, Sugihara K, Mori M (2014) Mortality after common rectal surgery in Japan: a study on low anterior resection from a newly established nationwide large-scale clinical database. Dis Colon Rectum 57:1075–1081
Kurita N, Miyata H, Gotoh M, Shimada M, Imura S, Kimura W, Tomita N, Baba H, Kitagawa Y, Sugihara K, Mori M (2015) Risk model for distal gastrectomy when treating gastric cancer on the basis of data from 33,917 Japanese patients collected using a national wide web-based data entry system. Ann Surg 262:295–303
Watanabe M, Miyata H, Gotoh M, Baba H, Kimura W, Tomita N, Nakagoe T, Shimada M, Kitagawa Y, Sugihara K, Mori M (2014) Total gastrectomy risk model: data from 20,011 Japanese patients in a nationwide internet-based database. Ann Surg 260:1034–1039
Kunisaki C, Miyata H, Konno H, Saze Z, Hirahara N, Kikuchi H, Wakabayashi G, Gotoh M, Mori M (2017) Modeling preoperative risk factors for potentially lethal morbidities using a nationwide Japanese web-based database of patients undergoing distal gastrectomy for gastric cancer. Gastric Cancer 20:496–507
Akaike H, Kawaguchi Y, Shiraishi K, Shimizu H, Furuya S, Hosomura N, Amemiya H, Kawaida H, Sudoh M, Inoue S, Kohno H, Ichikawa D (2019) Validity of additional surgical resection by comparing the operative risk with the stratified lymph node metastatic risk in patients with early gastric cancer after endoscopic submucosal dissection. World J Surg Oncol 17:136
Iwatsuki M, Yamamoto H, Miyata H, Kakeji Y, Yoshida K, Konno H, Seto Y, Baba H (2021) Association of surgeon and hospital volume with postoperative mortality after total gastrectomy for gastric cancer: data from 71,307 Japanese patients collected from a nationwide web-based data entry system. Gastric Cancer 24:526–534
Gotoh M, Miyata H, Hashimoto H, Wakabayashi G, Konno H, Miyakawa S, Sugihara K, Mori M, Satomi S, Kokudo N, Iwanaka T (2016) National Clinical Database feedback implementation for quality improvement of cancer treatment in Japan: from good to great through transparency. Surg Today 46:38–47
Birkmeyer JD, Finks JF, O’Reilly A, Oerline M, Carlin AM, Nunn AR, Dimick J, Banerjee M, Birkmeyer NJ, Michigan Bariatric Surgery Collaborative (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369:1434–1442
Collins JW, Sridhar A, Kelly J (2020) Surgical training benefits from the cumulative outcomes of proficiency-based training and mentorship. JAMA Surg 155:616
Okamura A, Watanabe M, Fukudome I, Yamashita K, Yuda M, Hayami M, Imamura Y, Mine S, Surgical team proficiency in minima et al (2018) Surgical team proficiency in minimally invasive esophagectomy is related to case volume and improves patient outcomes. Esophagus 15:115–121
Aydın A, Ahmed K, Abe T, Raison N, Hemelrijck MV, Garmo H, Ahmed HU, Mukhtar F, Al-Jabir A, Brunckhorst O, Shinohara N, Zhu W, Zeng G, Sfakianos JP, Gupta M, Tewari A, Gözen AS, Rassweiler J, Skolarikos A, Kunit T, Knoll T, Moltzahn F, Thalmann GN, Lantz Powers AG, Chew BH, Sarica K, Shamim Khan M, Dasgupta P, SIMULATE Trial Group (2022) Effect of simulation-based training on surgical proficiency and patient outcomes: a randomised controlled clinical and educational trial. Eur Urol 81:385–393
Varban OA, Thumma JR, Finks JF, Carlin AM, Ghaferi AA, Dimick JB (2021) Evaluating the effect of surgical skill on outcomes for laparoscopic sleeve gastrectomy: a video-based study. Ann Surg 273:766–771
Varban OA, Thumma JR, Carlin AM, Carlin AM, Ghaferi AA, Dimick JB (2020) Peer assessment of operative videos with sleeve gastrectomy to determine optimal operative technique. J Am Coll Surg 231:470–477
Livingston EH (2010) Relationship between surgeon volume and adverse outcomes after Roux-en-Y gastric bypass in Longitudinal Assessment of Bariatric Surgery (LABS) study. Surg Obes Relat Dis 6:587–588
Hannan EL, Radzyner M, Rubin D, Dougherty J, Brennan MF (2002) The influence of hospital and surgeon volume on in-hospital mortality for colectomy, gastrectomy, and lung lobectomy in patients with cancer. Surgery 131:6–15
