Abstract
Objective
The Endoscopic Surgical Skill Qualification System (ESSQS) was developed by the Japan Society for Endoscopic Surgery as a means of subjectively assessing the proficiency of laparoscopic surgeons. We conducted a study to evaluate how involvement of an ESSQS skill-qualified (SQ) surgeon influences short-term outcomes of laparoscopic cholecystectomy performed for acute cholecystitis.
Summary of background data
Previous reports suggest that assessment of the video-rating system is a potential tool to discriminate laparoscopic surgeons’ proficiency and top-rated surgeons face less surgical mortality and morbidity in bariatric surgery.
Methods
Data from the National Clinical Database regarding laparoscopic cholecystectomy performed for acute cholecystitis between January 2016 and December 2018 were analyzed. Outcomes were compared between patients grouped according to involvement vs. non-involvement of an SQ surgeon. Outcomes were also compared between patients grouped according to whether their operation was performed by biliary tract-, stomach-, or colon-qualified surgeon.
Results
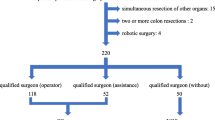
Of the 309,998 laparoscopic cholecystectomies during the study period, 65,295 were suitable for inclusion in the study and 13,670 (20.9%) were performed by an SQ surgeon. Patients’ clinical characteristics did not differ between groups. Thirty-day mortality was significantly lower in the SQ group (0.1%) 16/13,670 than in the non-SQ group (0.2%) 140/51,625 (P = 0.001). Thirty-day mortality was [0.1% (9/7173)] in the biliary tract-qualified group, [0.2% (5/3527)] in the stomach-qualified group, and [0.1% (2/3240)] in the colon-qualified group.
Conclusion
Surgeons with ESSQS certification outperform the non-skilled surgeons in terms of surgical mortality in 30 and 90 days. Further verification of the value of the ESSQS is warranted and similar systems may be needed in countries across the world to ensure patient safety and control the quality of surgical treatments.

Similar content being viewed by others
Abbreviations
- JSES:
-
Japan Society for Endoscopic Surgery
- ESSQS:
-
Endoscopic Surgical Skill Qualification System
- SQ:
-
Skill-qualified
References
Mackenzie H, Dixon A (2014) Proficiency gain curve and predictors of outcome for laparoscopic ventral mesh rectopexy. Surgery 156:158–167
Twijnstra A, Blikkendaal M, van Zwet E et al (2012) Predictors of successful surgical outcome in laparoscopic hysterectomy. Obstet Gynecol 119:700–708
Yamakawa T, Kimura T, Matsuda T et al (2013) Endoscopic surgical skill qualification system (ESSQS) of the Japanese Society of Endoscopic Surgery (JSES). BH Surg 3:6–8
Mori T, Kimura T, Kitajima M (2010) Skill accreditation system for laparoscopic gastroenterologic surgeons in Japan. Minim Invasive Ther Allied Technol 19:18–23
Kimura T, Mori T, Konishi F et al (2010) Endoscopic surgical skill qualification system in Japan: five years of experience in the gastrointestinal field. Asian J Endosc Surg 3:66–70
Etoh T, Honda M, Kumamaru H et al (2018) Morbidity and mortality from a propensity score-matched, prospective cohort study of laparoscopic versus open total gastrectomy for gastric cancer: data from a nationwide web-based database. Surg Endosc 32:2766–2773
Matsubara N, Miyata H, Gotoh M et al (2014) Mortality after common rectal surgery in Japan: a study on low anterior resection from a newly established nationwide large-scale clinical database. Dis Colon Rectum 57:1075–1081
Birkmeyer JD, Finks JF, O’Reilly A et al (2013) Surgical skill and complication rates after bariatric surgery. N Engl J Med 369:1434–1442
Paydar S, Ghahrmani Z, Bolandparvaz S et al (2014) Learning operational strategies in surgery training. J Adv Med Educ Prof 2:92–94
Spruit E, Guido P, Band G et al (2014) Optimal training design for procedural motor skills: a review and application to laparoscopic surgery. Psychol Res 78:878–891
