Abstract
Background
Since 2012, Associating Liver Partition and Portal vein ligation for Staged hepatectomy (ALPPS) has encountered several modifications of its original technique. The primary endpoint of this study was to analyze the trend of ALPPS in Italy over a 10-year period. The secondary endpoint was to evaluate factors affecting the risk of morbidity/mortality/post-hepatectomy liver failure (PHLF).
Methods
Data of patients submitted to ALPPS between 2012 and 2021 were identified from the ALPPS Italian Registry and evaluation of time trends was performed.
Results
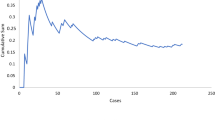
From 2012 to 2021, a total of 268 ALPPS were performed within 17 centers. The number of ALPPS divided by the total number of liver resections performed by each center slightly declined (APC = − 2.0%, p = 0.111). Minimally invasive (MI) approach significantly increased over the years (APC = + 49.5%, p = 0.002). According to multivariable analysis, MI completion of stage 1 was protective against 90-day mortality (OR = 0.05, p = 0.040) as well as enrollment within high-volume centers for liver surgery (OR = 0.32, p = 0.009). Use of interstage hepatobiliary scintigraphy (HBS) and biliary tumors were independent predictors of PHLF.
Conclusions
This national study showed that use of ALPPS only slightly declined over the years with an increased use of MI techniques, leading to lower 90-day mortality. PHLF still remains an open issue.




Similar content being viewed by others

Change history
11 May 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00464-023-10101-1
References
Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T, Goralcyk A, Hörbelt R, Kroemer A, Loss M, Rümmele P, Scherer MN, Padberg W, Königsrainer A, Lang H, Obed A, Schlitt HJ (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 255:405–414. https://doi.org/10.1097/SLA.0b013e31824856f5
De Santibañes E, Clavien PA (2012) Playing play-doh to prevent postoperative liver failure: the “aLPPS” approach. Ann Surg 255:415–417
Sandström P, Røsok BI, Sparrelid E, Larsen PN, Larsson AL, Lindell G, Schultz NA, Bjørnbeth BA, Isaksson B, Rizell M, Björnsson B (2018) ALPPS improves resectability compared with conventional two-stage hepatectomy in patients with advanced colorectal liver metastasis: results from a scandinavian multicenter randomized controlled trial (LIGRO Trial). Ann Surg 267:833–840. https://doi.org/10.1097/SLA.0000000000002511
Oldhafer KJ, Stavrou GA, Van Gulik TM, De Santibanes E, Malago M, Schadde E, Hernandez-Alejandro R, Kokudo N, Aloia TA, Abdalla E, Linecker M, Clavien PA (2016) ALPPS—where do we stand, where do we go? Eight recommendations from the first international expert meeting. Ann Surg 263:839–841. https://doi.org/10.1097/SLA.0000000000001633
Serenari M, Zanello M, Schadde E, Toschi E, Ratti F, Gringeri E, Masetti M, Cillo U, Aldrighetti L, Jovine E, Montalti R, Vivarelli M, Grazi GL, Vennarecci G, Ettorre GM, Massani M, Bassi N, Cotsoglou C, Mazzaferro V, Nardo B, Forchino F, Ferrero A, Gruttadauria S, Ercolani G, Pinna AD (2016) Importance of primary indication and liver function between stages: results of a multicenter Italian audit of ALPPS 2012–2014. HPB 18:419–427. https://doi.org/10.1016/j.hpb.2016.02.003
Serenari M, Ratti F, Zanello M, Guglielmo N, Mocchegiani F, Di Benedetto F, Nardo B, Mazzaferro V, Cillo U, Massani M, Colledan M, Dalla Valle R, Cescon M, Vivarelli M, Colasanti M, Ettorre GM, Aldrighetti L, Jovine E (2020) Minimally invasive stage 1 to protect against the risk of liver failure: results from the hepatocellular carcinoma series of the associating liver partition and portal vein ligation for staged hepatectomy Italian registry. J Laparoendosc Adv Surg Tech 30:1082–1089. https://doi.org/10.1089/lap.2020.0563