Begg CB, Cramer LD, Hoskins WJ, Brennan MF (1998) Impact of hospital volume on operative mortality for major cancer surgery. JAMA 280:1747–1751
Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A (2000) Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA 283:1159–1166
Halm EA, Lee C, Chassin MR (2002) Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med 137:511–520
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL (2003) Surgeon volume and operative mortality in the United States. N Engl J Med 349:2117–2127
Berardi G, Aghayan D, Fretland ÅA, Elberm H, Cipriani F, Spagnoli A, Montalti R, Ceelen WP, Aldrighetti L, Abu Hilal M, Edwin B, Troisi RI (2019) Multicentre analysis of the learning curve for laparoscopic liver resection of the posterosuperior segments. Br J Surg 106:1512–1522
Finks JF, Carlin A, Share D, O’Reilly A, Fan Z, Birkmeyer J, Birkmeyer J, Michigan Bariatric Surgery Collaborative from the Michigan Surgical Collaborative for Outcomes Research Evaluation (2011) Effect of surgical techniques on clinical outcomes after laparoscopic gastric bypass—results from the Michigan Bariatric Surgery Collaborative. Surg Obes Relat Dis 7:284–289
Funding
There are no sources of funding for this research and its publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Hideki Endo and Hiroyuki Yamamoto, who are affiliated with the Department of Healthcare Quality Assessment, Graduate School of Medicine, the University of Tokyo, receive endowments from the National Clinical Database, Johnson & Johnson K.K., and Nipro Corporation. Dr. Hiroyuki Yamamoto has received consulting fees from Mitsubishi Tanabe Pharma Corporation; received honoraria for his lectures from Chugai Pharmaceutical Co., Ltd. and Ono Pharmaceutical Co., Ltd.; and received payment for writing a manuscript from Astellas Pharma, Inc. Dr. Yuko Kitagawa is affiliated with Keio University School of Medicine, which has received grants from Asahi Kasei Pharma Corporation, Ono Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Factory Inc., Nippon Covidien Inc., Taiho Pharmaceutical Co., Ltd., Chugai Pharmaceutical Co., Ltd., Kaken Pharmaceutical Co., Ltd., Yakult Honsha Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Tsumura & Co., Sumitomo Pharma Co., Ltd., EA Pharma Co., Ltd., Eisai Co., Ltd., Kyowa Kirin Co., Ltd., Medicon Inc., Takeda Pharmaceutical Co., Ltd., and Teijin Pharma Limited. Dr. Yuko Kitagawa has received honoraria from Chugai Pharmaceutical Co., Ltd., Taiho Pharmaceutical Co., Ltd., Asahi Kasei Pharma Corporation, Otsuka Pharmaceutical Factory Inc., Shionogi & Co., Ltd., Nippon Covidien Inc., Ethicon, Inc., Ono Pharmaceutical Co., Ltd., Olympus Corporation, Bristol-Myers Squibb K.K., AstraZeneca K.K., MSD K.K., Smith & Nephew K.K., Kaken Pharmaceutical Co., Ltd., ASKA Pharmaceutical Co., Ltd., Miyarisan Pharmaceutical Co., Ltd., Toray Industries, Inc., Daiichi Sankyo Company, Limited, Chugai Foundation for Innovative Drug Discovery Science, Nippon Kayaku Co., Ltd., EA Pharma Co., Ltd., Intuitive Surgical G.K., and Takeda Pharmaceutical Co., Ltd. Dr. Hiroaki Miyata has received provision of materials from the National Clinical Database, Johnson & Johnson K.K., Nipro Corporation, and Intuitive Surgical Sàrl. Dr. Masafumi Inomata has received honoraria from Olympus Co. Ltd., Medtronic Co. Ltd., and Johnson & Johnson K.K. Drs. Takeyuki Misawa, Toshiyuki Mori, Shigeki Yamaguchi, Yoshiharu Sakai, and Yoshihiro Kakeji have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Misawa, T., Endo, H., Mori, T. et al. Skill-qualified surgeons positively affect short-term outcomes after laparoscopic gastrectomy for gastric cancer: a survey of the National Clinical Database of Japan. Surg Endosc 37, 4627–4640 (2023). https://doi.org/10.1007/s00464-023-09950-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09950-7