Martin JA, Regehr G, Reznick R (1997) Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 84:273–278
Holden G, Flach J, Donchin Y (1999) Perceptual-motor coordination in an endoscopic surgery simulation. Surg Endosc 13:127–132
Papanikolaou G, Haidopoulos D, Paschopoulos M et al (2019) Changing the way we train surgeons in the 21st century: a narrative comparative review focused on box trainers and virtual reality simulators. Eur J Obstet Gynecol Reprod Biol 235:13–18
Fukuta A, Obata S, Jimbo T (2019) Continuous skill training using the disease-specific endoscopic surgical simulator to promote young pediatric surgeons: learning curve for trainees. J Laparoendosc Adv Surg Tech A 29:1334–1341
Balik E, Asoglu O, Saglam S et al (2010) Effects of surgical laparoscopic experience on the short-term postoperative outcome of rectal cancer: results of a high volume single center institution. Surg Laparosc Endosc Percutan Tech 20:93–99
Birmoeyer NJ, Stukel TA, Siewers AE et al (2003) Surgeon volume and operative mortality in the United States. N Engl J Med 349:2117–2127
Livingston EH (2010) Relationship between surgeon volume and adverse outcomes after Roux-en-Y gastric bypass in Longitudinal Assessment of Bariatric Surgery (LABS) study. Surg Obes Relat Dis 6:587–588
Birkmeyer J, Finks J, O’Reilly A et al (2013) Michigan Bariatric Surgery Collaborative. Surgical skill and complication rates after bariatric surgery. N Engl J Med 369:1434–1442
Varban O, Thumma J, Finks J et al (2019) Evaluating the effect of surgical skill on outcomes for laparoscopic sleeve gastrectomy: a video-based study. Ann Surg. https://doi.org/10.1097/SLA.0000000000003385
Sgaramella L, Gurrado A, Pasculli A et al (2020) The critical view of safety during laparoscopic cholecystectomy: Strasberg Yes or No? An Italian Multicentre study. Surg Endosc. https://doi.org/10.1007/s00464-020-07852-6
Kobayashi H, Miyata H, Gotoh M et al (2014) Risk model for right hemicolectomy based on 19,070 Japanese patients in the National Clinical Database. J Gastroenterol 49:1047–1055
Watanabe T, Miyata H, Konno H et al (2017) Prediction model for complications after low anterior resection based on data from 33,411 Japanese patients included in the National Clinical Database. Surgery 161:1597–1608
Jensen K, Roth N, Krarup PM et al (2019) Surgical management of acute cholecystitis in a Nationwide Danish Cohort. Langenbecks Arch Surg 404:589–597
Finks JF, Carlin A, Share D et al (2011) Michigan bariatric surgery collaborative from the Michigan Surgical Collaborative for Outcomes Research Evaluation. Effect of surgical techniques on clinical outcomes after laparoscopic gastric bypass--results from the Michigan Bariatric Surgery Collaborative. Surg Obes Relat Dis 7:284–289
Giger U, Michel JM, Opitz I et al (2006) (Swiss Association of Laparoscopic and Thoracoscopic Surgery (SALTS) Study Group). Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg 203:723–728
Rodríguez-Sanjuán J, Arruabarrena A, Sánchez-Moreno L et al (2012) Acute cholecystitis in high surgical risk patients: percutaneous cholecystostomy or emergency cholecystectomy? Am J Surg 204:54–59
Berardi G, Aghayan D, Fretland ÅA et al (2019) Multicentre analysis of the learning curve for laparoscopic liver resection of the posterosuperior segments. Br J Surg 106:1512–1522
Acknowledgements
This study was supported by the Japan Society for Endoscopic Surgery.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Toshiyuki Mori, Hideki Endo, Takeyuki Misawa, Shigeki Yamaguchi, Yoshihiro Sakamoto, Masafumi Inomata, Yoshiharu Sakai, Yoshihiro Kakeji, Hiroaki Miyata, Yuko Kitagawa, and Masahiko Watanabe have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mori, T., Endo, H., Misawa, T. et al. Involvement of a skill-qualified surgeon favorably influences outcomes of laparoscopic cholecystectomy performed for acute cholecystitis. Surg Endosc 36, 5956–5963 (2022). https://doi.org/10.1007/s00464-022-09045-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09045-9