Clavien PA, Barkun J, De Oliveira ML, Vauthey JN, Dindo D, Schulick RD, De Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The clavien-dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, Koch M, Makuuchi M, Dematteo RP, Christophi C, Banting S, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greig P, Rees M, Yokoyama Y, Fan ST, Nimura Y, Figueras J, Capussotti L, Büchler MW, Weitz J (2011) Posthepatectomy liver failure: a definition and grading by the international study group of liver surgery (ISGLS). Surgery 149:713–724. https://doi.org/10.1016/j.surg.2010.10.001
Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, Hicks M, Alsfasser G, Lauwers G, Hawkins IF, Caridi J (2000) Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery 127:512–519. https://doi.org/10.1067/msy.2000.105294
Lemke AJ, Hosten N, Neumann K, Müller B, Neuhaus P, Felix R, Langer R (1997) CT-Volumetrie der Leber vor transplantation. RoFo Fortschritte auf dem Gebiete der Rontgenstrahlen und der Neuen Bildgeb Verfahren 166:18–23. https://doi.org/10.1055/s-2007-1015371
de Graaf W, van Lienden KP, Dinant S, Roelofs JJTH, Busch ORC, Gouma DJ, Bennink RJ, van Gulik TM (2010) Assessment of future remnant liver function using hepatobiliary scintigraphy in patients undergoing major liver resection. J Gastrointest Surg 14:369–378. https://doi.org/10.1007/s11605-009-1085-2
Zwart MJW, Görgec B, Arabiyat A, Nota CLM, van der Poel MJ, Fichtinger RS, Berrevoet F, van Dam RM, Aldrighetti L, Fuks D, Hoti E, Edwin B, Besselink MG, Abu Hilal M, Hagendoorn J, Swijnenburg RJ (2022) Pan-European survey on the implementation of robotic and laparoscopic minimally invasive liver surgery. HPB. https://doi.org/10.1016/j.hpb.2021.08.939
Torzilli G, Viganò L, Giuliante F, Pinna AD (2016) Liver surgery in Italy. Criteria to identify the hospital units and the tertiary referral centers entitled to perform it. Updates Surg 68:135–142. https://doi.org/10.1007/s13304-016-0373-0
Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, Soubrane O, Schnitzbauer AA, Raptis D, Tschuor C, Petrowsky H, De Santibanes E, Clavien PA, Abdalla E, Adam R, Alden D, Aldrighetti LA, De Paz EAP, Balzan S, Barkun J, Björnsson B, Castro-Benitez C, Brustia R, Chapman WC, Chardarov N, Chaychenko D, Cherqui D, Corradetti L, Croome K, Cugat E, Dong J, Donckier V, Doussot A, Enne M, Figueras J, Fonollosa EH, Gauzolino R, Gruenberger T, Keutgen XM, Koffron A, Kukudo N, Lendoire J, Li J, Lodge JPA, Logan S, Lorenzin D, Lucidi V, Lurje G, Masetti M, McCormack L, Montalti R, Nagino M, Nüssler N, Neuperlach K, Ortega-Deballon P, Pineda K, Pissanou T, Ratti F, Regimbeau JM, Rogiers X, Sakamoto Y, Sandström P, Santoyo J, Scatton O, Sergeant G, Serrablo A, Sharma D, Skipenko O, Solomonov E, Sparrelid E, Stojanovic S, Strassberg S, Torrenga H, Troisi R, Truant S, Vachharajani N, De Carvalho EV, Vibert E, Vicente E, Vivarelli M, Vyas S, Wen Z, Zheng W, Zhou J (2014) Early survival and safety of ALPPS first report of the international ALPPS registry. Ann Surg 260:829–838. https://doi.org/10.1097/SLA.0000000000000947
Schadde E, Raptis DA, Schnitzbauer AA, Ardiles V, Tschuor C, Lesurtel M, Abdalla EK, Hernandez-Alejandro R, Jovine E, Machado M, Malago M, Robles-Campos R, Petrowsky H, De SE, Clavien PA (2015) Prediction of mortality after ALPPS stage-1. Ann Surg 262:780–786. https://doi.org/10.1097/SLA.0000000000001450
de Santibañes E, Alvarez FA, Ardiles V, Pekolj J, de Santibañes M (2016) Inverting the ALPPS paradigm by minimizing first stage impact: the Mini-ALPPS technique. Langenbeck’s Arch Surg 401:557–563. https://doi.org/10.1007/s00423-016-1424-1
Serenari M, Collaud C, Alvarez FA, De Santibañes M, Giunta D, Pekolj J, Ardiles V, De Santibañes E (2018) Interstage assessment of remnant liver function in ALPPS using hepatobiliary scintigraphy: prediction of posthepatectomy liver failure and introduction of the HIBA index. Ann Surg 267:1141–1147. https://doi.org/10.1097/SLA.0000000000002150
Aldrighetti L, Ratti F, Cillo U, Ferrero A, Ettorre GM, Guglielmi A, Giuliante F, Calise F (2017) Diffusion, outcomes and implementation of minimally invasive liver surgery: a snapshot from the I Go MILS (Italian group of minimally invasive liver surgery) registry. Updates Surg 69:271–283. https://doi.org/10.1007/s13304-017-0489-x
Melandro F, Giovanardi F, Hassan R, Larghi Laureiro Z, Ferri F, Rossi M, Mennini G, Pawlik TM, Lai Q (2019) Minimally invasive approach in the setting of ALPPS procedure: a systematic review of the literature. J Gastrointest Surg 23:1917–1924
Michal K, Sau M, Tamara GMH, Long JR (2020) A better route to ALPPS: minimally invasive vs open ALPPS. Surg Endosc 34:2379–2389
MacHado MAC, Makdissi FF, Surjan RC (2012) Totally laparoscopic ALPPS is feasible and may be worthwhile. Ann Surg 256:1
Di Benedetto F, Assirati G, Magistri P (2020) Full robotic ALPPS for HCC with intrahepatic portal vein thrombosis. Int J Med Robot Comput Assist Surg. https://doi.org/10.1002/rcs.2087
Masetti M, Lombardi R, Romboli A, Jovine E (2020) Fully robotic ALPPS and simultaneous left colectomy for synchronous colorectal liver metastases. J Laparoendosc Adv Surg Tech. https://doi.org/10.1089/lap.2020.0589
Fiorentini G, Della Corte A, Ratti F, Cipriani F, Catena M, Gusmini S, De Cobelli F, Aldrighetti L (2021) The LiTOS hepatectomy: liver partitioning and total venous occlusion for staged hepatectomy. HPB. https://doi.org/10.1016/j.hpb.2021.08.688
Halls MC, Cipriani F, Berardi G, Barkhatov L, Lainas P, Alzoubi M, D’Hondt M, Rotellar F, Dagher I, Aldrighetti L, Troisi RI, Edwin B, Hilal MA (2017) Conversion for unfavorable intraoperative events results in significantly worst outcomes during laparoscopic liver resection: lessons learned from a multicenter review of 2861 cases. Ann Surg. https://doi.org/10.1097/SLA.0000000000002332
Ardito F, Famularo S, Aldrighetti L, Grazi GL, DallaValle R, Maestri M, Jovine E, Ruzzenente A, Baiocchi GL, Ercolani G, Griseri G, Frena A, Zanus G, Zimmitti G, Antonucci A, Crespi M, Memeo R, Romano F, Giuliante F (2020) The Impact of hospital volume on failure to rescue after liver resection for hepatocellular carcinoma: analysis from the HE.RC.O.LE.S. Italian Registry Ann Surg 272:840–846. https://doi.org/10.1097/SLA.0000000000004327
Serenari M, Lenzi J, Cucchetti A, Cipriani F, Donadon M, Ardito F, Fazio F, Nicolini D, Iaria M, Famularo S, Perri P, Ansaloni L, Zanello M, Lai Q, Conci S, Molfino S, Ferrari C, Germani P, Zago M, Romano M, Zimmitti G, Antonucci A, Fumagalli L, Troci A, Ferraro V, Memeo R, Crespi M, Chiarelli M, Ercolani G, Hilal MA, Zanus G, Pinotti E, Tarchi P, Griseri G, Baiocchi GL, Ruzzenente A, Rossi M, Jovine E, Maestri M, Grazi GL, Romano F, Dalla Valle R, Ravaioli M, Vivarelli M, Ferrero A, Giuliante F, Torzilli G, Aldrighetti L, Cescon M, on behalf of the HE.RC.O.LE.S. Group (2022) The effect of a liver transplant program on the outcomes of resectable hepatocellular carcinoma: a nationwide multicenter analysis. Ann Surg. https://doi.org/10.1097/SLA.0000000000005439
Balzano G, Guarneri G, Pecorelli N, Paiella S, Rancoita PMV, Bassi C, Falconi M (2020) Modelling centralization of pancreatic surgery in a nationwide analysis. Br J Surg. https://doi.org/10.1002/bjs.11716
Sparrelid E, Jonas E, Tzortzakakis A, Dahlén U, Murquist G, Brismar T, Axelsson R, Isaksson B (2017) Dynamic evaluation of liver volume and function in associating liver partition and portal vein ligation for staged hepatectomy. J Gastrointest Surg 21:967–974. https://doi.org/10.1007/s11605-017-3389-y
Serenari M, Bonatti C, Zanoni L, Peta G, Tabacchi E, Cucchetti A, Ravaioli M, Pettinato C, Bagni A, Siniscalchi A, D’Errico A, Golfieri R, Fanti S, Cescon M (2021) The role of hepatobiliary scintigraphy combined with spect/ct in predicting severity of liver failure before major hepatectomy: a single-center pilot study. Updates Surg 73:197–208. https://doi.org/10.1007/s13304-020-00907-2
Acknowledgements
ALPPS Italian Registry Collaborators Stefania Camagni (Unit of Hepato-biliary Surgery and Liver Transplantation, ASST Papa Giovanni XXIII, Bergamo, Italy), Fabio Forchino (Department of General and Oncological Surgery, Mauriziano Hospital “Umberto I”, Turin, Italy), Enrico Gringeri (Hepatobiliary and Liver Transplantation Unit, University of Padua, Padua, Italy), Salvatore Gruttadauria (Department for the Treatment and Study of Abdominal Diseases and Abdominal Transplantation, Istituto di Ricovero e Cura a Carattere Scientifico, Istituto Mediterraneo per i Trapianti e Terapie ad alta specializzazione, University of Pittsburgh Medical Center, Italy, Palermo, Italy), Paolo Magistri (Hepato-Pancreato-Biliary Surgery and Liver Transplantation Unit, University of Modena and Reggio Emilia, Modena, Italy), Bruno Nardo (General and Oncological Surgery Unit, Department of Surgery, Annunziata Hospital, Cosenza, Italy), Matteo Ravaioli (General Surgery and Transplant Unit, IRCCS, Azienda Ospedaliero-Universitaria di Bologna, Sant’Orsola-Malpighi Hospital, Bologna, Italy), Fabrizio Romano (School of Medicine and Surgery, University of Milano-Bicocca, San Gerardo Hospital, Monza, Italy), Maurizio Romano (Department of Surgical, Oncological and Gastroenterological Science, University of Padua; Hepatobiliary and Pancreatic Surgery Unit, Treviso Hospital, Italy), Andrea Scarinci (Division of Hepatobiliary pancreatic Unit, IRCCS, Regina Elena National Cancer Institute, Rome, Italy), Matteo Virdis (Department of Surgery, Division of HPB, General Surgery and Liver Transplantation, Fondazione IRCCS Istituto Nazionale Tumori di Milano, Milan, Italy), Giacomo Zanus (Department of Surgical, Oncological and Gastroenterological Science, University of Padua; Hepatobiliary and Pancreatic Surgery Unit, Treviso Hospital, Italy).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Dr. Matteo Serenari, Dr. Francesca Ratti, Dr. Nicola Guglielmo, Dr. Matteo Zanello, Prof. Federico Mocchegiani, Dr. Jacopo Lenzi, Prof. Michele Colledan, Prof. Vincenzo Mazzaferro, Prof. Umberto Cillo, Dott. Alessandro Ferrero, Prof. Matteo Cescon, Prof. Fabrizio Di Benedetto, Prof. Marco Massani, Prof. Gianluca Grazi, Prof. Raffaele Dalla Valle, Prof. Marco Vivarelli, Prof. Giuseppe Maria Ettorre, Prof. Luca Aldrighetti, Prof. Elio Jovine, Dr. Stefania Camagni, Dr. Fabio Forchino, Prof. Enrico Gringeri, Prof. Salvatore Gruttadauria, Dr. Paolo Magistri, Prof. Bruno Nardo, Prof. Matteo Ravaioli, Prof. Fabrizio Romano, Dr. Maurizio Romano, Dr. Andrea Scarinci, Dr. Matteo Virdis and Prof. Giacomo Zanus have no conficts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the ALPPS Italian Registry are listed in the acknowledgments.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Serenari, M., Ratti, F., Guglielmo, N. et al. Evolution of minimally invasive techniques and surgical outcomes of ALPPS in Italy: a comprehensive trend analysis over 10 years from a national prospective registry. Surg Endosc 37, 5285–5294 (2023). https://doi.org/10.1007/s00464-023-09937-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09937-4